Abstract
Background
The current study examines the association between the Dietary Diversity Score (DDS) and nonalcoholic fatty liver disease (NAFLD) in Iranian adults using structural equation modeling (SEM).
Methods
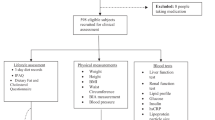
A sample of 3220 adults from the Amol Cohort Study was recruited for this cross-sectional study. Dietary acid load (DAL) and DDS were calculated using the data obtained from a validated food frequency questionnaire. Anthropometric parameters, blood pressure, biochemical measurements, and liver ultrasonography were evaluated according to standard protocols.
Results
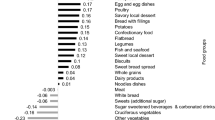
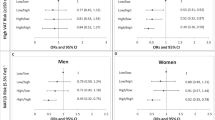
DDS was neither directly nor indirectly associated with a greater prevalence of NAFLD. In the second model (DDS sub-scores model), the association of DAL with NAFLD was fully mediated through waist circumference (WC) (of DAL to WC: β = 0.14, P < 0.0001, and of WC to NAFLD: β = 0.50, P < 0.001). Vegetable and fruit diversity scores had a significant negative indirect relationship with NAFLD prevalence through DAL (β = −0.06, P = 0.001, β = −0.10, P < 0.001, respectively). Meat diversity score was positively associated with NAFLD prevalence in a full mediational process through DAL (β = 0.12, P < 0.001). The SEM fit indices suggested a reasonably adequate fit of the data to the DDS model (Χ2/df = 4.76, GFI = 0.98, AGFI = 0.97, IFI = 0.97, CFI = 0.97, RMSEA = 0.03, and SRMR = 0.02) and its sub-scores model (Χ2/df = 4.72, GFI = 0.98, AGFI = 0.97, IFI = 0.95, CFI = 0.95, RMSEA = 0.03, and SRMR = 0.02).
Conclusion
Meat diversity and lack of vegetable and fruit diversity were indirectly associated with NAFLD prevalence through DAL and WC mediators. Interventions for NAFLD may be more successful if they target a lower intake of animal protein sources and dietary diversity, particularly vegetable and fruit diversity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57.
Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–112.
Estes C, Chan HL, Chien RN, Chuang WL, Fung J, Goh GB-B, et al. Modelling NAFLD disease burden in four Asian regions—2019–2030. Alimentary Pharmacol Therapeutics. 2020;51:801–11.
Moghaddasifar I, Lankarani K, Moosazadeh M, Afshari M, Ghaemi A, Aliramezany M, et al. Prevalence of non-alcoholic fatty liver disease and its related factors in Iran. Int J Organ Transplant Med. 2016;7:149.
Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67:829–46.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Habte TY, Krawinkel M. Dietary diversity score: a measure of nutritional adequacy or an indicator of healthy diet. J Nutr Health Sci. 2016;3:303.
Conklin AI, Monsivais P, Khaw K-T, Wareham NJ, Forouhi NG. Dietary diversity, diet cost, and incidence of type 2 diabetes in the United Kingdom: a prospective cohort study. PLoS Med. 2016;13:e1002085.
Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr. 2006;9:728–36.
Golpour-Hamedani S, Rafie N, Pourmasoumi M, Saneei P, Safavi SM. The association between dietary diversity score and general and abdominal obesity in Iranian children and adolescents. BMC Endocr Disord. 2020;20:1–8.
Doustmohammadian A, Saeidlou SN, Esfandyari S, Gholizadeh E, Maadi M, Motamed N, et al. Dietary Acid Load (DAL), Glycated Hemoglobin A1c (HbA1c), and Metabolic Syndrome (MeS) Mediate the Association of the Adherence to the Dietary Approaches to Stopping Hypertension (DASH) and Mediterranean Diet (MeD) With Nonalcoholic Fatty Liver Disease. Front Nutr. 2022;9:921415. https://doi.org/10.3389/fnut.2022.921415.
Chan R, Wong VW-S, Chu WC-W, Wong GL-H, Li LS, Leung J, et al. Higher estimated net endogenous Acid production may be associated with increased prevalence of nonalcoholic Fatty liver disease in chinese adults in Hong Kong. PLoS One. 2015;10:e0122406.
Doustmohammadian A, Pishgar E, Clark CC, Sobhrakhshankhah E, Nikkhah M, Faraji AH, et al. Empirically-derived dietary patterns in relation to non-alcoholic fatty liver diseases among adult participants in Amol, Northern Iran: A Structural Equation Modeling Approach. Front Nutr. 2022;9:821544. https://doi.org/10.3389/fnut.2022.821544.
Akter S, Eguchi M, Kuwahara K, Kochi T, Ito R, Kurotani K, et al. High dietary acid load is associated with insulin resistance: The Furukawa Nutrition and Health Study. Clin Nutr. 2016;35:453–9.
Lim S, Kim J-W, Targher G. Links between metabolic syndrome and metabolic dysfunction-associated fatty liver disease. Trends Endocrinol Metab. 2021;32:500–14.
Asrih M, Jornayvaz FR. Metabolic syndrome and nonalcoholic fatty liver disease: Is insulin resistance the link? Mol Cell Endocrinol. 2015;418:55–65.
Abbasalizad Farhangi M, Nikniaz L, Nikniaz Z. Higher dietary acid load potentially increases serum triglyceride and obesity prevalence in adults: an updated systematic review and meta-analysis. PloS One. 2019;14:e0216547.
Ghaemi A, Hosseini N, Osati S, Ehrampoush E, Honarvar B, Homayounfar R. Waist circumference is a mediator of dietary pattern in Non-alcoholic fatty liver disease. Sci Rep. 2018;8:1–9.
Alavian SM, Esmaillzadeh A, Adibi P, Azadbakht L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD). Hepatitis monthly. 2013;13:e10943. https://doi.org/10.5812/hepatmon.10943.
Pasdar Y, Moradi S, Moludi J, Darbandi M, Niazi P, Nachvak SM, et al. Risk of metabolic syndrome in non-alcoholic fatty liver disease patients. Mediterranean J Nutr Metab. 2019;12:353–63.
Sberna A, Bouillet B, Rouland A, Brindisi M, Nguyen A, Mouillot T, et al. European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD) and European Association for the Study of Obesity (EASO) clinical practice recommendations for the management of non‐alcoholic fatty liver disease: evaluation of their application in people with Type 2 diabetes. Diabet Med. 2018;35:368–75.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public health Nutr. 2010;13:654–62.
Ghaffarpour M, Houshiar-Rad A & Kianfar H (1999) The Manual for Household Measures, Cooking Yields Factors and Edible Portion of Foods. Tehran: Keshaverzi Press (In persian).
Azar M, Sarkisian E. Food composition table of Iran. Tehran: National Nutrition and Food Research Institute, Shahid Beheshti University. 1980;65.
Table FC Food and nutrition information center, UnitedStates Department of Agriculture (USDA) (2019). https://fdc.nal.usda.gov (Accessed August 2021).
Kant AK, Schatzkin A, Harris TB, Ziegler RG, Block G. Dietary diversity and subsequent mortality in the first national health and nutrition examination survey epidemiologic follow-up study. Am J Clin Nutr. 1993;57:434–40.
Kant AK, Block G, Schatzkin A, Ziegler RG, Nestle M. Dietary diversity in the US population, NHANES II, 1976–1980. J Am Dietetic Assoc. 1991;91:1526–31.
Remer T, Dimitriou T, Manz F. Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am J Clin Nutr. 2003;77:1255–60.
Frassetto LA, Todd KM, Morris RC Jr, Sebastian A. Estimation of net endogenous noncarbonic acid production in humans from diet potassium and protein contents. Am J Clin Nutr. 1998;68:576–83.
Remer T, Manz F. Potential renal acid load of foods and its influence on urine pH. J Am Dietetic Assoc. 1995;95:791–7.
Du Bois D. A formula to estimate the approximate surface area if height and weight be known. Nutrition. 1989;5:303–13.
Verbraecken J, Van de Heyning P, De Backer W, Van Gaal L. Body surface area in normal-weight, overweight, and obese adults. A comparison study. Metabolism. 2006;55:515–24.
Kant AK, Graubard BI. Energy density of diets reported by American adults: association with food group intake, nutrient intake, and body weight. Int J Obes. 2005;29:950–6.
Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, et al. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr. 2005;135:273–8.
Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9:755–62.
Willett W. Nutritional Epidemiology. 3rd ed New York, NY: Oxford University Press; (2013).
Azadbakht L, Esmaillzadeh A. Dietary diversity score is related to obesity and abdominal adiposity among Iranian female youth. Public Health Nutr. 2011;14:62–9.
Osuna-Padilla I, Leal-Escobar G, Garza-García C, Rodríguez-Castellanos F. Dietary acid load: mechanisms and evidence of its health repercussions. Nefrolía (Engl Ed). 2019;39:343–54.
Abris GP, Provido SMP, Hong S, Yu SH, Lee CB, Lee JE. Association between dietary diversity and obesity in the Filipino Women’s Diet and Health Study (FiLWHEL): a cross-sectional study. PLoS One. 2018;13:e0206490.
Fatahi S, Qorbani M, Surkan PJ, Azadbakht L. Associations between dietary acid load and obesity among Iranian women. J Cardiovasc Thorac Res. 2021;13:3.
Sookoian S, Pirola CJ. Systematic review with meta‐analysis: risk factors for non‐alcoholic fatty liver disease suggest a shared altered metabolic and cardiovascular profile between lean and obese patients. Alimentary Pharmacol Therapeutics. 2017;46:85–95.
Karimbeiki R, Pourmasoumi M, Feizi A, Abbasi B, Hadi A, Rafie N, et al. Higher dietary diversity score is associated with obesity: a case–control study. Public Health. 2018;157:127–34.
Kant AK, Schatzkin A, Ziegler RG. Dietary diversity and subsequent cause-specific mortality in the NHANES I epidemiologic follow-up study. J Am Coll Nutr. 1995;14:233–8.
Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60.
Noureddin M, Zelber‐Sagi S, Wilkens LR, Porcel J, Boushey CJ, Le Marchand L, et al. Diet associations with nonalcoholic fatty liver disease in an ethnically diverse population: the Multiethnic Cohort. Hepatology. 2020;71:1940–52.
Lei S, Liu ZW, Yun L, Cai G, Zhang H, Song LJ, et al. The prevalence of nonalcoholic fatty liver disease and its association with lifestyle/dietary habits among university faculty and staff in Chengdu. Biomed Environ Sci. 2012;25:383–91.
Li Y, He Y, Wang D, Gao X. Association between dietary acid‐based load and obesity in Chinese adults. Wiley Online Library. 2012.
Almeida NS, Rocha R, Cotrim HP, Daltro C. Anthropometric indicators of visceral adiposity as predictors of non-alcoholic fatty liver disease: a review. World J Hepatol. 2018;10:695.
Pang Q, Zhang J-Y, Song S-D, Qu K, Xu X-S, Liu S-S, et al. Central obesity and nonalcoholic fatty liver disease risk after adjusting for body mass index. World J Gastroenterology: WJG. 2015;21:1650.
Pilgrim A, Robinson S, Sayer AA, Roberts H. An overview of appetite decline in older people. Nurs Older People. 2015;27:29.
Hays NP, Roberts SB. The anorexia of aging in humans. Physiol Behav. 2006;88:257–66.
Hoshiar-Rad A, Kianfar H, Bani-Eghbal B, Dadkhah M, Ghafar-Pour M, editors. Determining of dietary variety in rural and urban families of Tehran. Proceedings of the Fourth Iranian Congress of Nutrition, Tehran, Iran, Tehran University; 1997.
Mirmiran P, Azadbakht L, Azizi F. Dietary diversity within food groups: an indicator of specific nutrient adequacy in Tehranian women. J Am Coll Nutr. 2006;25:354–61.
Acknowledgements
We greatly appreciate the participants, healthcare executives in public health centers in Amol, and the GILDRC staff (www.gildrc.ac.ir), without whom the study would not have been possible.
Funding
This research was conducted by a grant from the research council of Iran University of Medical Sciences of Iran (IUMS) (grant NO: 99–2–30–19054).
Author information
Authors and Affiliations
Contributions
FZ, MK, AHF, MN, MRM, and AD were responsible for the study concept and design. AD and NM had full access to all data and took responsibility for the integrity of the data and the accuracy of the data analysis. MM, FST, and AA were involved in data collection. AD, NM, CC, and SC analyzed and interpreted the data. MH and AD wrote the initial draft of the manuscript. All authors revised the manuscript critically for important intellectual content and approved the final manuscript. FZ is the guarantor and takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and procedures involving human subjects/patients were approved by the Iran University of Medical Sciences (IUMS) ethical committee (No. IR.IUMS.REC.1399.1393). Written informed consent was obtained from all participants prior to the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Doustmohammadian, A., Amirkalali, B., Gholizadeh, E. et al. Mediators of dietary diversity score (DDS) on NAFLD in Iranian adults: a structural equation modeling study. Eur J Clin Nutr 77, 370–379 (2023). https://doi.org/10.1038/s41430-022-01240-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01240-0