Abstract
Background/Aims
The liver plays a central role in the fatty acid metabolism. Therefore, cirrhosis is prone to energy malnutrition and is associated with a poor prognosis. On the other hand, proton density fat fraction (PDFF) measured by magnetic resonance imaging (MRI) is a noninvasive and highly accurate method to quantify liver fat. In this study, we aimed to investigate the relationship between hepatic fat loss (HFL) and malnutrition by PDFF measurement in chronic liver disease (CLD).
Methods
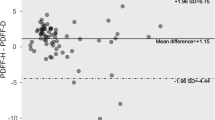
In this retrospective single-center study of 485 patients with CLD, hepatic fat content was measured by MRI-PDFF, and CT-measured body composition and CONUT (Controlling Nutritional Status) score were used as nutritional assessment methods, respectively.
Results
In the overall cohort, MRI-PDFF was positively correlated with body fat mass, muscle mass and respectively. The HFL defined by PDFF ≤ 2.7% is 25%, and in multivariate analysis, decreased body fat mass and Triglyceride, and increased CONUT score were independent associated factors of HFL (p < 0.05, for all). Additionally, 35% of patients with cirrhosis (n = 107) had HFL, and the Cox proportional hazards model showed that Child–Pugh score and HFL were independent prognostic factors (p < 0.01, for both).
Conclusions
MRI-PDFF was shown to be a useful indicator of malnutrition in cirrhosis reflecting body composition. Preservation of liver fat content in nutritional therapy may improve the prognosis of cirrhotic patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gluchowski NL, Becuwe M, Walther TC, Farese RV Jr. Lipid droplets and liver disease: from basic biology to clinical implications. Nat Rev Gastroenterol Hepatol. 2017;14:343–55.
Wang L, Liu J, Miao Z, Pan Q, Cao W. Lipid droplets and their interactions with other organelles in liver diseases. Int J Biochem Cell Biol. 2021;133:105937.
Tada T, Kumada T, Toyoda H, Sone Y, Takeshima K, Ogawa S, et al. Viral eradication reduces both liver stiffness and steatosis in patients with chronic hepatitis C virus infection who received direct-acting anti-viral therapy. Aliment Pharmacol Ther. 2018;47:1012–22.
Imajo K, Kessoku T, Honda Y, Tomeno W, Ogawa Y, Mawatari H, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016;150:626–37.
Caussy C, Reeder SB, Sirlin CB, Loomba R. Noninvasive, quantitative assessment of liver fat by MRI-PDFF as an endpoint in NASH trials. Hepatology. 2018;68:763–72.
Tajika M, Kato M, Mohri H, et al. Prognostic value of energy metabolism in patients with viral liver cirrhosis. Nutrition. 2002;18:229–34.
Enooku K, Tsutsumi T, Kondo M, Fujiwara N, Sasako T, Shibahara J, et al. Hepatic FATP5 expression is associated with histological progression and loss of hepatic fat in NAFLD patients. J Gastroenterol. 2020;55:227–43.
Nishikawa H, Shiraki M, Hiramatsu A, Moriya K, Hino K, Nishiguchi S. JSH guideline for sarcopenia in liver disease (1st edition): recommendation from the working group for creation of sarcopenia assessment criteria in the JSH. Hepatol Res. 2016;46:951–63.
Tantai X, Liu Y, Yeo YH, Praktiknjo M, Mauro E, Hamaguchi Y, et al. Effect of sarcopenia on survival in patients with cirrhosis: a systematic review and meta-analysis. J Hepatol. 2022;76:588–99.
Hsu C, Caussy C, Imajo K, Chen J, Singh S, Kaulback K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2019;17:630–7.
Takada A, Matsuda Y, Takase S, Okudaira M, Ohta Y, Tsujii T, et al. A national surveillance study on alcoholic liver disease in Japan (1986–1991). Nihon Shokakibyo Gakkai Zasshi. 1994;91:887–98.
Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018–26.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves H, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–8.
Reeder SB, McKenzie CA, Pineda AR, Yu H, Shimakawa A, Brau AC, et al. Water-fat separation with IDEAL gradient-echo imaging. J Magn Reson Imaging. 2007;25:644–52.
Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm RC, Rossman PJ, et al. Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol. 2007;5:1207–13.
Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288:462–8.
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Choi MH, Choi JI, Park MY, Rha SE, Oh SN, Jung SE, et al. Validation of intimate correlation between visceral fat and hepatic steatosis: quantitative measurement techniques using CT for area of fat and MR for hepatic steatosis. Clin Nutr. 2018;37:214–22.
Choi SJ, Kim SM, Kim YS, Kwon OS, Shin SK, Kim KK, et al. Magnetic resonance-based assessments better capture pathophysiologic profiles and progression in nonalcoholic fatty liver disease. Diabetes Metab J. 2020:dmj.2020.0137.
Lv Y, Yee Lau W, Wu H, Han X, Gong X, Liu N, et al. Causes of peripheral cytopenia in hepatitic cirrhosis and portal hypertensive splenomegaly. Exp Bio Med. 2017;242:744–9.
Rodrigues SG, Brabandt B, Stirnimann G, Maurer MH, Berzigotti A. Adipopenia correlates with higher portal pressure in patients with cirrhosis. Liver Int. 2019;39:1672–81.
Pang N, Zhao C, Li J, Li L, Yang X, Yang M, et al. Body mass index changes after transjugular intrahepatic portosystemic shunt in individuals with cirrhosis. Nutrition. 2021;84:111095.
Taniguchi E, Kawaguchi T, Otsuka M, Uchida Y, Nagamatsu A, Itou M, et al. Nutritional assessments for ordinary medical care in patients with chronic liver disease. Hepatol Res. 2013;43:192–9.
Glass C, Hipskind P, Tsien C, Malin SK, Kasumov T, Shah SN, et al. Sarcopenia and a physiologically low respiratory quotient in patients with cirrhosis: a prospective controlled study. J Appl Physiol. 2013;114:559–65.
Hanai T, Shiraki M, Nishimura K, Imai K, Suetsugu A, Takai K, et al. Free fatty acid as a marker of energy malnutrition in liver cirrhosis. Hepatol Res. 2014;44:218–28.
Bischoff SC, Bernal W, Dasarathy S, Merli M, Plank LD, Schütz T, et al. ESPEN practical guideline: clinical nutrition in liver disease. Clin Nutr. 2020;39:3533–62.
Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61:1385–96.
Arvaniti V, D’Amico G, Fede G, Manousou P, Tsochatzis E, Pleguezuelo M, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 2010;139:1246–56.
Kawamura S, Matsushita Y, Kurosaki S, Tange M, Fujiwara N, Hayata Y, et al. Inhibiting SCAP/SREBP exacerbates liver injury and carcinogenesis in murine nonalcoholic steatohepatitis. J Clin Investig. 2022;132:e151895.
Author information
Authors and Affiliations
Contributions
Guarantor of the article: AN. Specific author contributions: HA: study concept and design; TY, HA: patient recruitment and characterization; TY: data acquisition, data analysis, and article drafting. All authors provided input and critical revision and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakamura, A., Yoshimura, T. & Asakura, H. Clinical significance of hepatic fat loss in chronic liver disease: a study using MRI proton density fat fractionation. Eur J Clin Nutr 77, 264–269 (2023). https://doi.org/10.1038/s41430-022-01215-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01215-1