Abstract
Objective
The aim of this study was to determine the influence of polymorphisms in some key gene actors of the vitamin D (vitD) metabolic pathway on supplementation efficacy.
Methods
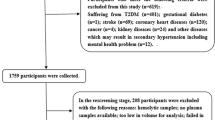
In total, 245 healthy participants were recruited from occupational medicine service in Sahloul University Hospital with vitD deficiency [25(OH)D ≤ 30 ng/ml]. After giving an informed consent, all participants were asked to complete a generalized questionnaire and to follow a detailed personalized supplementation protocol. Genetic study was performed by PCR-RFLP for 15 single nucleotide polymorphisms (SNPs) belonging to DBP, CYP2R1, CYP27B14, CYP24A1 and VDR genes. Statistical study was carried out with SPSS23.0.
Results
Among the studied SNPs, non-response was significantly associated with variant alleles of rs4588 (OR* = 11.51; p < 0.001), rs10766197 (OR* = 6.92; p = 0.008) and rs12794714 (OR* = 5.09; p = 0.004). These three SNPs contributed in 18.8% in response variability with rs4588 being the most influential (10.3%). There was a significant linear negative correlation between baseline 25(OH)D and post supplementation 25(OH)D concentration (r = −0.437; p < 0.001) as well as a linear negative association between the increase in 25(OH)D concentration and GRS (GRS: genetic risk score = the sum of risk alleles) (r = −0.149; p = 0.033).
Conclusions
DBP-rs4588, CYP2R1-rs10766197 and rs12794714 variants are associated with variations in serum 25(OH)D concentrations and efficacy of response to vitD supplementation in Tunisian adults. Taking into account these variations can help to better adapt vitD intake to ensure a higher response to supplementation.
Similar content being viewed by others
Introduction
Vitamin D (vitD) is a fat soluble secosteroid vitamin with multiple functions extending beyond the regulation of intestinal calcium absorption. In recent years, research articles investigating associations between vitD status and health have reached an all-time high, and an increase in supplementation studies has followed [1, 2]. Given the pleiotropic effects of vitD, the scientific focus has gone beyond its known classic benefits on skeletal health to include multiple pathologies such as hyperglycemic disorders, cardiovascular, neurological and liver diseases [3,4,5].
The global prevalence of hypovitaminosis D appears to be increasing, and it is estimated that more than 1.5 billion people worldwide have vitD deficiency including healthy community-living people, and even patients receiving medical treatment for osteoporosis, which makes this disorder one of the most common nutritional deficiencies in the world affecting all segments of the population [6, 7].
The spectrum of vitD status across the population in Tunisia resembles that in Southern European countries rather than in Middle Eastern ones. Although Tunisia is a sunny country, sun exposure was reported to be insufficient and dietary vitD intake did not achieve the dietary reference intakes. In fact, about 47.6% had vitD deficiency with an approximate daily vitD intake under 200UI/daily [8].
In recent years, awareness about vitD deficiency has increased greatly, and vitD supplementation is currently considered as one of the best approaches for achieving adequate serum 25(OH)D concentrations. However, changes in serum 25(OH)D relative to vitD supplementation vary widely among individuals. Determinants of change in serum post supplementation 25(OH)D concentration can be explained by demographic, genetic, and environmental factors [9]. In fact, recent genome-wide association studies have uncovered associations of 25(OH)D concentration with proteins involved in the metabolism action and transport of vitD. SNPs in these genes have been linked to vitD deficiency in the general population and to the high variability in response to supplementation [10, 11].
Studies that investigate the effect of genetic variants in vitD metabolic related gene polymorphisms on serum 25(OH)D concentrations are lacking in the Tunisian population. Therefore, we aimed to investigate the influence of non-genetic and genetic determinants of change in serum 25(OH)D levels and their effect on response efficacy to vitD supplementation, in healthy individuals.
Methods
All methods used in this study are described in the Supplementary Materials and Methods file.
Results
Post supplementation serum 25(OH)D concentration
Based on serum 25(OH)D concentrations dosed at baseline and considering 30 ng/ml as “cut off”, we subdivided our population into two subgroups: vitD deficient (25(OH)D < 30 ng/ml; 205 (83.7%)) and vitD non-deficient (25(OH)D ≥ 30 ng/ml; 40 (16.3%)).
In deficient subjects (n = 205), mean serum 25 (OH)D concentrations increased from baseline concentration of 13.8 ± 5.56 ng/ml to 35.74 ± 9.55 ng/ml after supplementation; ∆ = +21.94 ± 10.57 ng/ml. In this deficient group, 23 deficient subjects (11.2%) did not respond to supplementation, while 182 subjects (88.8%) increased their vitD status above 30 ng/ml. Sixty-two (30.2%) had low response, 59 (28.8%) had an average response and 61 (29.8%) had the highest response to supplementation.
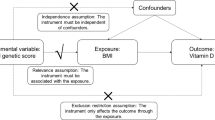
Effect of non-genetic factors in response to vitD supplementation
The study of various non-genetic factors as potential causes of variability in the responses to supplementation showed that among the studied characteristics, season, baseline vitD, number of vitD ampoules, physical activity and albumin were considered as potential confounding factors (p < 0.25) to which we adjusted all genotypic analysis so that we only obtain the specific effect of the studied SNPs (Supplementary Table 1). However, the diagnosis of the potential presence of multicollinearity in regression analysis, showed a moderate correlation between two confounders (baseline vitD and number of vitD ampoules) with a variance inflation factor: VIF = 5.39. Therefore, only season, baseline vitD, physical activity and albumin were considered as potential confounding factors. The new VIF for these variables were lower than two which proves the absence of multicollinearity.
As for the goodness of fit of the regression model, it was assessed by the Hosmer–Lemeshow test. The chi2 goodness-of-fit test provided no reason to reject the model as poorly fit (goodness of fit chi2 = 5.92, p = 0.656).
Effect of genotype in response to vitD supplementation
There was a significant difference in vitD increase according to genotype for three SNPs: DBP-rs4588 (p = 0.011), CYP2R1-rs10766197 (p = 0.006) and rs12794714 (p = 0.024) (Supplementary Table 2). Similarly, there were significant differences according to response level in genotype frequencies of these three SNPs (Table 1).
By binary logistic regression and after adjustment to potential confounding factors, we noted that the risk (OR) of non-response associated to the three SNPs (rs4588, rs10766197 and rs12794714) increased between 3.45 and 11.51 depending on the SNPs (rs4588, rs10766197 or rs12794714) and zygocy (homozygous major/minor or heterozygous) (Table 1).
In order to study the possible synergy between the three significant polymorphisms and their combined effects, we established a composite weighted genetic risk score (wGRS) defined by the following mathematical equation from the binary logistic regression model:
Where wGRS predictive score values ranged from 1.31 to 75.34 with a cutoff value of 12.03. By comparing responder and non-responder to vitD supplementation groups, we noted a significant difference in the scores (8.68 ± 10.88 versus 32.8 ± 25.7; p < 0.001). The sensitivity, specificity, accuracy and area under the ROC curve values for this model were 75%, 73.5%, 75.8% and 0.807 (p < 0.001), respectively using the SPSS software.
There were no associations between wGRS and baseline 25(OH)D concentration (r = −0.175; p = 0.06). However, a linear negative association was observed between post supplementation 25(OH)D concentration and wGRS (r = −0.232; p = 0.001) and between vitD increase Δ and wGRS (r = −0.152; p = 0.029).
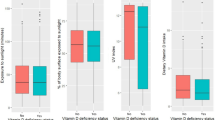
In order to simplify this score, we opted for the use of simple count method by establishing a simplified GRS as the sum of risk alleles (0–6). At baseline, there were no associations between GRS and baseline 25(OH)D concentrations (p = 0.074). Nevertheless, there was a linear negative association between post supplementation 25(OH)D concentration and GRS (r = −0.149; p = 0.033). We have also noted that subjects with GRS = 6 had the lowest increase (∆ = 12.46 ± 6.1 ng/ml) compared to those with GRS = 0 (∆ = 24.61 ± 11.8 ng/ml); p = 0.041 (Fig. 1A). Overall, there was a mean difference in 25(OH)D concentrations of 12.15 ng/ml between carriers of no risk alleles and carriers of all 6 risk alleles. Consequently, the risk of non-response to supplementation increases from 1.2 (1 risk allele) to 20.3 (6 risk alleles) (Fig. 1B).
A At baseline, no significant association was observed between GRS and 25(OH)D concentrations. However, there was a significant linear negative association between GRS and post supplementation 25(OH)D concentration (r = −0.149; p = 0.033). Participants carrying all six risk alleles experienced a reduced response in 25(OH)D (post supplementation 25(OH)D = 24.02 ± 4 ng/ml) compared to those carrying 0 risk allele (post supplementation 25(OH)D = 37.7 ± 8.8 ng/ml). Δ = 25(OH)D increase; GRS genetic risk score. B Adjusted OR of non-responseto vitD supplementation associated to genetic risk score. Adjusted OR including 95% confidence interval due to GRS variation (Adjusted for: season, baseline 25(OH)D, physical activity and albumin). The horizontal dashed line represents the OR reference value 1.
Furthermore, there was a significant linear negative correlation between baseline 25(OH)D and ∆ (r = −0.437; p < 0.001) meaning that lower baseline vitD status was associated with higher response to supplementation (Fig. 2). This negative correlation remains valid only for low GRS (0, 1 and 2). However in the presence of several variations meaning for higher GRS (more than 3), this correlation becomes non-significant. Similarly, when we adjust for the polymorphisms affecting post supplementation 25(OH)D status, this correlation becomes non-significant, thus the presence of polymorphisms alters this correlation.
Genetic and non-genetic factors contribution on response variation
Multiple linear regression revealed that genetic factors predicted 15.6%, while non-genetic factors predicted 3.5% of variability in response to vitD supplementation. Cumulative R2 was up to 18.8%. rs4588 by itself was responsible for 10.3% of the response variability (Table 2).
Discussion
In our population, 83.7% were deficient and required vitD supplementation. The mean 25(OH)D concentration in supplemented subjects increased from 13.8 ng/ml ±5.56 to 35.74 ng/ml ±9.55 (∆ = +21.94 ng/ml ±10.57). Our supplementation protocol corrected hypovitaminosis in 82.8% of the deficient subjects, yet there were still 11.2% whose 25(OH)D concentrations did not reach 30 ng/ml. This highlights a major variability of response to vitD supplementation between subjects. Our results were similar to those reported by Rouillon et al. and Yao et al. in various populations [12, 13]. Indeed, there was always a number of subjects who did not reach the desired concentration, which may be related to genetic or non-genetic factors [12]. Genetic differences in production, transportation and degradation of 25(OH)D resulting in differences in 25(OH)D at baseline seem to affect the handling of additional vitD supplements. Thus, different SNPs significantly influenced the response to vitD supplementation [1, 7, 14]. Three SNPs (rs4588, rs10766197 and rs12794714; p < 0.05), have shown to be significantly involved in response variation to vitD supplementation.
The rs4588 minor allele was associated with lower response to vitD supplementation, as 34.8% minor allele (TT) carriers remained vitD deficient versus the 70.4% major allele (GG) carriers who reached the desired post supplementation vitD value. In like manner, 73.8% GG carriers in the responders group had the highest response compared to only 4.8% TT carriers who had the lowest response. After adjustment for confounding factors, we noted that compared to homozygous major genotype, minor allele carriers were 11.51 and 7.58 times more likely to be non-responders respectively for homozygous and heterozygous. This low response associated with T allele was also reported by Al-Daghri et al. who demonstrated that the overall increase in 25(OH)D concentrations was 70.5% in homozygous major genotype group versus 56.9% in the heterozygous genotype group and that carriers of minor risk allele were 3.7 times more likely to be non-responders to vitD supplementation [15]. Nissen et al. demonstrated that carriers of rs4588 risk alleles had the smallest increase in serum 25(OH)D among Danes receiving vitD fortified bread and milk or ultraviolet B treatment [16]. Similar results were observed in a Chinese population supplemented with 2000 IU/day [12], as well as in a Thais study given 400 IU/day vitD and calcium [17].
DBP gene encodes the 52 to 59 kDA DBP protein, which regulates bioavailability and plays a key role in transporting vitD and its metabolites. Given its biological role, it is therefore not surprising that several previous studies [15, 18] have shown that DBP polymorphism contributes to variability in total circulating 25(OH)D concentrations and has more recently been strongly linked to the response to supplementation [16, 17, 19]. The specific effect of rs4588-G might largely be attributed to its raising DBP level, as well as a higher binding affinity for 25(OH)D. Additionally, vitD bound to DBP might have relatively long half-life by avoiding being catabolized to inactive metabolites and therefore, increasing 25(OH)D concentrations [12, 17, 20].
Although the association between CYP2R1 genotypes and serum 25 (OH)D concentration was already identified in several studies [10, 21], few have examined the effects of these genotypes in terms of efficacy of response to vitD supplementation.
In rs10766197, only 4.4% carriers of major alleles were non-responders versus 43.6% carriers of minor alleles. After adjustment for confounding factors, the risk of non-response was 6.92 times higher for homozygous minor allele and 5.31 times higher for heterozygous. Thus, we speculate that individuals with these polymorphisms may be at higher risk for vitD deficiency. The differences we have found between major and minor homozygous alleles for this SNP are similar to those reported by several studies [22, 23]. Bahrami et al. reported an OR of 25(OH)D increase associated to G allele two-fold higher compared to A allele (OR = 2.1; p = 0.03) [22] after supplementing healthy school girls with 50,000 IU of vitD for 9 weeks.
For the rs12794714, we noted that 39.1% AA carriers did not respond to supplementation versus only 4.4% GG carriers. The risk of non-responsiveness was 5.09 fold higher in genotypic variant AA and 3.45 folds higher in heterozygous.
Tomei et al. [24] and Slow et al. in the VIDARIS randomized controlled trial [20] did not report any significant association between these two SNPs and serum 25(OH)D concentrations neither at baseline nor in post supplementation. However, Barry et al. showed similar results with an estimated percentage difference of 3.8% for rs1279414 and 4.7% for rs10766197 per variant allele, after adjustment for sex, season and age [23].
These two SNPs seem to impair the biological role of CYP2R1 which is a member of the CYP2 family encoding cytochrome P450 proteins generating 25-hydroxy vitamin D in the liver. Therefore, reduced 25 hydroxylase activity may influence 25(OH)D concentrations even after supplementation [25].
Notably, individual SNPs confer little risk increments and explain a small portion of disease heritability, while the GRS can aggregate the contribution of multiple SNPs to evaluate the additive genetic effects on the risk of non-response to supplementation [26]. Our results indicate that the GRS from DBP and CYP2R1 variants can predict variability in response to vitD supplementation. In fact, the risk of non-response to vitD supplementation, increases from 1.2 (1 risk allele) to 20.3 (6 risk alleles). As the GRS increased, the individual’s risk of maintaining a 25(OH)D concentration below the required value increased. Genetically predisposed individuals carrying all 6 risk alleles had the lowest baseline 25(OH)D concentration and the smallest increase. This indicates that in order to achieve a targeted 25(OH)D concentration, those at the highest risk of deficiency have the greatest vitD requirement.
The suggestion from the present study is that beneficial effects of vitD supplementation occur when baseline 25(OH)D concentrations are <30 ng/ml, and that deficient subjects would ultimately achieve better health outcomes. Williams et al. reported a greater change in deficient subjects supplemented with sublingual and capsular vitD [27]. Yet, Sluyter et al. demonstrated that vitD supplementation significantly decreased central blood pressure in subjects with poor vitD status at baseline [28]. A similar threshold is suggested for vitD effects on other putative vitD targets, such as reduction of exacerbations of chronic obstructive pulmonary disease [29].
When both genetic and non-genetic determinants were considered, genetic factors exerted stronger impact in response to vitD supplementation. Indeed, genetic factors explained up to 18.8% of variability in response to vitD supplementation, while non-genetic factors (albumin and physical activity) had only 3.5% of the response-modifying effect. Similar results were reported by the randomized trial of Yao et al. suggesting that the joint effect of DBP-rs7041, VDR-rs2228570, and CYP2R1-rs10741657 measured by GRS, could explain a larger portion than the combined non-genetic factors (baseline value, BMI, and gender) in response to vitD supplementation [12]. Arabi et al. confirmed that genetic polymorphisms in CYP2R1 explained between 4.8 and 9.8% of variability in 25(OH)D levels but failed to detect any effect on changes of post supplementation vitD [30].
For non-genetic factors, the implication of albumin concentration might be explained by the fact that about 90% of total vitD is bound with DBP, 10–15% is loosely bound with albumin, and about 0.1% is present as free-circulating fraction. Therefore, the availability of 25(OH)D depends not only on the total 25(OH)D concentration but also on the concentration of DBP and albumin [31]. As for the physical activity influence, it might be explained by adiposity and that VitD could be sequestered by adipose tissue after supplementation [32]. A systematic review by Zittermann et al. indicated that variations in serum 25(OH)D levels after supplementation could be explained by body weight (34.5%), type of supplement (9.8%), age (3.7%), calcium supplements (2.4%) and baseline 25OHD levels (1.9%) [33]. Ekwaru et al. recommended vitD supplementation to be 2–3 times higher for obese subjects and 1.5 times higher for overweight subjects to achieve the same 25(OH)D values [34].
Recent studies have reported that the use of intermittent high-dose bolus, introduced to achieve high adherence, rather than regular daily maintenance was ineffective at preventing rickets, tuberculosis, acute respiratory infections [35] and may increase the risk of falling in elderly subjects [36]. There is a plausible biological explanation for this, since high-dose bolus supplementation induces the suppression of vitD activation by the expression of long-term catabolic enzyme 24-hydroxylase and fibroblast growth factor 23, both of which have vitD inactivating effects. It has been recognized that the increased 24-hydroxylase activity, as a feedback control response to a large bolus of vitD, may itself have a long half-life [37]. This means that a single high-dose bolus of vitD could paradoxically lead to intracellular deficiency of activated vitD as a rebound phenomenon. This might be particularly important in immune cells such as the dendritic cells that are probably central to the hyperinflammatory state seen in severe COVID-19 [35]. Overall, taking into account the rs4588 minor allele frequency (0.21%) (Supplementary Table 3) and the implication of this polymorphism on the poor response to vitD supplementation by modifying its binding affinity, it seems that modest doses and daily provision of vitD supplementation is more effective rather than intermittent high-dose boluses.
Furthermore, one of the major obstacles contributing to vitD deficiency is the lack of foods naturally rich in vitD. Therefore, food fortification programs seem to be a very promising strategy to curb vitD deficiency. Evidence from a long-term population-based Finnish study documented improvement of 25(OH)D concentration after 11 years of fortification [38]. VitD requirements might even be higher amongst high risk groups with genetically determined reduction in responsiveness to vitD. Therefore, applying food fortification programs on individuals with specific genetic background would be very promising for provision of personalized health care.
Our study has several strengths including its being the largest analysis of vitD status among healthy adults in Tunisia, the personalized supplementation protocol which was adapted to baseline vitD value and the availability of detailed personal data. Nevertheless, it has some limitations too; firstly, the decision for a mega dose of vitD intake is a very controversial choice; surely, it remarkably simplifies our study design but it induces self-regulatory mechanisms that may last for months. Secondly, the decision to focus on deficient subjects with serum 25(OH)D < 30 ng/ml) rather than deficient (<20 ng/ml) could be argued. Although concentrations >20 ng/ml may be adequate for bone health and used in most supplementation protocols, concentrations above 30 ng/ml are needed for many other health outcomes [39].
The current study provides novel insight that helps further define the complex relationship between genetic and environmental factors that affect vitD levels. It is also important for public health recommendations and vitD food fortification programs because it showed that the genetic predisposition in the DBP and CYP2RI genes may have large impact on 25(OH)D concentrations and that even after a personalized high doses supplementation protocol, vitD deficiency persisted in some groups. Further information on the effects of such factors on the self-regulatory mechanisms induced by interval bolus dosing would be valuable in planning programs for correcting vitD deficiency.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Zhang Y, Fang F, Tang J, Jia L, Feng Y, Xu P, et al. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ. 2019;366:l4673.
Stokes CS, Lammert F. Vitamin D supplementation: less controversy, more guidance needed. F1000Research. 2016;4–5.
Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur. J. Clin. Nutr. 2020;74:1498–513.
Bouillon R, Lips P, Bilezikian JP. Vitamin D supplementation and musculoskeletal health. Lancet Diabetes Endocrinol. 2019;7:85–6.
Dawson-Hughes B, Staten MA, Knowler WC, Nelson J, Vickery EM, LeBlanc ES, et al. Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the vitamin D and type 2 diabetes (D2d) study. Diabetes Care. 2020;43:2916–22.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81.
Wimalawansa S. Causes, benefits and consequences of vitamin D deficiency. 2019.
Meddeb N, Sahli H, Chahed M, Abdelmoula J, Feki M, Salah H, et al. Vitamin D deficiency in Tunisia. Osteoporos Int. 2005;16:180–3.
Mazahery H, Von, Hurst PR. Factors affecting 25-hydroxyvitamin D concentration in response to vitamin D supplementation. Nutrients. 2015;7:5111–42.
Jiang X, Kiel DP, Kraft P. The genetics of vitamin D. Bone. 2019;126:59–77.
Waterhouse M, Tran B, Armstrong BK, Baxter C, Ebeling PR, English DR, et al. Environmental, personal, and genetic determinants of response to vitamin D supplementation in older adults. J Clin Endocrinol Metab. 2014;99:E1332–40.
Yao P, Sun L, Lu L, Ding H, Chen X, Tang L, et al. Effects of genetic and nongenetic factors on total and bioavailable 25 (OH) D responses to vitamin D supplementation. J Clin Endocrinol Metab. 2017;102:100–10.
Rouillon V, Dubourg G, Gauvain J-B, Baron D, Glemarec J, Cormier G, et al. Insuffisance en vitamine D: évaluation d’une supplémentation orale standardisée utilisant des ampoules de 100 000 IU de cholécalciferol, en fonction du taux sérique initial de 25OH vitamine D. Rev du Rhum. 2012;79:351–4.
Pott-Junior H, Luzeiro C, Senise JF, Castelo A. Association of seasonality and serum albumin concentration with vitamin D deficiency in subjects with chronic hepatitis C infection living in a sunny country. Public Health Nutr. 2020;23:1247–53.
Al-Daghri NM, Mohammed AK, Bukhari I, Rikli M, Abdi S, Ansari MGA, et al. Efficacy of vitamin D supplementation according to vitamin D-binding protein polymorphisms. Nutrition. 2019;63:148–54.
Nissen J, Vogel U, Ravn-Haren G, Andersen EW, Madsen KH, Nexø BA, et al. Common variants in CYP2R1 and GC genes are both determinants of serum 25-hydroxyvitamin D concentrations after UVB irradiation and after consumption of vitamin D3–fortified bread and milk during winter in Denmark. Am J Clin Nutr. 2015;101:218–27.
Nimitphong H, Saetung S, Chanprasertyotin S, Chailurkit L-O, Ongphiphadhanakul B. Changes in circulating 25-hydroxyvitamin D according to vitamin D binding protein genotypes after vitamin D 3 or D 2 supplementation. Nutr J. 2013;12:39.
Pooyan S, Rahimi MH, Mollahosseini M, Khorrami-Nezhad L, Maghbooli Z, Mirzaei K. The Association between Vitamin D Deficiency and variants of Vitamin D Binding protein gene among Healthy Iranian Adults. Int. J. Vitam. Nutr. Res. 2019;90:249–56.
Mehramiz M, Khayyatzadeh SS, Esmaily H, Ghasemi F, Sadeghi-Ardekani K, Tayefi M, et al. Associations of vitamin D binding protein variants with the vitamin D-induced increase in serum 25-hydroxyvitamin D. Clin Nutr ESPEN. 2019;29:59–64.
Slow S, Pearson JP, Florkowski CM, Elder PA, Lewis JG, Kennedy MA, et al. Effect of genetic factors on the response to vitamin D3 supplementation in the VIDARIS randomized controlled trial. Nutrition. 2020;75:110761.
Xu X, Mao J, Zhang M, Liu H, Li H, Lei H, et al. Vitamin D deficiency in Uygurs and Kazaks is associated with polymorphisms in CYP2R1 and DHCR7/NADSYN1 genes. Med Sci Monit Int Med J Exp Clin Res. 2015;21:1960.
Bahrami A, Mehramiz M, Ghayour-Mobarhan M, Bahrami-Taghanaki H, Ardekani KS, Tayefi M, et al. A genetic variant in the cytochrome P450 family 2 subfamily R member 1 determines response to vitamin D supplementation. Clin Nutr. 2019;38:676–81.
Barry EL, Rees JR, Peacock JL, Mott LA, Amos CI, Bostick RM, et al. Genetic variants in CYP2R1, CYP24A1, and VDR modify the efficacy of vitamin D3 supplementation for increasing serum 25-hydroxyvitamin D levels in a randomized controlled trial. J Clin Endocrinol Metab. 2014;99:E2133–7.
Tomei S, Singh P, Mathew R, Mattei V, Garand M, Alwakeel M, et al. The role of polymorphisms in vitamin D-related genes in response to vitamin D supplementation. Nutrients. 2020;12:2608.
Shinkyo R, Sakaki T, Kamakura M, Ohta M, Inouye K. Metabolism of vitamin D by human microsomal CYP2R1. Biochem Biophys Res Commun. 2004;324:451–7.
Yu F, Wang C, Wang L, Jiang H, Ba Y, Cui L, et al. Study and evaluation the impact of vitamin D receptor variants on the risk of type 2 diabetes mellitus in Han Chinese: 中国汉族人群中维生素 D 受体基因多态性与 2 型糖尿病的关系分析和评价. J Diabetes. 2017;9:275–84.
Williams CE, Williams EA, Corfe BM. Rate of change of circulating 25-hydroxyvitamin D following sublingual and capsular vitamin D preparations. Eur J Clin Nutr. 2019;73:1630–5.
Sluyter JD, Camargo CA Jr, Stewart AW, Waayer D, Lawes CM, Toop L, et al. Effect of monthly, high‐dose, long‐term vitamin D supplementation on central blood pressure parameters: a randomized controlled trial substudy. J Am Heart Assoc. 2017;6:e006802.
Sluyter JD, Camargo CA, Waayer D, Lawes CM, Toop L, Khaw K-T, et al. Effect of monthly, high-dose, long-term vitamin D on lung function: a randomized controlled trial. Nutrients. 2017;9:1353.
Arabi A, Khoueiry-Zgheib N, Awada Z, Mahfouz R, Al-Shaar L, Hoteit M, et al. CYP2R1 polymorphisms are important modulators of circulating 25-hydroxyvitamin D levels in elderly females with vitamin insufficiency, but not of the response to vitamin D supplementation. Osteoporos Int. 2017;28:279–90.
Chun RF. New perspectives on the vitamin D binding protein. Cell Biochem Funct. 2012;30:445–56.
de Oliveira LF, de Azevedo LG, da Mota Santana J, de Sales LPC, Pereira-Santos M. Obesity and overweight decreases the effect of vitamin D supplementation in adults: systematic review and meta-analysis of randomized controlled trials. Rev. Endocr. Metab. Disord.2020;21:67–76.
Zittermann A, Ernst JB, Gummert JF, Börgermann J. Vitamin D supplementation, body weight and human serum 25-hydroxyvitamin D response: a systematic review. Eur J Nutr. 2014;53:367–74.
Ekwaru JP, Zwicker JD, Holick MF, Giovannucci E, Veugelers PJ. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS ONE. 2014;9:e111265.
Griffin G, Hewison M, Hopkin J, Kenny RA, Quinton R, Rhodes J, et al. Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19. Clin Med. 2021;21:e144.
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev. 2019;40:1109–51.
Ketha H, Thacher TD, Oberhelman SS, Fischer PR, Singh RJ, Kumar R. Comparison of the effect of daily versus bolus dose maternal vitamin D3 supplementation on the 24, 25-dihydroxyvitamin D3 to 25-hydroxyvitamin D3 ratio. Bone. 2018;110:321–5.
Jääskeläinen T, Itkonen ST, Lundqvist A, Erkkola M, Koskela T, Lakkala K, et al. The positive impact of general vitamin D food fortification policy on vitamin D status in a representative adult Finnish population: evidence from an 11-y follow-up based on standardized 25-hydroxyvitamin D data. Am J Clin Nutr. 2017;105:1512–20.
Pludowski P, Holick MF, Grant WB, Konstantynowicz J, Mascarenhas MR, Haq A, et al. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125–35.
Acknowledgements
We thank the Tunisian Ministry of Higher Education, Scientific Research and Technology and the Ministry of Health for their support. The authors are thankful to all the members of the biochemistry laboratory of Sahloul University Hospital for their cooperation in conducting this research specially Mrs. Henda Falfoul and Mr. Mahmoud Smida. Finally, we gratefully acknowledge the contribution of participating individuals whose cooperation made this study possible.
Funding
This study was funded by grants from the Tunisian Ministry of Higher Education, Scientific Research and Technology and the Ministry of Health.
Author information
Authors and Affiliations
Contributions
This study was supervised by AO and AB. MA, YK and HH designed the study and were responsible for screening potentially eligible studies. MA, SH and MST recruited the patients under the supervision of SK. MA performed the genotyping. AO and MA performed the statistical analysis and the interpretation of the data. MA wrote the manuscript. AO and DA provided a critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ammar, M., Heni, S., Tira, M.S. et al. Variability in response to vitamin D supplementation according to vitamin D metabolism related gene polymorphisms in healthy adults. Eur J Clin Nutr 77, 189–194 (2023). https://doi.org/10.1038/s41430-022-01218-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01218-y
This article is cited by
-
Pharmacological evaluation of vitamin D in COVID-19 and long COVID-19: recent studies confirm clinical validation and highlight metformin to improve VDR sensitivity and efficacy
Inflammopharmacology (2024)
-
Increasing baseline aortic valve peak flow velocity is associated with progression of aortic valve stenosis in osteoporosis patients—a possible link to low vitamin D status
Archives of Osteoporosis (2023)