Abstract
Background/Objectives
The Protein Screener 55 + (Pro55 + ) is a brief food questionnaire to screen older community-dwelling adults for low protein intake. The result is the predicted probability of protein intake <1.0 g/kg adjusted body weight (aBW)/d ranging from 0–1. For purposes of cross-cultural validation, we translated the Pro55+ into German and tested its discriminative accuracy in detecting low protein intake of older community-dwelling people in Germany.
Subjects/Methods
After translation and pilot-testing, the Pro55+ and the reference standard (3-day dietary record) were completed by 144 participants (81.6 ± 3.9 years, 61.8% female). Discriminative properties were tested by receiver operating characteristic curves and by calculating sensitivity and specificity for different cut-offs of predicted probability (>0.3/>0.5/>0.7) using <1.0 or <0.8 g/kg aBW/d to define low protein intake.
Results
Protein intake was <1.0 g/kg aBW/d in 39.6% of the sample and <0.8 g/kg aBW/d in 17.4%. Area under the curve was 62.0% (95%CI 52.6–71.5) and 68.8% (58.1–79.4), respectively. Specificity was 82–90% using probability cut-offs of 0.5 and 0.7 for both protein thresholds. Sensitivity was poor for protein threshold of 1.0 g/kg aBW/d regardless of the used probability cut-offs. For protein threshold of <0.8 g/kg aBW/d, sensitivity was 88.0% (71.8–96.9) using a probability cut-off of 0.09.
Conclusion
The overall discriminative accuracy of the German Pro55+ to identify older community-dwelling people with low protein intake was poor. However, applying different probability cut-offs allows increasing specificity and sensitivity for 0.8 g/kg aBW/d to levels justifying the use for certain purposes e.g. excluding individuals with adequate protein intake. Further validation is needed.
Similar content being viewed by others
Introduction
Low protein intake has been shown to be associated with accelerated loss of muscle mass and function in older people [1, 2]. Moreover, because of inflammatory processes, insulin resistance, reduced postprandial availability of amino acids, and a blunted anabolic response towards ingested protein, older people may have higher dietary protein needs compared to younger people [3, 4]. Therefore, in recent years expert groups have questioned the existing recommendation for protein intake of 0.8 g/kg BW/d and suggested an optimal protein intake of 1.0–1.2 g/kg BW/d for healthy older adults [5, 6]. In 2017, the German Nutrition Society changed their reference value on protein intake for healthy people 65 years or older to an estimated value of 1.0 g/kg BW/day [7].
Protein intake of older people is often below 1.0 g/kg BW/day [8, 9]. In a recent meta-analysis of four large cohort studies (n = 8107) in community-dwelling older people aged 55 years and older, the pooled prevalence of protein intake below 1 g/kg adjusted body weight (aBW)/d was 46.7% (95%CI 38.3–55.3) [10].
However, intervention studies using protein supplements have often failed to improve muscle mass and function in older people, presumably caused by sufficiently high habitual protein intake [11, 12]. Therefore, it is important to identify older people with low protein intake who may benefit from increased intake.
The adequacy of protein intake is usually evaluated by repeated 24 h recalls, dietary records or food frequency questionnaires (FFQ) [13]. The application of these methods and data analysis requires specific nutritional knowledge and therefore, needs to be performed by trained staff like dietitians or nutritionists. Furthermore, these methods are time-consuming and depend on the motivation and cooperation of the older individual. Especially in frail older adults, dietary assessment can be challenging due to physical limitations and recall bias caused by memory impairments [13,14,15]. Therefore, for clinical practice validated screening instruments for low protein intake would be helpful as a first step to reduce the number of the time-consuming full assessments.
In 2018, the Protein Screener 55 +, a brief food questionnaire to screen older community-dwelling adults (≥55y) for low protein intake (<1.0 g/kg aBW/d) with good discriminative ability compared to the reference standard a FFQ was developed by a Dutch research group [16]. As protein intake pattern may vary between countries, cross-cultural validation is needed before applying this tool in clinical practice in other countries.
The current study aimed to validate the German version of the Protein Screener 55+ in community-dwelling older people using 3-day-dietary-records as the reference standard.
Material/subjects and methods
Protein Screener 55+
The Protein Screener 55 + (https://proteinscreener.nl/#/) comprises ten questions on the amount of intake of protein-rich foods on an average day or the frequency of intake referring to the last four weeks. It includes additionally information on age, sex, body height and weight [16]. The items were derived from a semi-quantitative FFQ (HELIUS FFQ [17]) and selected using multivariable backward regression analyses [16]. The questions ask for slices of bread (number), glasses of milk, buttermilk or soymilk (number), meat with warm dish (portion size), cheese (amount and frequency), dairy products (frequency), eggs, (frequency), pasta (frequency), fish (frequency) and nuts/peanuts (frequency). The screening result is the predicted probability of a low protein intake (<1.0 g/kg aBW/d) with a higher score indicating a higher probability. A predicted probability of more than 0.3 has been identified as the optimal cut-off in a Dutch population, balancing sensitivity and specificity best, to screen for protein intake <1.0 g/kg aBW/d (sensitivity: 82.2%, specificity: 80.0%, AUC: 85.6%) [16].
Validation process
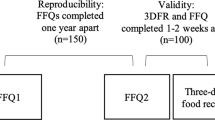
We conducted the validation of the German version of the Protein Screener 55+ in a two-step approach.
Step 1: Translation and layout
The English version was translated to German by a researcher fluent in both languages (EK). Afterwards, two experts reviewed the German translation (HS, DV) for accuracy and comprehensibility. The consented version was then back translated to English by another researcher fluent in both languages (DS), who was blinded to the original version. All results were compared to the original version of the Protein Screener and consensus on the German version was reached.
As we aimed to use the Protein Screener as paper and pencil method that can be self-completed by older adults, a questionnaire template was designed focusing on readability and clear layout. In a pretest, four older adults (3 female, 1 male) aged between 70 and 86 years filled in the Protein Screener and completed a feedback questionnaire on comprehensibility, clarity, missing information, readability, format, time needed for completion, and further remarks. Based on this feedback, the content and layout of the questionnaire were slightly adapted including a simplification of the wording of question 10 and the presentation of answer categories of questions 1, 2 and 10. The time for completion (~5 min) was considered adequate. The German version of the Protein Screener 55+ can be found at https://proteinscreener.nl/#/.
Step 2: Validation study
The validation was conducted at the German study center (Institute for Biomedicine of Aging in Nuremberg) of two at the time ongoing studies (SPRINT-T [18] and SCOPE [19]) between July 2019 and February 2020. SPRINT-T is a multicenter randomized controlled trial to test the efficacy of a multicomponent intervention to prevent mobility disability in older adults (≥70 years) with physical frailty and sarcopenia [18]. For the current analysis, data from the final study visit were used. The SCOPE study is a multicenter prospective cohort study in community-dwelling adults (≥75 years) [19]. Data for the present analysis refer to the 24-month visit.
For the present analysis, only participants without major cognitive impairment as defined by a Mini Mental Status Examination (MMSE) score of ≥24 points of max. 30 points, plausible energy intake (mean energy intake ±3 standard deviations of sample mean) and with complete data on both the Protein Screener and the reference method (dietary record), were included. For the purpose of this validation study no a priori sample size calculation was performed.
As reference method, an estimated consecutive 3-day-dietary-record was used [8]. The dietary records did not include predefined food groups but had open fields to list all foods eaten. Participants were advised to stick to their usual eating habits and to report all consumed foods and beverages as detailed as possible, including portion sizes (e.g. grams, usual household measures, packaging information), fat content (e.g. milk, yogurt), ingredients and quantities of recipes, cooking methods and timing of consumption.
At the study visits, participants received both the Protein Screener and the dietary record with detailed oral and written instructions for completion at home during the week after the visit. For the dietary record, the three days for completion were determined a priori together with the participants. The completed documents were sent back in prepaid envelopes and checked for completeness and plausibility by a nutrition scientist or dietitian. Missing or implausible information was clarified by phone within one week after arrival. Data of the 3-day dietary records were entered in EBISpro-software (EBISpro, Willstätt-Legelshurst, Germany, 2016) by a trained nutrition scientist or dietitian to calculate intake of protein (g), and in addition of energy (kilocalories (kcal)), fat (g) and carbohydrates (g) per day based on the German nutrient database “Bundeslebensmittelschlüssel” (version 3.02, Karlsruhe, Germany). All entered data were cross-checked by a second nutrition scientist and mean values of the three days were used for analysis.
Protein intake is presented in g/kg aBW/d to consider reduced protein needs per kg body weight in overweight and increased protein needs per kg body weight in underweight persons [20]. Adjusted body weight was calculated for persons with BMI > 27 kg/m² and <22 kg/m² by using the body weight that corresponds to a BMI of 27 kg/m² or 22 kg/m², respectively [16]. Low protein intake was defined by either <1.0 g/kg aBW/d or <0.8 g/kg aBW/d – the same thresholds as described by Wijnhoven et al. (2018).
Further measurements
Participants’ characteristics
Sex, age, and living situation (living alone vs. living with others) were assessed through standardized questionnaires. Illness burden was evaluated by the study physician using the Cumulative Illness Rating Scale for Geriatrics (CIRS-G), rating 14 disease categories on a scale from 0 (no problem) to 4 (extremely severe) [21].
Functional status was measured using the Short Physical Performance Battery (SPPB; 0–12 points) with tests on standing balance, usual gait speed, and lower extremity strength (chair rise test) [22]. An SPPB score ≤9 points was defined as poor performance [23].
Handgrip strength (kg) was measured with a JAMAR hydraulic hand dynamometer (Sammons Preston Rolyan, Bolingbrook, IL, USA) in a seated position according to the study specific standard operating procedures. The maximal value of the dominant hand was used.
For calculating body mass index (BMI, kg/m²) body weight was measured in light clothes with calibrated scales and body height with a stadiometer. Nutritional status was evaluated using the Mini Nutritional Assessment Short Form (MNA-SF, 0–14 points) and categorized as normal (12–14 points), at risk of malnutrition (8–11 points), and malnourished (0–7 points) [24].
Statistical analyses
Participant characteristics and intake data are presented as relative frequencies for nominal and ordinal variables or as mean±standard deviation for continuous variables for the total sample and stratified by protein intake (<, ≥1.0 g/kg aBW/d) and gender. Group differences were tested by the Mann–Whitney-U-Test or Chi²-test. To identify potential country differences, the questionnaire responses were compared to the original validation study from the Netherlands using the provided data of the Longitudinal Aging Study Amsterdam (LASA) (n = 1348).
For the validation of the German version of the Protein Screener 55+, we calculated the predicted probability of low protein intake for each participant by using the equation provided by Wijnhoven et al. (2018) (supplementary material 1). We tested the performance of the equation using receiver operating characteristic (ROC) curves. Discriminative ability is considered good with an area under the curve (AUC) > 0.8. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated for different probability cut-offs (0.3, 0.5, 0.7) and using <1 g protein/kg aBW as reference value. An additional analysis was conducted with <0.8 g protein/kg aBW to define low protein intake.
Statistical analyses were performed with SPSS version 26 (IBM SPSS Statistics, Chicago, IL, USA).
Results
Participants
The Protein Screener was completed by 161 participants. Seventeen participants were excluded from analysis due to MMSE score <24 points (n = 4), tube feeding (n = 1), implausible energy intake (n = 1) or incomplete data (n = 11). Therefore, the final sample comprised 144 participants.
Mean age of participants was 81.6 ± 3.9 years, nearly two thirds were female (61.8%) and one third (34%) had a poor functional status (Table 1). Participants’ characteristics did not differ between groups with low and sufficient protein intake (Table 1).
Dietary intake
Mean energy intake was 1770.1 ± 440.4 kcal/d and was higher in those with sufficient protein intake than in those with low protein intake (Table 2) as well as in males than in females (supplementary material 2). Mean protein intake amounted 1.0 ± 0.3 g/kg aBW/d. Protein intake <1.0 g/kg aBW/d was present in 39.6% of the sample and <0.8 g/kg aBW/d in 17.4%, respectively.
Protein Screener
The result of the Protein Screener, expressed as median (interquartile range) predicted probability, was 0.17 (0.04–0.46). In participants with protein intake <1.0 g/kg aBW/d the predicted probability was significantly higher compared to those with sufficient protein intake (0.31 (0.08–0.68) vs. 0.13 (0.02–0.41), p = 0.015). The responses to the single items of the Protein Screener in comparison to the Dutch validation study are presented in supplementary material 3.
Validation
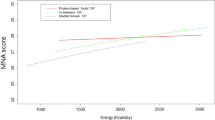
When applying a protein intake of 1.0 g/kg aBW/d as reference value, the AUC was 62.0% (95%CI 52.6–71.5), indicating low discriminative abilities of the Protein Screener (Fig. 1). Highest sensitivity + specificity was found for the probability cut-off value of 0.17 (sensitivity: 63.2% (95%CI 50.3–74.9); specificity: 57.5% (95%CI 47.0–67.5); PPV 49.3% (95%CI 38.0–60.7); NPV 70.4% (95%CI 59.2–80.2)). Sensitivity, specificity, PPV and NPV for further probability cut-off values are presented in Table 3. Sensitivity of the Protein Screener to identify participants with protein intake <1.0 g/kg aBW/d was generally low. Moderate specificity was identified for probability cut-offs 0.5 (specificity: 83.9% (95%CI 75.3–90.6)) and 0.7 (89.7% (95%CI 82.1–94.9)).
When using 0.8 g/kg aBW/d as reference value, the AUC was 68.8% (95%CI 58.1–79.4)) (Fig. 1). Highest sensitivity + specificity was found for the probability cut-off of 0.09 (Sensitivity: 88.0% (95%CI 71.8-96.9); Specificity: 42.0% (95%CI 33.4–51.0); PPV 24.2% (95%CI 16.2–33.6); NPV 94.3% (95%CI 86.0–98.6)). Specificity could be increased to a moderate level, when using the probability cut-offs 0.5 and 0.7 (Table 4).
Discussion
We have translated the Protein Screener 55+ to German and tested its discriminative accuracy in detecting low protein intake of older community-dwelling people living in the Region of Nuremberg in Southern Germany. Based on the AUCs, the German version’s ability to discriminate between low and sufficient protein intake – for both 1.0 g/kg aBW/d and 0.8 g/kg aBW/d thresholds – was poor. The 0.3-probability cut-off that was recommended based on the best trade-off between sensitivity and specificity in the original validation study [16], did not distinguish well between older people with low and sufficient protein intake in our study. We were not able to identify probability cut-off values with moderate or high levels of both sensitivity and specificity.
As the result of the Protein Screener is expressed as predicted probability, that can take values between 0 and 1, it is possible to use specific cut-off values according to the purpose of the screening (i.e. ruling in or ruling out a condition) [16, 25]. A low probability cut-off should be used when high sensitivity is important, meaning not to miss any individuals with low protein intake [16, 25]. In our study, with a very low probability cut-off of 0.09 (best trade-off between sensitivity and specificity), it was possible to classify 88% of the older people with protein intake below 0.8 g/kg aBW/d correctly. With regard to the reference threshold of 1.0 g/kg aBW/d, the sensitivity of the Protein Screener was poor – even when applying low probability cut-offs. The slightly better performance of the Protein Screener when using the lower protein threshold might be explained by the fact that it is easier to detect more severe stages of a condition (<0.8 g/kg aBW/d) [26]. The use of higher probability cut-offs increases specificity and is recommended when it is crucial to have few false positive cases [16, 25]. For purposes of identifying older individuals with sufficient protein intake, the Protein Screener seems somewhat better suited. When applying probability cut-offs of 0.5 or 0.7, specificity reached 82–90% in the current sample (Tables 3–4). From a public health perspective, the screener may thus be used to filter out individuals with sufficient protein intake. The remaining individuals would then need a detailed dietary assessment to determine the actual protein intake.
Compared to the Dutch validation study [16] the discriminative properties of the German version were distinctly lower. These deviating results are likely caused by several reasons that are discussed in the following.
Firstly, some methodological differences regarding the used reference method need to be acknowledged. Originally, the Protein Screener was developed data-driven based on the semi-quantitative HELIUS FFQ, which refers to the consumption of food items in the last four weeks [17]. Accordingly, the same items are incorporated in the Protein Screener as well as in the original reference standard, which may partially explain the higher agreement between these tools [26]. In the present study, a 3-day dietary record was used as reference standard that documents current intake. Albeit the Protein Screener and the dietary record were assessed in parallel, the periods the intake data refer to did not overlap, which may have affected the results. However, eating habits of older people are generally considered relatively stable [27, 28]. Moreover, the agreement between FFQs and dietary records as methods to assess protein intake was characterized as low to adequate in previous studies [29,30,31,32,33,34]. The HELIUS FFQ was specifically validated in older people (72 ± 9 years), and for intake of energy and macronutrients, an acceptable to good relative validity compared to 24 h recalls was described [35]. For protein intake, the group level bias between the methods was 4.7% and the Pearson correlation coefficient amounted to 0.39 [35]. On the level of food intake, the HELIUS FFQ overestimated the intake of fish, eggs, dairy products and nuts/seeds compared to the 24 h recalls items that are also included in the Protein Screener. It can be assumed, that 24 h recalls and 3-day dietary records may not depict usual intake of food groups such as fish and eggs that are typically not eaten daily [35].
Secondly, participant selection may have affected test accuracy [26]. The sample in the present study had a distinctly higher mean age compared to that of the Dutch validation study (82 ± 4 years vs. 62 ± 4 years) [16]. Even though cognitive status was overall good – expressed by a mean MMSE score of 28 points – completing the questionnaires might be more challenging for people of advanced age bearing the risk of a recall bias [36]. A format, where the screener is conducted as an interview by trained personnel might be an option to increase accuracy. The higher age might also have affected portion sizes and eating behavior due to decreased appetite, earlier satiety or functional impairments [27, 37,38,39]. Therefore, the portion sizes taken as basis for the screener might be larger compared to real portions of our participants. Further, the proportion of older people with low protein intake was higher in the present study compared to the Dutch validation study (<1.0 g/kg aBW/d: 40% vs. ~30%; <0.8 g/kg aBW/d: 17% vs. ~10%), which may also be explained by aspects like higher age and limited functional abilities [40, 41]. The high prevalence of older people with low protein intake as observed in our study underlines the need for appropriate screening tools. One quarter of participants in our study was obese; the proportion was slightly higher in those with low protein intake while energy intake was lower in participants with obesity. Even though we checked all dietary records thoroughly, this could be an indicator for underreporting in older people with obesity, which has been described previously [42]. However, sensitivity and specificity in subgroups of participants with BMI < and ≥30 kg/m² did not differ markedly (data not shown).
Thirdly, potential cultural differences in food intake between older people from Germany and the Netherlands may have affected the results. Comparing the responses to the single Protein Screener items between the Dutch and the current study (supplementary material 3) indicates that the chosen protein sources are relevant for protein intake in both countries. Some differences e.g. in the portion size of meat with a warm dish might be explained by different sample compositions regarding sex and age. Two recent publications from Germany (D) and the Netherlands (NL) showed similar contributions of animal and plant protein to total daily protein intake in older adults with a mean age >70 years [43, 44]. In both studies, main protein sources were meat/meat products (NL: 23% vs. D: 24%), cereals/starchy foods (NL: 19% vs. D: 21%) and dairy products (NL: 26% vs. D: 20%) [43, 44]. The contribution of dairy products appeared to be slightly higher in Dutch compared to German older people. A recent analysis of the SHARE database supports this assumption reporting a higher frequency of dairy product consumption at every day of the week in Dutch compared to German older adults [45]. However, this difference could not be seen in the answers to the four Protein Screener items referring to dairy products. For few items e.g. pasta, the category referring to the most frequent consumption was more pronounced in our compared to the Dutch study, which might have led to an underestimation of protein intake by this source. However, this effect is considered marginal. It remains to be investigated if exchanging certain items of the Protein Screener by protein sources more commonly consumed in Germany e.g. potatoes, legumes or cold meat could improve the precision of the German Screener version.
Further, as no a priori sample size calculation was performed, a too small sample size might have influenced the validation results. However, following the guidance for determining the minimum sample size required for a screening study [46], a minimum sample size of 122 participants, including n = 49 with low protein intake as determined by our reference standard (3-day dietary record; prevalence of ~40% for low protein intake <1 g/kg aBW/d), would have been sufficient to achieve 80% power for detecting a change in the percentage value of sensitivity from 50% (chance) to 70% based on an alpha error level of 5%.
Conclusions
The overall discriminative accuracy of the German version of Protein Screener 55+ to identify older community-dwelling people with low protein intake was poor compared to the reference standard of a 3-day dietary record. However, applying different probability cut-offs increased specificity and sensitivity for 0.8 g/kg aBW/d to sufficient levels justifying the use for certain purposes e.g. identifying individuals with sufficient intake in order to exclude them from an in-depth and time-consuming nutritional assessment to determine actual protein intake. Further validation studies in samples with a broader age range, using different reference methods, applying modified versions by exchanging single items or comparing different application methods i.e. paper-pencil vs. interview are needed.
Data availability
Data described in the manuscript are available from the corresponding author on reasonable request.
References
Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87:150–5.
Mendonca N, Granic A, Hill TR, Siervo M, Mathers JC, Kingston A, et al. Protein Intake and Disability Trajectories in Very Old Adults: The Newcastle 85+ Study. J Am Geriatr Soc. 2019;67:50–6.
Burd NA, Gorissen SH, van Loon LJ. Anabolic resistance of muscle protein synthesis with aging. Exerc Sport Sci Rev. 2013;41:169–73.
Gorissen SHM, Witard OC. Characterising the muscle anabolic potential of dairy, meat and plant-based protein sources in older adults. Proc Nutr Soc. 2018;77:20–31.
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14:542–59.
Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. 2014;33:929–36.
Richter M, Baerlocher K, Bauer JM, Elmadfa I, Heseker H, Leschik-Bonnet E, et al. Revised Reference Values for the Intake of Protein. Ann Nutr Metab. 2019;74:242–50.
Gingrich A, Spiegel A, Kob R, Schoene D, Skurk T, Hauner H, et al. Amount, Distribution, and Quality of Protein Intake Are Not Associated with Muscle Mass, Strength, and Power in Healthy Older Adults without Functional Limitations-An enable Study. Nutrients 2017;9:1358.
Houston DK, Tooze JA, Garcia K, Visser M, Rubin S, Harris TB, et al. Protein Intake and Mobility Limitation in Community-Dwelling Older Adults: the Health ABC Study. J Am Geriatr Soc. 2017;65:1705–11.
Hengeveld LM, Boer JMA, Gaudreau P, Heymans MW, Jagger C, Mendonça N, et al. Prevalence of protein intake below recommended in community-dwelling older adults: a meta-analysis across cohorts from the PROMISS consortium. J Cachexia Sarcopenia Muscle. 2020;11:1212–22.
Ten Haaf DSM, Nuijten MAH, Maessen MFH, Horstman AMH, Eijsvogels TMH, Hopman MTE. Effects of protein supplementation on lean body mass, muscle strength, and physical performance in nonfrail community-dwelling older adults: a systematic review and meta-analysis. Am J Clin Nutr. 2018;108:1043–59.
Tieland M, Franssen R, Dullemeijer C, van Dronkelaar C, Kyung Kim H, Ispoglou T, et al. The Impact of Dietary Protein or Amino Acid Supplementation on Muscle Mass and Strength in Elderly People: Individual Participant Data and Meta-Analysis of RCT’s. J Nutr Health Aging. 2017;21:994–1001.
Thompson FE, Subar AF Chapter 1 - Dietary Assessment Methodology. In: Coulston AM, Boushey CJ, Ferruzzi MG, Delahanty LM, editors. Nutrition in the Prevention and Treatment of Disease (Fourth Edition): Academic Press; 2017. p. 5–48.
Volkert D, Schrader E. Dietary assessment methods for older persons: what is the best approach? Curr Opin Clin Nutr Metab Care. 2013;16:534–40.
McNeill G, Winter J, Jia X. Diet and cognitive function in later life: a challenge for nutrition epidemiology. Eur J Clin Nutr. 2009;63(Suppl 1):S33–7.
Wijnhoven HAH, Elstgeest LEM, de Vet HCW, Nicolaou M, Snijder MB, Visser M. Development and validation of a short food questionnaire to screen for low protein intake in community-dwelling older adults: The Protein Screener 55+ (Pro55+). PLoS One. 2018;13:e0196406.
Beukers MH, Dekker LH, de Boer EJ, Perenboom CW, Meijboom S, Nicolaou M, et al. Development of the HELIUS food frequency questionnaires: ethnic-specific questionnaires to assess the diet of a multiethnic population in The Netherlands. Eur J Clin Nutr. 2015;69:579–84.
Landi F, Cesari M, Calvani R, Cherubini A, Di Bari M, Bejuit R, et al. The “Sarcopenia and Physical fRailty IN older people: multi-componenT Treatment strategies” (SPRINTT) randomized controlled trial: design and methods. Aging Clin Exp Res. 2017;29:89–100.
Corsonello A, Tap L, Roller-Wirnsberger R, Wirnsberger G, Zoccali C, Kostka T, et al. Design and methodology of the screening for CKD among older patients across Europe (SCOPE) study: a multicenter cohort observational study. BMC Nephrol. 2018;19:260.
Berner LA, Becker G, Wise M, Doi J. Characterization of dietary protein among older adults in the United States: amount, animal sources, and meal patterns. J Acad Nutr Dietetics. 2013;113:809–15.
Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–48.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–31.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13:782–8.
Trevethan R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front Public Health. 2017;5:307.
Schmidt RL, Factor RE. Understanding sources of bias in diagnostic accuracy studies. Arch Pathol Lab Med. 2013;137:558–65.
de Castro JM. Age-related changes in the social, psychological, and temporal influences on food intake in free-living, healthy, adult humans. J Gerontol A Biol Sci Med Sci. 2002;57:M368–77.
Gingrich A, Rennekamp R, Brandl B, Skurk T, Hauner H, Sieber CC, et al. Do Aspects of Protein Intake Vary Across the Week in Healthy Community-Dwelling Older Adults?-An enable Study. Nutrients. 2018;10:1217.
Erkkilä AT, Järvinen R, Karvonen H, Keronen L, Tuppurainen MT. Validation of a semi-quantitative FFQ using food records as a reference in older women in the Kuopio Fracture Prevention Study (OSTPRE-FPS). Public Health Nutr. 2012;15:635–9.
Shatenstein B, Nadon S, Godin C, Ferland G. Development and validation of a food frequency questionnaire. Can J Diet Pr Res. 2005;66:67–75.
Talegawkar SA, Tanaka T, Maras JE, Ferrucci L, Tucker KL. Validation of Nutrient Intake Estimates Derived Using a Semi-Quantitative FFQ against 3 Day Diet Records in the Baltimore Longitudinal Study of Aging. J Nutr Health Aging. 2015;19:994–1002.
Kobayashi S, Yuan X, Sasaki S, Osawa Y, Hirata T, Abe Y, et al. Relative validity of brief-type self-administered diet history questionnaire among very old Japanese aged 80 years or older. Public Health Nutr. 2019;22:212–22.
Smith W, Mitchell P, Reay EM, Webb K, Harvey PW. Validity and reproducibility of a self-administered food frequency questionnaire in older people. Aust N. Z J Public Health. 1998;22:456–63.
Horwath CC. Validity of a short food frequency questionnaire for estimating nutrient intake in elderly people. Br J Nutr. 1993;70:3–14.
Visser M, Elstgeest LEM, Winkens LHH, Brouwer IA, Nicolaou M. Relative Validity of the HELIUS Food Frequency Questionnaire for Measuring Dietary Intake in Older Adult Participants of the Longitudinal Aging Study Amsterdam. Nutrients. 2020;12:1998.
Knäuper B, Carrière K, Chamandy M, Xu Z, Schwarz N, Rosen NO. How aging affects self-reports. Eur J Ageing. 2016;13:185–93.
Giezenaar C, Chapman I, Luscombe-Marsh N, Feinle-Bisset C, Horowitz M, Soenen S. Ageing Is Associated with Decreases in Appetite and Energy Intake-A Meta-Analysis in Healthy Adults. Nutrients. 2016;8:28.
Shahar D, Fraser D, Shai I, Vardi H. Development of a food frequency questionnaire (FFQ) for an elderly population based on a population survey. J Nutr. 2003;133:3625–9.
Yannakoulia M, Mamalaki E, Anastasiou CA, Mourtzi N, Lambrinoudaki I, Scarmeas N. Eating habits and behaviors of older people: Where are we now and where should we go? Maturitas. 2018;114:14–21.
Berryman CE, Lieberman HR, Fulgoni VL 3rd, Pasiakos SM. Protein intake trends and conformity with the Dietary Reference Intakes in the United States: analysis of the National Health and Nutrition Examination Survey, 2001-2014. Am J Clin Nutr. 2018;108:405–13.
Coelho-Junior HJ, Milano-Teixeira L, Rodrigues B, Bacurau R, Marzetti E, Uchida M. Relative Protein Intake and Physical Function in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2018;10:1330.
Tomoyasu NJ, Toth MJ, Poehlman ET. Misreporting of total energy intake in older men and women. J Am Geriatr Soc. 1999;47:710–5.
Gingrich A, Spiegel A, Gradl JE, Skurk T, Hauner H, Sieber CC, et al. Daily and per-meal animal and plant protein intake in relation to muscle mass in healthy older adults without functional limitations: an enable study. Aging Clin Exp Res. 2018;31:1271–81.
Tieland M, Borgonjen-Van den Berg KJ, Van Loon LJ, de Groot LC. Dietary Protein Intake in Dutch Elderly People: A Focus on Protein Sources. Nutrients 2015;7:9697–706.
Ribeiro I, Gomes M, Figueiredo D, Lourenço J, Paúl C, Costa E. Dairy Product Intake in Older Adults across Europe Based On the SHARE Database. J Nutr Gerontol Geriatr. 2019;38:297–306.
Bujang MA, Adnan TH. Requirements for Minimum Sample Size for Sensitivity and Specificity Analysis. J Clin Diagn Res. 2016;10:YE01–YE06.
Acknowledgements
We like to thank the study staff of the SPRINT-T and the SCOPE study from the study center in Nuremberg for their support. The study was supported by a grant of the Karl-Düsterberg-Stiftung. The foundation had no role in the design of the study, used methods, participant recruitment, data collections, analysis and preparation of the paper. The contributions of HAHW and MV were funded by EU Horizon 2020 PROMISS Project ‘Prevention Of Malnutrition In Senior Subjects in the EU’, Grant agreement no. 678732.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
EK, DV conceptualization. EK, HS, DS, DV methodology. EK, HS investigation. HAHW data curation. HS, HAHW, MV, RK, CCS, EF resources. EK formal analysis. EK, DV funding acquisition. EK project administration. EK writing original draft. EK visualization. EK, DS, HS, RK, EF, CCS, MV, HAHW, DV writing review & editing.
Corresponding author
Ethics declarations
Competing interests
EK, HS, DS, RK, EF, MV, HAHW and DV declare no conflicts of interest. CCS has received honoraria for lectures and presentations for Abbott, Nestlé, Nutricia, Pfizer and Novartis.
Ethical approval
The studies were performed according to the guidelines published in the Declaration of Helsinki and the study protocols were approved by the ethics committee of the Friedrich-Alexander-University Erlangen-Nürnberg, Germany (SPRINT-T 191_15B, SCOPE 340_15B). Written informed consent was obtained from every participant prior to the start of the studies.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kiesswetter, E., Siebentritt, H.M., Schoene, D. et al. Validation of the German version of the Protein Screener 55+. Eur J Clin Nutr 77, 579–585 (2023). https://doi.org/10.1038/s41430-023-01266-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01266-y