Abstract
Expanded carrier screening (ECS) entails a screening offer for multiple recessive disorders at the same time, and allows testing of individuals or couples regardless of ancestry or geographic origin. Children of consanguineous couples have a higher-than-average risk of manifesting autosomal recessive disorders. This study aims to contribute to the responsible implementation of ECS for consanguineous couples. Seven semi-structured interviews were conducted with consanguineous couples who had recently participated in Whole Exome Sequencing (WES)-based ECS at Maastricht University Medical Center (MUMC+), the Netherlands. The test offered at MUMC+ covers a large number of disease-related genes (~2000), including severe, relatively mild, early- and late-onset disorders. Respondents were interviewed about their views on, and experiences with participation in WES-based ECS. Overall, participation was experienced as worthwhile: it enabled respondents to make informed choices with regard to family planning as well as to take on the presumed parental responsibility to deliver their children as healthy as possible. Furthermore, our findings suggest that (1) true consent for having this test requires timely information about the possible implications of a positive test result for specific categories of findings, as well as about the success rates of the available reproductive options; (2) the clinical geneticist can play a pivotal part in informing participants as well as providing clear information about autosomal recessive inheritance; (3) more research is needed to explore what type of genetic risk information is considered ‘meaningful’ by participants and actually contributes to reproductive decision-making.
Similar content being viewed by others
Introduction
Expanded carrier screening (ECS) entails a screening offer for a high number of autosomal (and sometimes X-linked) recessive disorders at the same time, and allows testing of individuals or couples regardless of ancestry or geographic origin. Although rare individually, it is estimated that one to two in 100 couples of the general population are at risk of having a child affected with a recessive disorder [1, 2]. Children of consanguineous couples have an additional risk of manifesting recessive disorders because of the expression of autosomal recessive gene mutations inherited from a common ancestor [3, 4]. This risk increases if partners have a closer biological relationship. First-degree cousins, for instance, are predicted to share 12.5% of their genes, meaning that on average, their progeny will be homozygous at 6.25% of gene loci. Offspring of second-degree cousins are expected to have children with 1.56% of their genome homozygous [5]. In a study by Sallevelt et al., a positive carrier couple status was found more frequently than expected also in more distantly related couples [6]. In genetic counselling, the risk of first-degree cousin couples of having affected children is generally presented as being 2–2.5% higher compared with nonconsanguineous couples [6]. However, recent studies suggest that the additional genetic risk associated with consanguinity may be substantially higher than previously thought [2, 6, 7].
Until recently, most consanguineous couples were referred to a clinical geneticist only after the birth of a child with an autosomal recessive disorder. ECS may provide consanguineous couples with information about previously unknown carrier status and contribute to autonomous reproductive decision making. If ECS is offered prior to pregnancy, couples have a wider range of reproductive choices than only prenatal diagnosis followed by a possible termination of pregnancy, including IVF followed by preimplantation genetic testing (PGT) for monogenic disorders. Other reproductive options include gamete donation, adoption, accepting the risk or refraining from having children. Carrier screening might also contribute to early therapeutic procedures in the neonatal period (or even prior to birth) for treatable conditions that require diagnosis ultimately in the first days of life, for instance medium-chain acyl-CoA dehydrogenase deficiency [8].
Recently, a whole-exome sequencing (WES)-based ECS test was designed, validated and diagnostically implemented for consanguineous couples at Maastricht University Medical Center (MUMC+), the Netherlands. In departure from recommendations from the European Society of Human Genetics (ESHG) to limit the scope of ECS to severe congenital or childhood-onset disorders, this test covers a large number of autosomal recessive disease-related genes (~2000), including relatively mild and late-onset disorders. The reason for doing so is that consanguineous couples may be at risk for any autosomal recessive disorder, including extremely rare ones that one would rather not risk missing by the use of predetermined filters. A recent publication about the yield of WES-based ECS as offered at MUMC+ showed that 28% of tested consanguineous couples carried (likely) pathogenic variants not previously known, the vast majority of which were indeed associated with serious disease, having impact on quality of life, causing impairment and/or requiring interventions, and with onset generally at infancy or early childhood [6].
In this paper, we report the experiences of a small number of consanguineous couples who had recently participated in WES-based ECS at the clinical genetics department of MUMC+. To date, only a few studies have explored the experiences, views and expectations of consanguineous couples in relation to ECS, notably Thain et al. [9]. Whereas the latter focussed on the experiences of couples who attended prenatal or preconception genetic counselling for consanguinity and their perspectives on self‐pay ECS for this indication, the respondents involved in our study already participated in WES-based ECS, and the majority were already enroled, or considering to enrol, in a PGT-trajectory. Moreover, in the Netherlands, the costs of ECS based on consanguinity are covered under national health insurance. However, because of required out-of-pocket expenses for healthcare services, couples may have to pay a personal contribution for participating in WES-based ECS. Our study aims to contribute to the literature on the responsible implementation of ECS as an offer to consanguineous couples. It will make an inventory of facilitators and barriers in the counselling trajectory and decision-making process with regard to participating in WES-based ECS and reproductive options after a positive test result. Our guiding question is: What are important points to consider in relation to a responsible offer of WES-based ECS to consanguineous couples?
Methods
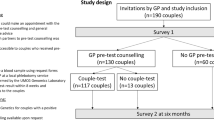
Study design
We used in-depth semi-structured interviews in order to gain a better understanding of the views and experiences of couples in relation to WES-based ECS. Moreover, this qualitative study design allowed us to investigate sensitive topics related to reproductive decision-making. This study received an ethics review waver under the Dutch Act on Research with Human Subjects by the Medical Ethics Committee of MUMC+. We obtained informed consent from all respondents prior to participation. All data were coded and stored in a protected database.
Setting
In the period January 2018 to December 2019, researchers from MUMC+ performed WES-based ECS in consanguineous and non-consanguineous couples as part of a pilot study after which a diagnostic preconception carrier test was implemented as a screening offer in clinical practice [6, 10]. WES data were filtered against a broad OMIM-based list of autosomal recessive diseases without stringent severity criteria. Only genes with unclear or very mild phenotypes were excluded. As consanguinity does not lead to an increased risk of manifesting X-linked disorders, these were not included in the screening panel. Variants were classified according to ACMG-guidelines and only class IV (likely pathogenic) and V (definitely pathogenic) variants, present in both partners, were included in the final diagnostic report. On average, participating couples had to wait three months for the test results. As only couple-based results have utility for reproductive decision-making, individual carrier status was not communicated with participating couples (for full details see Sallevelt et al. 2021 [6]).
Respondent recruitment
A purposive sample of study respondents was recruited by two clinical geneticists (SS, CdD) at the Department of Clinical Genetics of MUMC + . Couples were eligible to participate in this study if they had received genetic counselling because of consanguinity. Other inclusion criteria included mastery of the Dutch language and a minimum age of 18 years. During or sometime after preconception genetic counselling, a clinical geneticist informed potential respondents about the purpose of the study. Those who expressed interest to participate were contacted by researchers (SvdH and AW) via e-mail or telephone to arrange an interview. Important reasons for declining participation included lack of time or having to cope with already emotional personal situations related to positive carrier status and the care for, or loss of, an affected child. All couples or individual participants were reimbursed 25 euros for their time.
Data collection and analysis
Between May 2019 and January 2021, seven in-depth semi-structured interviews – either with couples or with the female partner only – were conducted face-to-face at a location of the respondents’ preference or using a secure video calling programme (because of COVID-19) by AW and SvdH. The interview topic guide included the following topics: views on WES-based ECS, decision-making with regard to participation in WES-based ECS and reproductive options after a positive test result, evaluation of the decision to participate in WES-based ECS and the impact of participation. All interviews, but one, were audiotaped and transcribed verbatim. One respondent did not consent to the taping of the interview and extensive notes were made. The interviews lasted about 45-90 minutes.
A thematic analysis [11] was used to explore the experiences and views of respondents with regard to WES-based ECS. The transcripts were read and reread to identify and index themes. Through a process of constant comparison, the data were classified and clustered into key themes and subthemes. Data analysis continued until no new themes emerged from the interviews. All interviews were independently coded by AW and SvdH. Coding was compared for reliability and discrepancies were discussed until agreement was reached. Representative quotes were selected to illustrate the views and experiences of study respondents. All quotes were translated into English while preserving the verbatim character of the original statements.
Results
Respondent characteristics
Of the seven interviews, three were with respondents of non-Western origin (Turkish, Moroccan or Yemeni) and four with respondents of Dutch origin. Respondents were either first (R01), double first (R02) or second cousins (R03, R06). In three cases, the degree of consanguinity was unknown (R04, R05, R07). Five interviews were conducted with couples and two with women only. Five couples were referred for WES-based ECS after the birth of a child with a severe autosomal recessive disorder, all of whom proved to be homozygous. Two couples requested the test on their own initiative. At the time of the interview, six couples already knew their test results, three of whom were enroled in a PGT-trajectory. Only one couple (R03) was still waiting for the ECS-results (Table 1). Although in principle, WES-based ECS at MUMC+ is meant for couples who are not pregnant, two couples (R01 and R03) were expecting a child when they participated in ECS.
The 5 main themes arising from the data were: (1) Awareness of increased genetic risk related to consanguinity; (2) Reasons to participate in WES-based ECS; (3) Facilitators and barriers in the decision-making process with regard to participation in WES-based ECS; (4) Facilitators and barriers in the decision-making process with regard to reproductive options after a positive test result; (5) Experiences with the screening process.
Awareness of increased genetic risk related to consanguinity and knowledge of autosomal recessive inheritance
Although most respondents reported to be aware of their increased risk of having affected offspring due to their consanguineous relationship, their knowledge about autosomal recessive inheritance was limited. One respondent, aware of having an “increased risk of having a child with a disability” (R02), was still shocked when she received a positive test result. As the diseases that were mentioned as examples during pretest counselling did not occur in her family, she expected nothing would come out of the test. Another respondent indicated to “have a strong family” (R01, male). The risk of being a carrier and transmitting a genetic disorder to offspring was not only misunderstood by some of our respondents, but also by their family members. They did not see the need to participate in ECS. One respondent reported having been accused of “thinking too complicated, [as] no one in the family has the disease” (R02).
Some respondents did not understand the kinds of disorders covered in a preconception carrier screening offer. For instance, ECS was confused with non-invasive prenatal testing (NIPT):
“I found it reassuring to know that everything had been ruled out […]. Later, when we were offered the NIPT, I was wondering whether we should actually do this. Because […] everything has already been ruled out, so it would be strange if the NIPT would turn out positive” (R04, female).
Reasons to participate in WES-based ECS
Informed choice
For most respondents, the opportunity to make an informed decision regarding family planning was a main motivation to participate in WES-based ECS. One respondent indicated that she and her partner wanted to be informed about possible genetic risks before starting a family. They wanted to increase the chance to conceive a healthy child, “not only for our own sake […], but also in the best interest of the child” (R04, female).
Parental responsibility
Some respondents thought it was not only ‘sensible’, but also a ‘parental responsibility’ to prevent the conception of an affected child. This was an important reason to participate in carrier screening:
“The responsibility towards your own child… Obviously, you don’t want to burden your own child with a rare condition. […] You have the option to find out. So that’s what I went for” (R05).
The experience of having a parental responsibility to avoid suffering was especially strong among couples who already had a child with an autosomal recessive disorder. After all, “you know what’s at stake” (R01, male). In addition, having done everything possible to conceive a healthy child was a strong motive to accept the screening offer: “I would actually like to have another healthy child, but even if they’re not healthy, then I’ve done the best I can” (R06, female).
Facilitators and barriers in the decision-making process with regard to participation in ECS
Pre-test counselling
Most respondents indicated that they only received condensed information during pre-test counselling.
“Actually very concise… That 2000 different things were looked at. And that bit about out-of-pocket expenses” (R03, male).
One respondent indicated that, as she and her partner knew very little about autosomal recessive disorders and screening opportunities, “we really don’t know if we missed anything” (R06, female). Moreover, many respondents did not recall that reproductive options were discussed during pre-test counselling.
Interviewer: “And were those reproductive options, such as PGT, discussed as well?”
Respondent: “No, no. Not yet” (R06, female).
In spite of receiving limited information, respondents were generally satisfied with the pre-test counselling. This had largely to do with the attitude of the clinical geneticist. In particular, respondents appreciated how responsive their counsellor was on email:
“I have the doctor’s email address and I can always send an email” (R03, female).
Scope of WES-based ECS
The broad scope of WES-based ECS made some respondents hesitant about participation:
“At first, I was like, why would we want that? To what extent do you want to know everything? I think that’s kind of tricky, too. There’s a tension between wanting to know and not wanting to know” (R03, female).
“Do we want to know everything about ourselves? Which potential conditions or whatever could come out of [the test]? Actually, it was a complex issue” (R07, male).
Most respondents, however, were positive about the broad scope of the test and wished to be informed about carrier status of both severe, mild, early- and late-onset disorders:
“I would like to know everything. That’s why I took the test. I want to know everything: whether small or big” (R02).
Religious beliefs
When discussing the role of religion, respondents of Dutch origin indicated that this had no influence on their decision to participate in ECS; among these respondents, we did not observe any differences between those with and without religious beliefs. This was different for respondents of non-Dutch origin, all of whom were Muslims. A female respondent of Moroccan origin indicated that she was hesitant as to whether or not to accept the screening offer:
“I think that some things are a gift from God. If God has given this [i.e. a positive carrier status] to me, is it acceptable that I try to figure out everything?” (R05).
A couple with a Yemeni background believed it to be acceptable to make use of preventive options:
“We are Muslims, but we also use our common sense. And this does not conflict with Islam. […] We listen and we also follow our hearts” (R06, female).
Financial aspects
Even though out-of-pocket insurance costs did not arise as an important factor in respondents’ decision-making process, many indicated that financial barriers may withhold others from having the test:
“We were in a position that we could [afford] it, but I can also imagine that if you have less to spend, this might be a reason to refrain from it. It [participating in ECS] is rather expensive” (R04, female).
Facilitators and barriers in the decision-making process with regard to reproductive options after a positive test result
Reproductive options are not always available and do not always lead to desired results
Participation in WES-based ECS did not always lead to reproductive options that were experienced as ‘meaningful’ by our respondents. For instance, one respondent stated that, being aware of her and her partner’s positive carrier status made it impossible for her to give her daughter a sibling. Neither IVF followed by PGT, nor prenatal diagnosis followed by a possible termination of pregnancy, were good options for her. She feared that IVF would make her ill because of the hormones, which would hinder her in taking care of her daughter. Moreover, she was very hesitant about undergoing amniocentesis due to the risk of miscarriage:
“I do have those options now, but then again I don’t, because I don’t know what to do. I have too much information […] Some people just make children. They might be happier than me” (R02).
For one of the couples (R03), IVF did not lead to a successful pregnancy, as the female partner did not respond to the hormones that were part of the procedure. This motivated her and her partner to achieve a spontaneous pregnancy followed by prenatal diagnosis instead of opting for IVF/PGT.
Many respondents considered information about carrier status valuable in itself, even if the test would show them to be a carrier couple of a disorder that for lack of severity would not meet current Dutch indication criteria for PGT, which require that conditions are life threatening or have a significant impact on quality of life. One respondent explained that this would still enable her to “prepare [her]self psychologically for what is coming. So that’s important to me” (R04, female). Another respondent argued that being informed about their carrier status as a couple would prevent her from “mulling things over” (R05), even if the positive test results would not lead to access to PGT.
Variable expression
Several respondents brought up the complexity of decision-making with regard to disorders with variable expression. One respondent argued that, being aware that he and his partner were carriers of a disease that may lead to either mild or severe symptoms, did not reduce his uncertainty:
“There are eighteen children in the Netherlands with [X] disease, but there is so much difference between them. At a certain point you have to make a choice. Suppose you are a carrier of something, what does that mean? […] The same applies to people with Down’s syndrome, that comes in different degrees as well” (R01, male).
Experiences with the screening process
Even though respondents were in general positive about the screening procedure, the waiting time for the ECS result was considered to be (too) long. Waiting for the test results was often done in already difficult circumstances. Some respondents had recently lost a child suffering from a severe recessive disorder (R06) or had been faced with recurrent pregnancy loss (R01). One respondent, who was 10 weeks pregnant at the time of the interview, had been confronted with both. She experienced her current pregnancy as very emotional, and went from one check-up to another. This had made her hesitant about participating in WES-based ECS:
“I had doubts about doing this [i.e. undergoing ECS]. You can keep going forever” (R03, female).
One respondent, who was eight weeks pregnant when she participated in ECS, reported that the result became known when termination of pregnancy was no longer an option:
“She [the clinical geneticist] said: ‘The test takes 100 days.’ This made me think: why does it have to take so long? I knew then, for my pregnancy, it wouldn’t really matter anymore. But I also knew: if one more [affected child] came along, it would definitely matter” (R01, female).
Discussion
This is the first study to explore the experiences and views of consanguineous couples who were offered WES-based ECS. Our results show that overall, participation was experienced as worthwhile: respondents indicated that it enabled them to make informed choices with regard to family planning as well as to take on a felt parental responsibility to give their children the best possible start, or at least to avoid suffering in their offspring. This finding on reasons to participate is in line with previous Dutch studies on non-consanguineous couples’ experiences with ECS [12, 13]. While emphasising that participating in WES-based ECS contributed to informed reproductive decision-making, most respondents claimed that they only received condensed information during pre-test counselling; the information about the screening trajectory and the conditions included in the screening panel was experienced as being very concise. Moreover, respondents recalled that reproductive options were only discussed after a positive test result. Most respondents were nonetheless satisfied with the counselling trajectory. Interestingly, the responsive attitude of the clinical geneticist was a more important factor for decisional satisfaction than receiving comprehensive information about the screening process and reproductive options after a positive test result.
A major motivation of clinical geneticists for limiting pre-test information is to avoid the risk that couples become overwhelmed with genetic information (personal communication). In the 1990s already, strategies based on ‘generic’ consent have been proposed for genetic screening. These strategies are aimed at enabling patients to make informed choices, but at the same time seek to “avoid the information overload that could lead to ‘misinformed’ consent” [14]. In the context of ECS, a strategy based on generic consent implies that the genetic counsellor does not give a full explanation of the clinical and test characteristics of each condition, but broadly describes the categories of conditions being screened for [15]. More detailed information about specific disorders will only be given after a positive test result. To ensure that couples receive balanced information about the potential implications of different types of findings, generic consent should not be interpreted as an alternative for, but rather as a variant of informed consent. Such an approach is in line with the ‘reasonable person standard’ [16] and would require that reproductive options and their success rates are explicitly mentioned – albeit not extensively discussed – during pre-test counselling.
Although most respondents were aware of increased reproductive risks related to consanguinity, their understanding of autosomal recessive inheritance and the insignificance of a non-contributory family history was incomplete (see also Thain et al. 2019 [9]). Misunderstandings about the kinds of disorders included in preconception carrier screening can lead to false reassurance and may withhold couples from participating in other forms of reproductive screening, for instance when they think that a negative ECS result makes NIPT obsolete. The clinical geneticist can play a pivotal part in correcting misconceptions as well as exploring participants’ risk awareness during pre- and post-test counselling.
Since in the Netherlands, all citizens over 18 years of age are required to pay annually for the first 385 euros of their healthcare expenses out of their own pocket, couples may have to pay a personal contribution for participating in WES-based ECS. Although the respondents involved in our study were not withheld by these expenses, many of them indicated that these might be a barrier for couples with lower incomes. To limit out-of-pocket expenses and facilitate equal access, the Clinical Genetics Department of MUMC+ claims the costs of WES-based ECS of both partners on the female partner’s account. Moreover, we must not forget that in many countries, ECS for consanguineous couples is not covered under national health insurance at all.
We explained that there are substantiated reasons for choosing a broader scope of screening in this particular population than recommended in the ESHG guidelines. After all, consanguineous couples may be at risk for any autosomal recessive disorder, including extremely rare ones. A possible consequence of this broad scope deserving special attention is that couples may be faced with positive test results that for lack of severity are not accepted as an indication for PGT. Respondents argued that they considered information about genetic risks valuable in itself, even without the option to participate in PGT. Our finding that respondents want to know “everything that could come out of the test” is supported by various other studies. For instance, Kraft et al. 2018 [17], who explored whether patient decision-making is served by sorting conditions into categories, reported that most respondents were interested in receiving all categories of results [17]. Conijn et al.’s [18] respondents were more hesitant, especially with regard to including late-onset disorders, as these would deprive children of “a carefree childhood” [18]. It should, however, be added that the respondents participating in our study were found to be carrier couples of autosomal recessive disorders with PGT-indication. Considering how some of them struggled with findings that did not lead to courses of action that they experienced as ‘meaningful’, the question arises as to whether they would have been as positive about ‘knowing everything’ if the test would have revealed a positive carrier status for a recessive disorder without PGT-indication. The possible disadvantages of such a test result should be balanced against the advantage of identifying serious reproductive risks that would otherwise have remained unknown.
Our findings support the recommendation that pre-test information should include the possible implications of a positive test result for specific categories of findings, as well as the success rates of the available reproductive options; participants may not only wrongly assume that all reproductive options are available, but also that they will lead to the desired outcome, i.e. the birth of an unaffected child. Furthermore, our findings underline the importance of delivering customised solutions; while the ESHG recommendation to limit the scope of screening to severe childhood onset disorders is sometimes too easily defined as the ‘golden standard’, we must also be careful not to simply use respondents’ stated preferences as guiding, especially if their experience with unanticipated outcomes is limited. In determining the scope of screening, we should be guided by the question as to whether the information obtained is useful in reproductive decision-making [19]. More research is needed to explore what type of genetic risk information is considered ‘meaningful’ by participants and actually contributes to reproductive decision-making.
Limitations
Our exploratory study has certain limitations that must be acknowledged. First, this study was conducted with a small and diverse sample size in a Dutch setting. Moreover, five out of seven couples already had a child with an autosomal recessive disorder before participating in WES-based ECS, three of whom were enroled in a PGT-trajectory. As they had quite substantial background knowledge about genetic risks related to consanguinity, some caution is needed in generalising our findings. Second, non-respondents in ECS were not included in our study. It is possible that the study population was biased towards people who are more inclined to provide positive feedback regarding counselling and participation in ECS than non-respondents. Third, views of clinical geneticists were not included in our study and the statements of the respondents regarding the provision of information during pre-test counselling cannot be checked. There is a great possibility of recall bias, provided that the interviews were conducted after the pre-test counselling sessions.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available in order to protect the privacy of our research participants. They are, however, available from the corresponding author on reasonable request.
References
Ropers HH. On the future of genetic risk assessment. J Community Genet. 2012;3:229–36.
Fridman H, Yntema HG, Magi R, Andreson R, Metspalu A, Mezzavila M, et al. The landscape of autosomal-recessive pathogenic variants in European populations reveals phenotype-specific effects. Am J Hum Genet. 2021;108:608–19.
Bittles AH, Black ML. The impact of consanguinity on neonatal and infant health. Early Hum Dev. 2010;86:737–41.
Sheridan E, Wright J, Small N, Corry PC, Oddie S, Whibley C, et al. Risk factors for congenital anomaly in a multiethnic birth cohort: an analysis of the Born in Bradford study. Lancet 2013;382:1350–9.
Hamamy H. Consanguineous marriages: Preconception consultation in primary health care settings. J Community Genet. 2012;3:185–92.
Sallevelt S, Stegmann APA, de Koning B, Velter C, Steyls A, van Esch M, et al. Diagnostic exome-based preconception carrier testing in consanguineous couples: results from the first 100 couples in clinical practice. Genet Med. 2021;23:1125–36.
Kahrizi K, Hu H, Hosseini M, Kalscheuer VM, Fattahi Z, Beheshtian M, et al. Effect of inbreeding on intellectual disability revisited by trio sequencing. Clin Genet. 2019;95:151–9.
Plantinga M, Van Langen I 2018. Available from: https://www.biotechnologie.nl/dragerschapsscreening-als-alternatieve-route/.
Thain E, Shuman C, Miller K, Sappleton K, Myles-Reid D, Chitayat D, et al. Prenatal and preconception genetic counseling for consanguinity: Consanguineous couples’ expectations, experiences, and perspectives. J Genet Couns. 2019;28:982–92.
Sallevelt S, de Koning B, Szklarczyk R, Paulussen ADC, de Die-Smulders CEM, Smeets HJM. A comprehensive strategy for exome-based preconception carrier screening. Genet Med. 2017;19:583–92.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
van Dijke I, Lakeman P, Sabiri N, Rusticus H, Ottenheim CPE, Mathijssen IB, et al. Couples’ experiences with expanded carrier screening: evaluation of a university hospital screening offer. Eur J Hum Genet. 2021;29:1252–8.
Plantinga M, Birnie E, Abbott KM, Sinke RJ, Lucassen AM, Schuurmans J, et al. Population-based preconception carrier screening: how potential users from the general population view a test for 50 serious diseases. Eur J Hum Genet. 2016;24:1417–23.
Elias S, Annas GJ. Generic consent for genetic screening. N. Engl J Med. 1994;330:1611–3.
Edwards JG, Feldman G, Goldberg J, Gregg AR, Norton ME, Rose NC, et al. Expanded carrier screening in reproductive medicine-points to consider: a joint statement of the American College of Medical Genetics and Genomics, American College of Obstetricians and Gynecologists, National Society of Genetic Counselors, Perinatal Quality Foundation, and Society for Maternal-Fetal Medicine. Obstet Gynecol. 2015;125:653–62.
Odwazny LM, Berkman BE. The “Reasonable Person” Standard for Research Informed Consent. Am J Bioeth. 2017;17:49–51.
Kraft SA, McMullen CK, Porter KM, Kauffman TL, Davis JV, Schneider JL, et al. Patient perspectives on the use of categories of conditions for decision making about genomic carrier screening results. Am J Med Genet A 2018;176:376–85.
Conijn T, van Dijke I, Haverman L, Lakeman P, Wijburg FA, Henneman L. Preconception expanded carrier screening: a focus group study with relatives of mucopolysaccharidosis type III patients and the general population. J Community Genet. 2021;12:311–23.
Dondorp WJ, de Wert GM. The ‘thousand-dollar genome’: an ethical exploration. Eur J Hum Genet 2013;21:S6–26.
Acknowledgements
We would like to thank Sander Stegman for reviewing the parts of the manuscript in which information was provided about the WES-based ECS test offered at MUMC+.
Funding
This research was funded by the Clinical Genetics Department of Maastricht University Medical Center, the Netherlands.
Author information
Authors and Affiliations
Contributions
AW and SvdH conducted the interviews, analysed the collected data and draughted the manuscript. GdW and WD contributed to interpreting the results. AP, CdD and SS draughted the text with background information about the WES-based ECS test offered at MUMC+. GdW, WD, AP, CdD and SS all contributed to revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study received an ethics review waver under the Dutch Act on Research with Human Subjects by the Medical Ethics Committee of MUMC +.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van der Hout, S., Woudstra, A.J., Dondorp, W. et al. Consanguineous couples’ experiences and views regarding expanded carrier screening: Barriers and facilitators in the decision-making process. Eur J Hum Genet 31, 1317–1322 (2023). https://doi.org/10.1038/s41431-023-01402-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01402-z
This article is cited by
-
Deep phenotyping and population-level data can help resolve genomic variants
European Journal of Human Genetics (2023)