Abstract
Background
Breakfast quality in early childhood remains understudied. This study describes the changes in breakfast quality index (BQI) (i.e. trajectory) in early childhood and assesses its associations with obesity outcomes.
Methods
Data from children who participated in the Melbourne InFANT Program were used (n = 328). The Melbourne InFANT Program was a 15-month early obesity prevention intervention conducted from 2008 to 2013. Dietary intakes at ages 1.5, 3.5 and 5.0 years were assessed using three parent-proxy reported 24 h recalls. A revised nine-item BQI tool developed based on Australian dietary recommendations for young children was used to calculate BQI scores. Group-based trajectory modelling identified BQI trajectory groups. Multivariable linear and logistic regression examined the associations between identified BQI trajectory groups and obesity outcomes at age 5 years.
Results
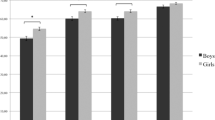
Mean BQI at ages 1.5, 3.5 and 5.0 years was 4.8, 4.8, 2.7 points, respectively. Two BQI trajectory groups were identified, and both showed a decline in BQI. The mean BQI of most children (74%) decreased from 5.0 to 4.0 points from ages 1.5 to 5.0 years (referred as “High BQI” group). The remaining children (26%) had a mean BQI of 4.8 and 1.2 points at age 1.5 and 5.0 years, respectively (referred as “Low BQI” group). The “Low BQI” group appeared to show higher risk of overweight (OR:1.30, 95% CI: 0.60, 2.81, P = 0.66) at age 5 years than the “High BQI” group. No difference in body mass index (BMI) z-score was found between the two groups.
Conclusions
Two BQI trajectory groups were identified. Both groups showed a decline in breakfast quality from ages 1.5 to 5.0 years. Our study highlights the need for early health promotion interventions and strategies to improve and maintain breakfast quality across early childhood.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
World Health Organization (WHO). Report of the Commission on Ending Childhood Obesity. In: Geneva, Switzerland. 2017.
World Health Organization (WHO). Obesity and overweight. In: Geneva, Switzerland. 2021..
Australian Institute of Health and Welfare (AIHW). Overweight and obesity among Australian children and adolescents. In: Canberra, Australia. 2020.
Weihrauch-Blüher S, Wiegand S. Risk Factors and Implications of Childhood Obesity. Curr Obes Rep. 2018;7:254–9. https://doi.org/10.1007/s13679-018-0320-0
Australian Institute of Health and Welfare (AIHW). Overweight and obesity. In: Canberra, Australia. 2022.
Koletzko B, Brands B, Poston L, Godfrey K, Demmelmair H. Early nutrition programming of long-term health. Proc Nutr Soc. 2012;71:371–8. https://doi.org/10.1017/s0029665112000596. e-pub ahead of print 2012/06/19
Mikkilä V, Räsänen L, Raitakari O, Pietinen P, Viikari J. Consistent dietary patterns identified from childhood to adulthood: the cardiovascular risk in Young Finns Study. Br J Nutr. 2005;93:923–31.
Spence C. Breakfast: the most important meal of the day? Int J gastronomy food Sci. 2017;8:1–6.
Alexy U, Wicher M, Kersting M. Breakfast trends in children and adolescents: frequency and quality. Public Health Nutr. 2010;13:1795–802.
Rampersaud GC. Benefits of Breakfast for Children and Adolescents: Update and Recommendations for Practitioners. Am J Lifestyle Med. 2009;3:86.
Gibney MJ, Barr SI, Bellisle F, Drewnowski A, Fagt S, Livingstone B, et al. Breakfast in Human Nutrition: The International Breakfast Research Initiative. Nutrients. 2018;10:559 https://doi.org/10.3390/nu10050559
Pereira MA, Erickson E, McKee P, Schrankler K, Raatz SK, Lytle LA, et al. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J Nutr. 2011;141:163–8.
Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III. J Am Coll Nutr. 2003;22:296–302. https://doi.org/10.1080/07315724.2003.10719307. E-pub ahead of print 2003/08/05.
Wyatt HR, Grunwald GK, Mosca CL, Klem ML, Wing RR, Hill JO. Long‐term weight loss and breakfast in subjects in the National Weight Control Registry. Obes Res. 2002;10:78–82.
Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? J Am Dietetic Assoc. 2005;105:1373–82.
Summerbell C, Moody R, Shanks J, Stock M, Geissler C. Relationship between feeding pattern and body mass index in 220 free-living people in four age groups. Eur J Clin Nutr. 1996;50:513–9.
Shang X, Li Y, Xu H, Zhang Q, Hu X, Liu A, et al. Healthy breakfast habits and changes in obesity-related cardiometabolic markers in children: a longitudinal analysis. Eur J Clin Nutr. 2020;74:1685–97.
Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics. 2008;121:e638–e645.
Alsharairi NA, Somerset SM. Skipping breakfast in early childhood and its associations with maternal and child BMI: a study of 2-5-year-old Australian children. Eur J Clin Nutr. 2016:450. https://doi.org/10.1038/ejcn.2015.184
Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster-randomised controlled trial. BMC Public Health. 2008;8:1–9.
Campbell KJ, Lioret S, McNaughton SA, Crawford DA, Salmon J, Ball K, et al. A parent-focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics. 2013;131:652–60.
Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster-randomised controlled trial. BMC Public Health. 2008;8:103.
Hesketh KD, Campbell K, Salmon J, McNaughton SA, McCallum Z, Cameron A, et al. The Melbourne infant feeding, activity and nutrition trial (InFANT) program follow-up. Contemp Clin Trials. 2013;34:145–51.
Zheng M, Campbell KJ, Scanlan E, McNaughton SA. Development and evaluation of a food frequency questionnaire for use among young children. PloS ONE. 2020;15:e0230669.
Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–8.
Food Standards Australia New Zealand (FSANZ). AUSNUT 2007. In: Canberra, Australia. 2007.
Thompson FE, Subar AF. Dietary assessment methodology. Nutrition in the Prevention and Treatment of Disease. 2017;5–48..
Leech RM, Worsley A, Timperio A, McNaughton SA. Characterizing eating patterns: a comparison of eating occasion definitions. Am J Clin Nutr. 2015;102:1229–37. https://doi.org/10.3945/ajcn.115.114660
Monteagudo C, Palacin-Arce A, del Mar Bibiloni M, Pons A, Tur JA, Olea-Serrano F, et al. Proposal for a Breakfast Quality Index (BQI) for children and adolescents. Public Health Nutr. 2013;16:639–44.
National Health and Medical Research Council (NHMRC). Nutrient Reference Values. In: Canberra, Australia. 2020.
Harttig U, Haubrock J, Knüppel S, Boeing H. The MSM program: web-based statistics package for estimating usual dietary intake using the Multiple Source Method. Eur J Clin Nutr. 2011;65:S87–S91.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica. 2006;95:76–85.
Kêkê L, Samouda H, Jacobs J, Di Pompeo C, Lemdani M, Hubert H, et al. Body mass index and childhood obesity classification systems: A comparison of the French, International Obesity Task Force (IOTF) and World Health Organization (WHO) references. Rev d’epidemiologie et de sante publique. 2015;63:173–82.
Silva LM, van Rossem L, Jansen PW, Hokken-Koelega ACS, Moll HA, Hofman A, et al. Children of Low Socioeconomic Status Show Accelerated Linear Growth in Early Childhood; Results from the Generation R Study. PLOS ONE. 2012;7:e37356 https://doi.org/10.1371/journal.pone.0037356
Fernando NN, Campbell KJ, McNaughton SA, Zheng M, Lacy KE. Predictors of dietary energy density among preschool aged children. Nutrients. 2018;10:178.
Zheng M, Cameron AJ, Birken CS, Keown‐Stoneman C, Laws R, Wen LM, et al. Early infant feeding and BMI trajectories in the first 5 years of life. Obesity. 2020;28:339–46.
National Health and Medical Research Council (NHMRC). Infant Feeding Guidelines: Summary. In: Canberra, Australia. 2013.
Zheng M, Lioret S, Hesketh KD, Spence A, Taylor R, Campbell KJ. Association Between Longitudinal Trajectories of Lifestyle Pattern and BMI in Early Childhood. Obesity. 2021;29:879–87.
Zheng M, Campbell KJ, Baur L, Rissel C, Wen LM. Infant feeding and growth trajectories in early childhood: the application and comparison of two longitudinal modelling approaches. Int J Obes (Lond). 2021;45:2230–7. https://doi.org/10.1038/s41366-021-00892-5. e-pub ahead of print 2021/07/08
Zheng M, Hesketh KD, Wu JHY, Heitmann BL, Downing K, Campbell KJ. Nighttime sleep duration trajectories were associated with body mass index trajectories in early childhood. Pediatr Obes. 2021;16:e12766 https://doi.org/10.1111/ijpo.12766
Morales IF, Vilas MA, Vega CM, Para MCM. Breakfast quality and its relationship to the prevalence of overweight and obesity in adolescents in Guadalajara (Spain). Nutrición Hospitalaria. 2011;26:952–8.
Defeyter MA, Graham PL, Walton J, Apicella T. Breakfast clubs: availability for British schoolchildren and the nutritional, social and academic benefits. Nutr Bull. 2010;35:245–53. https://doi.org/10.1111/j.1467-3010.2010.01843.x
Hassan BK, Cunha DB, da Veiga GV, Pereira RA, Sichieri R. Changes in breakfast frequency and composition during adolescence: The Adolescent Nutritional Assessment Longitudinal Study, a cohort from Brazil. PloS ONE. 2018;13:e0200587.
Zheng M, Wu JHY, Louie JCY, Flood VM, Gill T, Thomas B, et al. Typical food portion sizes consumed by Australian adults: results from the 2011-12 Australian National Nutrition and Physical Activity Survey. Sci Rep. 2016;6:19596–19596. https://doi.org/10.1038/srep19596
Smith KJ, Breslin MC, McNaughton SA, Gall SL, Blizzard L, Venn AJ. Skipping breakfast among Australian children and adolescents; findings from the 2011–12 National Nutrition and Physical Activity Survey. Aust NZ J Public Health. 2017;41:572–8.
Scaglioni S, De Cosmi V, Ciappolino V, Parazzini F, Brambilla P, Agostoni C. Factors influencing children’s eating behaviours. Nutrients. 2018;10:706.
Cole NC, An R, Lee S-Y, Donovan SM. Correlates of picky eating and food neophobia in young children: a systematic review and meta-analysis. Nutr Rev. 2017;75:516–32.
Nicklaus S. The role of food experiences during early childhood in food pleasure learning. Appetite. 2016;104:3–9.
Fletcher S, Wright C, Jones A, Parkinson K, Adamson A. Tracking of toddler fruit and vegetable preferences to intake and adiposity later in childhood. Matern Child Nutr. 2017;13:e12290 https://doi.org/10.1111/mcn.12290
Moding KJ, Fries LR. Feeding practices demonstrated by parents of toddlers: An observational analysis of breakfast, lunch, dinner, and snacks. Appetite. 2020;155:104825 https://doi.org/10.1016/j.appet.2020.104825
Reyes LI, Frongillo EA, Moore S, Blake CE, Gonzalez W, Bonvecchio A. Functions of social networks in maternal food choice for children in Mexico. Matern Child Nutr. 2022;18:e13263 https://doi.org/10.1111/mcn.13263
Hulshof K, Brussaard J, Kruizinga A, Telman J, Löwik M. Socio-economic status, dietary intake and 10 y trends: the Dutch National Food Consumption Survey. Eur J Clin Nutr. 2003;57:128–37.
Alsharairi NA, Somerset S. Parental work status and children’s dietary consumption: Australian evidence. Int J Consum Stud. 2018;42:522–32.
Aranceta J, Serra-Majem L, Ribas L, Pérez-Rodrigo C. Breakfast consumption in Spanish children and young people. Public Health Nutr. 2001;4:1439–44.
Liu S, Willett WC, Manson JE, Hu FB, Rosner B, Colditz G. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. Am J Clin Nutr. 2003;78:920–7.
Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J. 2000;14:1132–8.
Pereira MA, Erickson E, McKee P, Schrankler K, Raatz SK, Lytle LA, et al. Breakfast Frequency and Quality May Affect Glycemia and Appetite in Adults and Children. J Nutr. 2010;141:163–8. https://doi.org/10.3945/jn.109.114405
Dougkas A, Barr S, Reddy S, Summerbell CD. A critical review of the role of milk and other dairy products in the development of obesity in children and adolescents. Nutr Res Rev. 2019;32:106–27.
Spence LA, Cifelli CJ, Miller GD. The role of dairy products in healthy weight and body composition in children and adolescents. Curr Nutr Food Sci. 2011;7:40–9.
Stokes A, Campbell KJ, Yu H-J, Szymlek-Gay EA, Abbott G, He Q-Q, et al. Protein Intake from Birth to 2 Years and Obesity Outcomes in Later Childhood and Adolescence: A Systematic Review of Prospective Cohort Studies. Adv Nutr. 2021;12:1863–76. https://doi.org/10.1093/advances/nmab034
Rocandio A, Ansotegui L, Arroyo M. Comparison of dietary intake among overweight and non-overweight schoolchildren. Int J Obes. 2001;25:1651–5.
Rodríguez G, Moreno LA. Is dietary intake able to explain differences in body fatness in children and adolescents? Nutr Metab Cardiovasc Dis. 2006;16:294–301.
McMurray RG, Harrell JS, Creighton D, Wang Z, Bangdiwala SI. Influence of physical activity on change in weight status as children become adolescents. Int J Pediatr Obes. 2008;3:69–77.
Department of Education and Training. Expanded School Breakfast Clubs program. In: State of Victoria, Australia. 2020.
Acknowledgements
We acknowledge the contribution of the parents and children who participated in the Melbourne InFANT Study.
Author information
Authors and Affiliations
Contributions
Conceptualisation: MZ, PL, KL, KC. Data curation: MZ, KL, SP. Formal analysis: MZ, SP. Project administration: MZ. Resources: MZ. KC. Software: MZ, SP. Supervision: MZ, PL, KL, KC. Writing original draft: SP. Writing review and editing: MZ, PL, KL, KC.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, S.Y., Love, P., Lacy, K.E. et al. Describing the longitudinal breakfast quality index trajectories in early childhood: results from Melbourne InFANT program. Eur J Clin Nutr 77, 363–369 (2023). https://doi.org/10.1038/s41430-022-01249-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01249-5