Abstract
Data sources Cochrane Oral Health Trials Register, Cochrane Central Register of Controlled Trials, MEDLINE, Embase, CINAHL, Chinese Biomedical Literature Database, China National Infrastructure, US National Institutes of Health Ongoing Trials Registry, WHO Clinical Trials Registry, Sciencepaper Online, 19 Chinese dental and nursing journals. Reference lists of included studies were also screened.
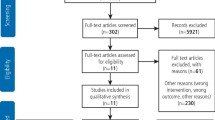
Study selection Studies were included if they explored oral care with the purpose of reducing pneumonia compared to no oral care, usual care or other oral care measures. Only randomised controlled trials were included which could be either parallel design or cluster RCTs with randomisation by care facility. No restrictions were placed on language, year of publication or publication status.
Data extraction and synthesis Two independent reviewers undertook screening for inclusion, data extraction and assessment of risk of bias. The Cochrane tool for risk of bias was used to assess quality of the studies. Synthesis was mainly narrative, though numerical results were combined where feasible.
Results Four studies were included, all of which were parallel RCTs. All were judged to be at high risk of bias due to lack of blinding. One study suggested that oral care may reduce pneumonia associated death, though evidence was low quality and should be treated with caution. There was no high quality evidence available to indicate which oral care methods may be most effective in reducing pneumonia.
Conclusions It was not possible to establish the effects of professional oral care on nursing home-acquired pneumonia due to the limited number of studies and low quality evidence. Further trials are needed to draw reliable conclusions.
Similar content being viewed by others
A Commentary on
Liu C, Cao Y, Lin J, Ng L, Needleman I, Walsh T, Li C.
Oral care measures for preventing nursing home-acquired pneumonia. Cochrane Database Syst Rev 2018; 9: Art. No. CD012416. DOI: 10.1002/14651858.CD012416.pub2

GRADE rating
Cochrane Reviews are regularly updated as new evidence emerges and in response to feedback, the Cochrane Library (www.thecochranelibrary.com) should be consulted for the most recent version of the review.
Commentary
Over the recent past, life expectancy in the UK has risen. As a population we are now living longer than ever before.1 This has given rise to an increase in the proportion of the adult population aged over 65 years old. In the UK this is 18.2% in 2017 and expected to rise to 24% by 2037.2 Healthy life expectancy (number of years lived in good health) has not increased at the same rate as life expectancy, leading to a significant proportion of our population living many years with ill health, multi-morbidity and frailty.1 It is estimated that between a quarter and a half of adults aged over 85 are considered medically 'frail' and this is associated with increased disability and crisis admissions to hospital.1Of these unplanned admissions to hospital, pneumonia is a common cause. The mortality rate of community-acquired pneumonia (which includes cases acquired in care homes) is between five and 14%, with around 50% of deaths from pneumonia occurring in those aged over 84.3 Links have been made between oral bacteria and community-acquired pneumonia, indeed one of the recognised complications of dysphagia is pneumonia, most likely arising from oral bacteria.4 Good oral care is thought to be a possible preventive measure for community-acquired pneumonia, especially for those adults living in supported care environments such as care homes.5 This Cochrane review aimed to examine the evidence base around whether oral care in care homes reduced the incidence of community-acquired pneumonia.
As expected from a Cochrane review, the methodology was well explained and robust. The review addressed a clear question and involved searches of multiple databases and trials registries. Only studies with a randomised control trial design were eligible for inclusion. The authors highlighted a difference in definition of the term 'randomised control trial' within Chinese literature and took additional steps to ensure that studies were only included where they were genuine RCTs. No restrictions were placed on language or year of publication.
No criteria were specified for participants within the included studies, allowing for inclusion of subjects of all ages and medical histories, with both dentate and edentulous individuals and patients receiving alternate feeding methods or mechanical ventilation. This broad range raises the possibility of variation in susceptibility to pneumonia among study subjects.
The definitions of the intervention 'professional oral care' and control 'usual oral care' were also broad and non-standard between included studies with no specification on who should perform the intervention or description of what procedures would be involved in either professional or usual oral care. In addition one of the included studies involved patients in the intervention group being fed in an upright position which may have influenced pneumonia risk independently of the enhanced oral care. None of the included studies compared professional oral care to no oral care, with all comparing against 'usual oral care'. It is likely that the standard of 'usual care' varied between studies.
Primary outcomes considered were: incidence (two studies), incidence proportion (three studies) or prevalence (zero studies) of nursing home-acquired pneumonia of any severity; pneumonia-associated mortality (three studies) and all-cause mortality (two studies). Only one study reported on adverse events of the intervention and none was found.
Only four studies were eligible for inclusion in the review, with all judged to be at high risk of bias due to lack of blinding. Most were however at low risk of other biases and it is unlikely to be possible to blind participants to the intervention in a study of this nature.
Synthesis was mainly presented in a narrative format, although pooling of results of three of the studies was undertaken for mortality due to pneumonia, with a Forrest plot included in the supplemental tables and figures. It was not felt appropriate to include results of the fourth study in pooling as it had been stopped early due to lack of evidence of an effect. Although methodology to test for heterogeneity between studies was described, there was no further discussion of whether this was undertaken.
The authors conclude that the findings may suggest that professional oral care could reduce mortality due to pneumonia, however due to the small number of studies and high risk of bias this should be interpreted with caution. It was not possible to identify which oral care procedures may be most effective in reducing the risk of nursing home-acquired pneumonia. The review highlights the need for further high quality studies in this area.
It is difficult therefore to be able to take away an actionable message for clinical care from this review. Although the findings were inconclusive around whether professional oral care in care homes reduces pneumonia rates, it does not negate the importance of oral health measures for other reasons. Prevention of oral disease is particularly important in this cohort of patients given the complexities of care for people with multiple co-morbidities, polypharmacy and capacity issues, needless to mention the importance of reducing pain, suffering and maintaining oral health related quality of life for all.
References
Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/535187/gs-16-10-future-of-an-ageing-population.pdf (accessed February 2019).
Available at https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/november2018 (accessed February 2019).
Available at https://www.nice.org.uk/guidance/cg191 (accessed February 2019).
Available at http://hub.careinspectorate.com/media/176816/nhs-caring-for-smiles.pdf (accessed February 2019).
Available at http://hub.careinspectorate.com/media/357290/nice_oral-health-for-adults-in-care-homes.pdf (accessed February 2019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muir, M., Burns, J. & McGoldrick, N. Oral care and nursing home-acquired pneumonia . Evid Based Dent 20, 14–15 (2019). https://doi.org/10.1038/s41432-019-0002-0
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-019-0002-0