Abstract
If undetected, inherited cardiac conditions can lead to sudden cardiac death, while treatment options are available. Predictive DNA testing is therefore advised for at-risk relatives, and probands are currently asked to inform relatives about this. However, fewer than half of relatives attend genetic counselling. In this trial, we compared a tailored approach to informing relatives, in which probands were asked whether they preferred relatives to be informed by themselves or by the genetic counsellor, with current practice. Our primary outcome was uptake of genetic counselling in relatives in the first year after test result disclosure. Secondary outcomes were evaluation of the approach and impact on psychological/family functioning measured 3 (T1) and 9 (T2) months post-disclosure via telephone interviews and questionnaires. We included 96 probands; 482 relatives were eligible for counselling and genetic testing. We observed no significant difference in uptake of genetic counselling between the control (38%) and the intervention (37%) group (p = 0.973). Nor were there significant differences between groups in impact on family/psychological functioning. Significantly more probands in the tailored group were satisfied (p = 0.001) and felt supported (p = 0.003) by the approach, although they also felt somewhat coerced to inform relatives (p < 0.001) and perceived room for improvement (p < 0.001). To conclude, we observed no differences in uptake and impact on family/psychological functioning between the current and tailored approach, but probands in the tailored group more often felt satisfied. Further research on barriers to relatives attending genetic counselling and on how to optimize the provision of a tailored approach is needed.
Similar content being viewed by others
Introduction
If they remain undetected, inherited cardiac conditions (ICCs), such as cardiomyopathies and primary arrhythmia syndromes, may lead to severe heart failure or even sudden cardiac death (SCD) at young age [1]. ICCs generally follow an autosomal dominant inheritance pattern, with first-degree relatives being at 50% risk of inheriting the disease-causing variant [2]. Given incomplete penetrance and variable expression, relatives carrying the disease-causing variant may be unaware of their risks of disease and SCD (2). Predictive DNA-testing and/or cardiac monitoring is therefore advised for at-risk relatives to determine whether they carry the disease-causing variant or show subtle signs indicating early features of disease [2, 3]. Predictive DNA-testing thus allows for prevention and timely treatment in relatives and supports their decision-making about life and reproductive choices [2].
Probands (the first person in a family diagnosed with the ICC in whom a (likely) pathogenic variant is identified) are asked to inform relatives about the advice to seek genetic counselling to discuss predictive DNA-testing and/or cardiac monitoring [4]. In some countries, including the Netherlands, a family letter is provided to support this process [4, 5]. However, in current practice, less than half of relatives attend genetic counselling for predictive DNA testing in the first year following probands’ genetic diagnosis [2, 4, 6, 7]. Even in the 16-years post proband diagnosis, uptake only increases to 60% [8]. Previous research indicated that probands struggle with informing relatives due to barriers, such as family conflicts [5, 9] and the complicated nature of genetic information [10], and probands experience informing relatives as practically and mentally burdensome [11]. As a result, relatives may be not informed or lack appropriate information, complicating informed decision-making.
Certain interventions, including enhanced support for probands in informing at-risk relatives, have been effective in increasing uptake of genetic counselling [12]. Research on healthcare professionals directly contacting relatives indicates that this could almost double the uptake in relatives, although some of these studies were registry-based, with relatives already being familiar with the genetic nature of the disease via the registry [13,14,15,16]. While these studies did not show psychological harm in probands or relatives, direct contact approaches may lead to unwarranted worry or coercion to choose in favour of predictive DNA-testing [13, 14]. Moreover, healthcare professionals may be unaware of personal or family characteristics that may make the direct approach unsuitable. In the Netherlands, a direct contact approach without consent of the proband is not allowed, except in case of significant health concerns for relatives. In other (European) countries, a direct contact approach is even prohibited.
We hypothesised that tailoring the contact approach to probands’ preferences and their family and personal characteristics would effectively support them in informing at-risk relatives and improve the number of relatives (appropriately) informed by genetic counselling [17]. We chose to do so using a tailored approach in which probands could express which relatives they preferred to inform themselves and those they wished informed by the clinical geneticist/genetic counsellor (hereafter referred to as genetic counsellor). This approach acknowledges the probands’ knowledge of family functioning and their relatives’ personal characteristics while also respecting the probands’ autonomy [18]. In this randomised controlled trial, we investigated the effect of our tailored approach on the uptake of genetic counselling in comparison to current practice. In addition, we evaluated appreciation of the approach used and assessed impact on psychological and family functioning.
Methods
Design
In three cardiogenetic centres in the Netherlands, we conducted a randomised controlled trial with a parallel-group design that compared a tailored approach (intervention group) with the family-mediated approach (current practice/control group). Probands were randomised using computerised randomisation software based on a 1:1 allocation ratio [19]. Full details of the study protocol are described elsewhere [17].
Procedure
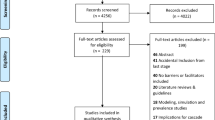
Figure 1 shows a flowchart of the study procedure and inclusion. Enrolment of participants took place between November 2017 and November 2020. Probands 18 years or older with an ICC, or suspicion thereof, were approached for inclusion if they: (1) were the first in their family to visit the cardiogenetic outpatient clinic for counselling about genetic testing for ICCs, (2) had at least one living adult relative and (3) had mastered the Dutch language. Probands were then included if a likely pathogenic (class 4) or pathogenic (class 5) DNA variant in a disease-associated gene was identified. Penetrance of class 4 and 5 variants is substantial; therefore, predictive DNA-testing and/or cardiac monitoring is advised for relatives. Relatives of included probands were approached to participate if they were: (1) an 18-year-old or older first-degree relative or second-degree relative when a deceased connecting relative was affected or suspected to be affected and (2) able to read and write Dutch. Probands and relatives were informed about the study by the genetic counsellor during pre-test counselling and received an information letter. If interested, the executing researcher (LvdH) contacted participants by telephone and written informed consent forms were sent. Probands were randomised prior to test result disclosure. The counsellor would then discuss the approach to informing relatives based on randomisation. Subsequently, probands were asked to participate in a structured telephone interview and to fill out a questionnaire (paper or online) 3 and 9 months after test result disclosure. Relatives were asked to fill out one questionnaire after pre-test counselling.
Intervention
During post-test counselling, probands in the intervention group were asked which relatives they preferred to inform themselves and which relatives they preferred be informed by the genetic counsellor. Probands were also asked to consent to a family letter being sent directly to all eligible relatives after one month, irrespective of whether they were already informed by the proband. Consenting probands were further asked to provide relatives’ contact details. If probands were unable to get contact details, these relatives also did not receive a direct family letter. The family letter was standardised for all three centres and did not reveal the probands’ identity Supplementary Material S1). For the intervention group, the letter also included a link to a website specifically designed for this study (www.familieleden.erfelijkehartziekten.nl) that provided tailored information about the disease, the procedure of predictive DNA-testing and considerations to include when deciding whether to undergo DNA-testing using a short survey popping up the first time someone visited the website. Relatives of probands in the control group were referred to a general website about ICCs (www.erfelijkehartziekten.nl), showing similar (but non-tailored) information.
Data collection
Primary outcome measures
The primary outcomes were uptake of (1) genetic counselling and (2) predictive DNA-testing by at-risk relatives in the first year after disclosure of the probands’ DNA-test result. To assess uptake, the number of eligible relatives attending genetic counselling and the number of relatives pursuing predictive DNA testing were collected using data from the DNA-laboratories of participating centres. The number of eligible relatives was obtained using family pedigrees of the participating centres. First-degree relatives were considered eligible, as were second-degree relatives if there was a deceased connecting first-degree relative suspected of having an ICC.
Secondary outcome measures
Secondary outcome measures included (1) appreciation of the approach used to inform at-risk relatives and (2) impact on psychological and family functioning in both probands and relatives. Items administered are described in the supplementary material of the study protocol [17].
Appreciation:
Five self-constructed items on appreciation were administered in probands at 3 months (T1). In relatives, six self-constructed items were used [17]. During the structured telephone interview, probands were asked to answer one additional item about whether they would have preferred to inform their relatives differently. To assess decisional conflict in probands in the intervention group, probands were asked to rate two 5-point Likert-scale items stating: (a) that probands had experienced any difficulties in deciding which relatives they had to inform and which relatives should be informed by the genetic counsellor and (b) that they were satisfied with their decision. At 9 months (T2), probands were asked whether their opinion about the approach used had changed. In addition, probands (at T1 and T2) and relatives were asked whether they visited the websites www.erfelijkehartziekten.nl (control group) or www.familieleden.erfelijkehartziekten.nl (intervention group).
Impact on family functioning:
The perceived impact on family functioning and communication difficulties was assessed in probands (at T1 and T2) and relatives by the 10-item Openness to Discuss Cancer in the Family (ODCF) scale [20]. The ODCF scale was adapted by changing ‘cancer’ into ‘ICC’, and a higher score indicates more communication difficulties. Of the original ODCF scale, psychometric characteristics were satisfactory [20]. We also included a self-constructed item to ask whether probands and relatives experienced changes in relationships because of providing information on the ICC. Self-efficacy and perceived motivators and barriers to informing relatives were assessed by the ‘motivation’ and ‘self-efficacy’ subscales of the Informing Relatives Inventory (IRI), with ‘cancer’ adapted to ‘ICC’ [21]. Reliability and validity were assessed as satisfactory [21]. Probands were also asked to answer self-constructed items during telephone interviews asking (a) which relatives were considered eligible for genetic counselling and predictive DNA-testing, (b) whether these relatives were informed and (c) whether probands intended to inform (remaining) relatives.
Impact on psychological functioning:
Participants were asked to fill out an adapted version of the validated Cancer Worry Scale (CWS) with ‘cancer’ changed to ‘ICC’ [22]. This scale consists of eight items on a 4-point Likert scale (range 8-32), with a higher score indicating more worry. Reliability and validity of the original CWS were assessed as satisfactory [22]. In addition, we administered the Hospital Anxiety and Depression Scale (HADS) to assess participants’ anxious or depressed feelings [23]. A cut-off score of 8 was used for the anxiety and depression scores; psychometric characteristics were found to be good [23].
Participant characteristics
Sociodemographic and clinical characteristics collected for probands (at T1) and relatives included: gender, education level, living situation and parental status, family history and probands’ diagnosis. Relatives were also asked for their kinship with the proband. Psychosocial and personality factors included: coping style, trait anxiety, risk perception and health literacy. Coping style was assessed using the shortened version of the Threatening Medical Situations Inventory (TMSI) [24]. The TMSI assesses whether individuals have a ‘monitoring’ versus ‘blunting’ coping style related to a medical threat and was previously evaluated in an oncogenetic patient population [24, 25]. The shortened version of the TMSI contains two subscales, each consisting of six items. Reliability and validity of the Dutch TMSI were satisfactory [24]. The 20-item Trait subscale of the State Trait Anxiety Inventory (STAI) was administered to assess trait anxiety [26]. Psychometric characteristics of the Dutch translation of the STAI are assessed as good [26]. Health literacy was assessed in probands and relatives using the ‘functional health literacy’ and ‘communicative health literacy’ subscales of the 3HL questionnaire [27]. The 3HL questionnaire was assessed as having high reliability and satisfactory validity [27].
Data analysis
Sample size calculation was based on the primary outcome measure: uptake of genetic counselling. We aimed to detect a difference of 15% between the control and intervention group. To this aim, we needed 340 relatives eligible for genetic counselling and predictive DNA testing. With on average four eligible relatives per proband, 85 probands with a (likely) pathogenic variant needed to be included [17]. An intention-to-treat approach was used for analyses. We did not differentiate between high penetrance versus medium or low penetrance (likely) pathogenic variants, as our policy for at-risk relatives is the same for these variants. Family-clustered logistic regression analysis was performed to assess differences between randomisation groups on the primary outcome (uptake), with the randomisation group as the main explanatory variable and relatives nested in families and in hospitals (glm package in R). The selection of variables was based on previous literature on uptake of genetic counselling in ICCs [4]. We present a non-adjusted model, a fully adjusted model and a final model with best fit based on AIC and BIC values. For secondary outcomes, we assessed differences in appreciation of the approach between randomisation groups using chi square or Fisher’s exact tests, as appropriate. For chi-square tests and Fisher’s exact tests, we report the Cramer’s V to explore the strength of the difference: V < 0.20 considered weak, V = 0.20‒0.30 moderate and V > 0.30 strong. Next, multilevel mixed-model regression analyses using the lme4 package in R were conducted to assess the impact of randomisation on family and psychological functioning in probands, when adjusting for covariates. A non-adjusted model, fully adjusted model and final model with optimal fit based on AIC and BIC values are presented per outcome measure (Supplementary Material S2). For relatives, independent sample t-tests or Mann–Whitney U tests and chi-square or Fisher’s exact tests were conducted to assess differences between randomisation groups in appreciation and family and psychological functioning in relatives, as appropriate. A Bonferroni-corrected p value of <0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS (v25.0) and R Studio (v1.2.5033).
Results
Study population
In total, 615 probands who were approached by the genetic counsellor agreed to be contacted by the researcher (74% of probands were considered eligible based on patient notes taken in two of the three centres participating). Of these 615 probands, 407 (66%) provided informed consent to participate. In 96 of the 407, a (likely) pathogenic variant was detected, and these 96 participated in this study (Fig. 1). Of their relatives, 95 of the 96 relatives (99%) approached during genetic counselling agreed to be contacted by the researcher to fill out a questionnaire. Of these relatives, 77% (N = 73) could be contacted and provided consent, of which 70% (N = 51) completed a questionnaire. Due to short turn-around times in the DNA laboratory, most relatives (43 out of 51; 84%) received their DNA test result prior to filling out the questionnaire, of whom N = 15 (65%) received an unfavourable result in the intervention group compared to N = 13 (65%) in the control group.
Table 1 shows the sociodemographic and clinical characteristics of the study population. Probands in the control group had a median of six eligible relatives (range 1‒16), compared to five eligible relatives (range 1‒23) in the intervention group. We observed no significant differences between the randomisation groups in proband characteristics. Relatives eligible for genetic counselling in the intervention group had a cardiomyopathy diagnosed in their family significantly more often (p = 0.005), were less often a first-degree relative (p = 0.035) and more often had a relative who died from SCD (p < 0.001). Of the relatives filling out a questionnaire, 32% (N = 8) in the control group had a primary arrhythmia syndrome diagnosed in their family compared to none in the intervention group (p = 0.002). Other characteristics were not significantly different.
Uptake of genetic counselling and predictive DNA testing
In total, 483 relatives were eligible for genetic counselling and predictive DNA testing (control: N = 252, 52%; intervention: N = 231, 48%). We observed no significant difference in uptake of genetic counselling between the control (38%) and intervention (37%) groups (p = 0.973) (Fig. 2). Of relatives attending counselling, almost all proceeded with predictive DNA testing in both groups. Within the intervention group, 24 relatives from seven families (out of 48 families; 14.6%) did not receive a family letter directly from the genetic counsellor because the proband did not consent to this or no contact details were available. Six of these relatives (25%) attended genetic counselling. Eight probands (out of 43 participating in the structured interview; 18.6%) indicated at T1 that they had decided that all or certain relatives in their family would be informed directly by the genetic counsellor. Relatively more probands in the control group reported that none (N = 3, 7%) or only some (N = 8, 20%) of their relatives were informed at T1 compared to the intervention group (none informed: N = 0, 0%; some informed: N = 3, 8%). At T2, almost all relatives were informed (control: none informed N = 1 (3%), partly informed N = 3 (8%); intervention: none informed N = 0 (0%), partly informed N = 1 (3%)). Some probands encountered difficulties with relatives living abroad and not having contact details of these relatives. Relatives considered eligible differed significantly in ICC type, kinship, whether relatives were diagnosed with the ICC prior to test result disclosure and SCD (Table 1). After adjusting for these and other covariates, the randomisation groups still showed no significant difference in uptake (Table 4, Supplementary Material S2). First-degree relatives (p = 0.005) and ICC diagnosis in relatives (p = 0.002) remained significant in the final model.
Appreciation of the approach used
Table 2 shows the responses on appreciation items. Probands and relatives in both randomisation groups found that the approach used was justified. Significantly more probands in the intervention group were satisfied with the approach (control: 66%, intervention: 97%; p = 0.001) and felt supported in informing relatives (control: 66%, intervention: 94%; p = 0.003). However, probands in the intervention group also more often felt that the approach could be improved (control: 25%; intervention: 86%; p < 0.001) and indicated they felt somewhat coerced to inform their relatives (control: 22%; intervention: 81%; p < 0.001). While 81% of probands in the intervention group struggled with deciding how to inform relatives (to do so themselves or via the genetic counsellor), 95% reported being satisfied with their decision. At T2, most probands in both groups held the same opinion (control: 90%; intervention: 94%) or had become more positive (control: 3%; intervention: 3%; p = 0.808). Among relatives, no difference in appreciation was observed. Only a few relatives who filled out the questionnaire visited the aforementioned websites (control: N = 7; intervention: N = 2).
Impact on psychological and family functioning
Table 3 lists the mean scores on variables related to psychological and family functioning at T1 and T2 in probands and relatives, per randomisation group.
Impact of intervention on psychological functioning
Probands:
We observed no difference between groups on anxiety and depression at T1 and T2 (Table 3). Mean scores of anxiety and depression were below the cut-off score of 8. Worry about the disease was also comparable for both groups at T1. When adjusting for covariates, the randomisation groups also showed no significant effect on anxiety, depression and worry, as shown in Tables 5‒7 (Supplementary Material S2).
Relatives:
We observed higher but non-pathological anxiety and depression scores in relatives in the intervention group compared to the control group (anxiety: p = 0.002; depression: p = 0.004). No significant differences were found between groups for worrying about the disease in relatives.
Impact of intervention on family functioning
Probands:
No differences in communication difficulties (ODCF) were observed between randomisation groups at T1 and T2, even when controlling for covariates (Table 8, Supplementary Material S2). Most probands reported no impact on relationships with the relatives they informed (control: N = 39 (93%), intervention: N = 41 (98%), p = 0.306) at T1. Moreover, no probands reported worsening of their relationship with relatives due to informing them about the ICC. Probands in the intervention group did report significantly more motivation to inform relatives (p < 0.001), whereas self-efficacy regarding informing at-risk relatives was similar (Table 3).
Relatives:
No differences in median total scores regarding communication difficulties (ODCF) were observed in both groups. Most relatives experienced no impact on their relationship with the proband (control: N = 23 (92%), intervention: N = 22 (88%), p = 0.637). No relatives reported their relationship with the proband had worsened.
Discussion
We hypothesised that by tailoring the approach to probands’ (family) characteristics and preferences, the number of relatives attending genetic counselling would increase. However, we observed no significant effect of the tailored approach on uptake of genetic counselling. Nonetheless, more probands receiving the tailored approach felt satisfied and supported, although more of them also felt somewhat coerced to inform relatives and thought the approach could be improved. Relatives were equally satisfied with either approach, but we found higher anxiety and depression in the intervention group.
We conclude that a tailored approach, in which probands can choose what they feel as the most appropriate approach to inform their relatives, may provide the most optimal support [18, 28, 29]. Furthermore, a tailored approach respects probands’ autonomy [18] and takes their expertise about family dynamics into account [30]. Even so, probands perceived room for improvement, particularly regarding logistics (e.g., timely distribution of family letters and a long waiting list for genetic counselling for at-risk relatives). Some probands also did not prefer a direct letter because of relatives’ privacy. However, although only a few did not provide consent for the direct letter, and thus did not share relatives’ contact details, the request itself may have led some probands in the intervention group to feel somewhat coerced to inform relatives. Because the intervention comprised more steps than the approach in the control group, probands were perhaps more conscious of the approach, which may have led to them having more comments about how to improve it. Moreover, although we did not evaluate the approach among professionals, another study by our research group found that healthcare professionals worry about the workload when using a more active approach. Further research on a tailored approach should therefore include an evaluation among healthcare professionals [11].
Our findings do not corroborate previous research findings that a more active approach increases uptake of genetic counselling and predictive DNA-testing [13,14,15,16]. Since participation, in itself, could increase uptake, we also assessed uptake in the year prior to the study and found no significant difference. This may be explained by the fact that in the tailored approach, in contrast to other direct contact approaches, it was possible for probands to decide not to inform relatives. However, there were only a few probands in the intervention group who did not agree with a family letter sent directly to relatives, and only one proband reported that not all relatives were informed. Furthermore, some studies investigating direct contact reporting increased uptake were registry-based [13, 14], and only one was a randomised controlled trial [14].
Our results raise the question of whether the relatively low uptake of counselling can be fully explained by relatives not being (appropriately) informed. Many relatives may simply decide not to attend genetic counselling. Most relatives probably only ask for a referral for genetic counselling if they already decided in favour of DNA-testing, as supported by the fact that almost all the counselled relatives in this and previous studies pursued DNA-testing [4, 8]. Only limited research has addressed decision-making of at-risk relatives not attending genetic counselling, and knowledge obtained by previous research was mostly collected indirectly (i.e., through probands or relatives who did attend genetic counselling) [31]. It is important to gain insight into decision-making of relatives not attending genetic counselling and into the potential barriers they face, e.g., consequences for health insurance.
Our findings of significantly higher, but still non-pathological, scores on anxiety and depression in relatives contrast with those of previous studies on direct contact that reported no psychological impact, including studies comparing a direct approach with current practice [13,14,15,16]. Due to the low response among relatives attending genetic counselling, research on the psychological impact on relatives of a more active, tailored approach is needed to further investigate this finding. We also observed no impact of the tailored approach on psychological and family functioning in probands.
Strengths and limitations
Strengths of this study include its randomised design, the inclusion of participants from multiple centres and the assessment of the tailored approach on multiple outcomes. This trial also had some limitations. First, despite randomisation, characteristics known to affect uptake were significantly different between randomisation groups. Nevertheless, uptake was not significantly affected by randomisation group when correcting for these characteristics. In addition, we potentially missed relatives who were living abroad or counselled in centres not participating in this study and who not proceeded with predictive DNA-testing. However, in the Netherlands, predictive DNA-testing is conducted in the laboratory where the proband was first counselled and tested and therefore, these tested relatives have been included in the study. Considering the high number of relatives who attends genetic counselling and subsequently pursues predictive DNA-testing, we expect that the vast majority of eligible relatives who attended genetic counselling was collected. Unfortunately, blinding of participants and counsellors was not possible, nor was blinding of the executing researcher, due to the slight differences between the questionnaires in the randomisation groups. A bias in participating probands also cannot be excluded, as probands who anticipated difficulties with informing relatives may have declined participation. In addition, we could only approach relatives who attended genetic counselling for participation, and the logistics of approaching them was complicated. Therefore, only a small number of relatives filled out a questionnaire, leading to a low response and potentially a biased sample. Moreover, unfortunately, a large number of relatives who participated received their DNA test result prior to filling out the questionnaire. This may have affected our findings, especially with regard to the psychological impact. In addition, although eight probands indicated that some or all eligible relatives in their family were informed by the counsellor directly, we could not retrieve data on how many relatives were contacted (at first) by the genetic counsellor. Furthermore, in one centre, the number of probands approached for the trial was not well-documented. Finally, while tailored information for relatives in the intervention group was provided by a special website as part of the intervention, only a few relatives who attended counselling visited the website. This part of the intervention could therefore not be evaluated, and it is unlikely that this intervention component contributed to the effects identified.
Conclusion
A tailored approach to informing relatives at risk of ICCs may provide optimal support for probands in informing at-risk relatives, although no significant effect of this approach was found on uptake of genetic counselling and predictive DNA-testing. However, higher, but non-pathological, anxiety and depression scores were observed in relatives. These results may inform clinical practice using such a tailored approach and indicate how to improve the support provided. Further research is needed to identify barriers that prevent relatives from attending genetic counselling, to assess psychological impact of a tailored approach in relatives and to gain insight into how to optimize a tailored approach.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Wilde AA, Behr ER. Genetic testing for inherited cardiac disease. Nat Rev Cardiol. 2013;10:571–83.
Miller EM, Wang Y, Ware SM. Uptake of cardiac screening and genetic testing among hypertrophic and dilated cardiomyopathy families. J Gen Couns. 2013;22:258–67.
Christiaans I, van Langen IM, Birnie E, Bonsel GJ, Wilde AA, Smets EM. Genetic counseling and cardiac care in predictively tested hypertrophic cardiomyopathy mutation carriers: the patients’ perspective. Am J Med Genet A. 2009;149A:1444–51.
Christiaans I, Birnie E, Bonsel GJ, Wilde AA, van Langen IM. Uptake of genetic counselling and predictive DNA testing in hypertrophic cardiomyopathy. Eur J Hum Genet. 2008;16:1201–7.
Leenen CH, Heijer M, van der Meer C, Kuipers EJ, van Leerdam ME, Wagner A. Genetic testing for Lynch syndrome: family communication and motivation. FamCancer. 2016;15:63–73.
Burns C, McGaughran J, Davis A, Semsarian C, Ingles J. Factors influencing uptake of familial long QT syndrome genetic testing. Am J Med Genet A. 2016;170A:418–25.
Van der Roest WP, Pennings JM, Bakker M, van den Berg MP, van Tintelen JP. Family letters are an effective way to inform relatives about inherited cardiac disease. Am J Med Genet A 2009;149A:357–63.
Van den Heuvel LM, van Teijlingen MO, van der Roest W, van Langen IM, Smets EMA, van Tintelen JP, et al. Long-term follow-up study on the uptake of genetic counseling and predictive DNA testing in inherited cardiac conditions. Circ Genom Precis Med. 2020;13:524–30.
Menko FH, Jeanson KN, Bleiker EMA, van Tiggelen CWM, Hogervorst FBL, Ter Stege JA, et al. The uptake of predictive DNA testing in 40 families with a pathogenic BRCA1/BRCA2 variant. An evaluation of the proband-mediated procedure. Eur J Hum Genet. 2020;28:1020–7.
Forrest LE, Curnow L, Delatycki MB, Skene L, Aitken M. Health first, genetics second: exploring families’ experiences of communicating genetic information. Eur J Hum Genet. 2008;16:1329–35.
Van den Heuvel LM, Huisinga MJ, Hoedemaekers YM, Baas AF, Plantinga M, Henneman L, et al. Informing relatives at risk of inherited cardiac conditions: experiences and attitudes of healthcare professionals and counselees. Eur J Hum Genet. 2019;27:1341–50.
Hodgson JM, Metcalfe S, Gaff C, Donath S, Delatycki MB, Winship I, et al. Outcomes of a randomised controlled trial of a complex genetic counselling intervention to improve family communication. Eur J Hum Genet. 2016;24:356–60.
Aktan-Collan K, Haukkala A, Pylvanainen K, Jarvinen HJ, Aaltonen LA, Peltomaki P, et al. Direct contact in inviting high-risk members of hereditary colon cancer families to genetic counselling and DNA testing. J Med Genet. 2007;44:732–8.
Sermijn E, Delesie L, Deschepper E, Pauwels I, Bonduelle M, Teugels E, et al. The impact of an interventional counselling procedure in families with a BRCA1/2 gene mutation: efficacy and safety. FamCancer. 2016;15:155–62.
Suthers GK, Armstrong J, McCormack J, Trott D. Letting the family know: balancing ethics and effectiveness when notifying relatives about genetic testing for a familial disorder. J Med Genet. 2006;43:665–70.
Frey MK, Kahn RM, Chapman-Davis E, Tubito F, Pires M, Christos P, et al. Prospective feasibility trial of a novel strategy of facilitated cascade genetic testing using telephone counseling. J Clin Oncol. 2020;38:1389–97.
Van den Heuvel LM, Hoedemaekers YM, Baas AF, van Tintelen JP, Smets EMA, Christiaans I. A tailored approach towards informing relatives at risk of inherited cardiac conditions: study protocol for a randomised controlled trial. BMJ Open. 2019;9:e025660.
Leonard SJ, Newson AJ Ethical perspectives. In: Gaff CL, Bylund, CL, editor. Family communication about genetics: Theory and practice. New York: Oxford University Press, inc.; 2010.
CASTOR. Castor Electronic Data Capture 2019 [Available from: castoredc.com].
Mesters I, van den Borne H, McCormick L, Pruyn J, de Boer M, Imbos T. Openness to discuss cancer in the nuclear family: scale, development, and validation. Psychosom Med. 1997;59:269–79.
De Geus E, Aalfs CM, Menko FH, Sijmons RH, Verdam MG, de Haes HC, et al. Development of the informing relatives inventory (IRI): assessing index patients’ knowledge, motivation and self-efficacy regarding the disclosure of hereditary cancer risk information to relatives. Int J Behav Med. 2015;22:551–60.
Custers JA, van den Berg SW, van Laarhoven HW, Bleiker EM, Gielissen MF, Prins JB. The Cancer Worry Scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014;37:E44–50.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–70.
Van Zuuren FJ, De Groot KI, Mulder NL, Muris P. Coping with medical threat: an valuation of the Threatening Medical Situations Inventory (TMSI). Pers Individ Dif. 1996;21:21–31.
Wakefield CE, Homewood J, Mahmut M, Taylor A, Meiser B. Usefulness of the Threatening Medical Situations Inventory in individuals considering genetic testing for cancer risk. Patient Educ Couns. 2007;69:29–38.
Defares PB, Van der Ploeg HM, Spielberger CD. Handleiding bij de Zelf-Beoordelings Vragenlijst ZBV. Een Nederlandse bewerking van de Spielberger State-Trait Anxiety Inventory STAI-DY. Lisse: Swets & Zeitlinger; 1981.
Van der Vaart R, Drossaert CH, Taal E, ten Klooster PM, Hilderink-Koertshuis RT, Klaase JM, et al. Validation of the Dutch functional, communicative and critical health literacy scales. Patient Educ Couns. 2012;89:82–8.
Menko FH, Ter Stege JA, van der Kolk LE, Jeanson KN, Schats W, Moha DA, et al. The uptake of presymptomatic genetic testing in hereditary breast-ovarian cancer and Lynch syndrome: a systematic review of the literature and implications for clinical practice. Fam Cancer. 2018;18:127–35.
Wiseman M, Dancyger C, Michie S. Communicating genetic risk information within families: a review. Fam Cancer. 2010;9:691–703.
Dheensa S, Lucassen A, Fenwick A. Limitations and pitfalls of using family letters to communicate genetic risk: a qualitative Study with patients and healthcare professionals. J Gen Couns. 2018;27:689–701.
Mendes A, Paneque M, Clarke A, Sequeiros J. Choosing not to know: accounts of non-engagement with pre-symptomatic testing for Machado-Joseph disease. Eur J Hum Genet. 2019;27:353–9.
Acknowledgements
We thank T. Filippini, R. Soorchy and S. Kleinendorst for their assistance in the study. We also thank K. McIntyre for editing the manuscript.
Funding
This work was supported by the Netherlands Cardiovascular Research Initiative, an initiative supported by Dutch Heart Foundation (2015-12 eDETECT; 2017-10 DOLPHIN GENESIS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical clearance for conducting this randomised controlled trial was obtained for all participating centres (METC 2017.145).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
van den Heuvel, L.M., Hoedemaekers, Y.M., Baas, A.F. et al. A tailored approach to informing relatives at risk of inherited cardiac conditions: results of a randomised controlled trial. Eur J Hum Genet 30, 203–210 (2022). https://doi.org/10.1038/s41431-021-00993-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-021-00993-9
This article is cited by
-
Direct notification by health professionals of relatives at-risk of genetic conditions (with patient consent): views of the Australian public
European Journal of Human Genetics (2024)
-
Patients’ perceptions and practices of informing relatives: a qualitative study within a randomised trial on healthcare-assisted risk disclosure
European Journal of Human Genetics (2024)
-
Cascade genetic counseling and testing in hereditary syndromes: inherited cardiovascular disease as a model: a narrative review
Familial Cancer (2024)
-
A new system for variant classification?
European Journal of Human Genetics (2022)