Abstract
Background/objectives
Malnutrition is common among older adults. Dietary intervention studies in older adults aiming to improve anthropometrics measures and physical function have been inconsistent. We aimed to investigate the effects of nutrition therapy in combination with home delivered meals and oral nutritional supplements (ONS) in community-dwelling older adults discharged from hospital.
Methods
A total of 106 participants (>65 years) were randomized into the intervention group (n = 53) and into the control group (n = 53). The intervention group received individual nutrition therapy (five in person visits and three phone calls) and freely delivered energy- and protein- rich foods, while the control group received standard care. Dietary intake, anthropometrics, and short physical performance battery (SPPB) were assessed at baseline and at endpoint.
Results
Energy intake at baseline was similar in both groups (~1500 kcal at the hospital) but there was a significant increase in energy intake and body weight in the intervention group (+919 kcal/day and 1.7 kg, P < 0.001 in both cases) during the study period, compared to a significant decrease in both measures among controls (−815 kcal/day and −3.5 kg, P < 0.001 in both cases). SPPB score increased significantly in the intervention group while no changes were observed among controls.
Conclusions
Most Icelandic older adults experience substantial weight loss after hospital discharge when receiving current standard care. However, a 6-month multi-component nutrition therapy, provided by a clinical nutritionist in combination with freely delivered supplemental energy- and protein-dense foods has beneficial effects on body weight, physical function, and nutritional status.
Study registration
This study was registered at ClinicalTrials.gov (NCT03995303).
Similar content being viewed by others
Introduction
Malnutrition, which is commonly observed among older adults [1, 2], is strongly associated with altered body composition, diminished physical and mental function as well as other adverse clinical outcomes. There is, however, some evidence from observational studies that aging per se is not inevitably associated with malnutrition and that appropriate dietary intake and adequate nutritional status is strongly associated with a reduced risk of mobility limitations and improved quality of life [3,4,5]. Hospitalizations are usually short as the health care system is overburdened, and if malnutrition is diagnosed in a patient, there might not be enough time to reverse poor nutritional status during the hospital stay. This should shift the emphasis of treatment to the patient’s home after hospital discharge [6].
In older adults discharged from hospital, there are several options which can potentially help to improve dietary intake, e.g., Meals on Wheels (MOW), oral nutritional supplements (ONS) or nutrition therapy provided by a clinical nutritionist/dietitian. According to a recent systematic review [7], MOW interventions in older adults showed significant improved effects on total energy intake and the number of consumed meals/day to be important. Only three studies out of twelve in this review reported outcomes on functional measures, which are more relevant than simple measures of absolute energy intake. In Iceland, standard care among older adults after discharge from hospital is to be able to order MOW, supplying one hot meal a day, but a recent study suggests that such service may be inadequate for frail and sick older adults at nutritional risk [8].
The use of ONS is another way to improve nutritional status but meta-analyses of such interventions have only shown modest benefits with respect to weight gain (~1.0 kg) and improvements in nutritional status [9]. However, there is some suggestion that inclusion of dietary counselling in such interventions might increase efficacy of these two outcomes [8, 10,11,12,13,14,15].
Very few studies have investigated the combined effects of nutrition therapy and the use of ONS in older adults. Thus, we conducted a 6-month randomized controlled dietary intervention study with the aim of investigating the effects of nutrition therapy provided by a clinical nutritionist following the principles of the Nutrition Care Process (NCP) [16]. This involved access to freely delivered supplemental energy- and protein-dense foods and ONS in community-dwelling older adults discharged from hospital.
Subjects and methods
Study design
The HOMEFOOD study was a 6-month, randomized controlled, assessor blinded intervention trial conducted in older adults (age 66–95 years) recruited in the Reykjavik capital area, Iceland between January 2019, and July 2020. The primary aim was to investigate the effects of intense nutritional therapy, including free access to energy- and protein-dense foods delivered to subjects recently discharged from hospital. The primary outcomes of this trial were changes in body weight and physical function (Short Physical Performance Battery (SPPB)). Body weight loss and poor physical function are both important predictors of negative health outcomes in older adults [2, 17]. These two variables were chosen to be the primary outcomes, as a nutrition intervention with focus on increasing energy- and protein intake is likely to affect body weight and physical function [4, 18], considering the low energy intake previously reported in elderly discharged patients [19]. Secondary outcomes included other anthropometric measurements, nutritional status, muscular strength, dietary intake, exercise, and reported food-related digestion issues, such as diarrhoea, nausea, constipation, or stomach pain.
Reporting, approval, and funding
This study was conducted and reported according to the Consolidated Standards of Reporting Trials guidelines for Randomized Trials of Nonpharmacologic Treatments (CONSORT) [20]. The study was approved by the Ethics Committee for Health Research of the National University Hospital of Iceland and data protection registry (24/2018) in August 2018 and performed in accordance with the Declaration of Helsinki [21]. The study was registered at ClinicalTrials.gov (NCT03995303).
Screening and recruitment
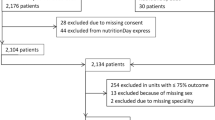
Potential participants (N = 1003) were screened by a clinical nutritionist in collaboration with attending nurses at the Landspitalinn University Hospital of Iceland. Eligible patients were discharging home to independent living from the hospital, aged 65 years or older, and assessed as being at risk for malnutrition (score ≥ 3) according to the validated Icelandic Nutrition Screening Tool [22], and had given their written informed consent. Excluded were those with known dietary allergies/being on a special diet, severe chronic kidney disease (glomerular filtration rate < 30 mL/min/1.73 m2), in active cancer treatment, receiving tubal feeding, not being able to communicate with the research team, cognitive function ≤20 according to the Mini Mental State Examination (MMSE) [23], and not having access to a functioning kitchen at home (i.e., refrigerator, oven, or microwave oven). Of the 1003 screened potential participants, n = 897 were ineligible for participation in the study. They were ineligible as they were too sick to participate, had been discharged, deceased, scored <20 on the MMSE, had been admitted to a nursing home, were not community dwelling, relying on tubal feeding, were <65 years of age, were not living in the capital area, or had declined participation (Fig. 1).
Randomization
The participants were randomly allocated to either the intervention or the control group by using a random number generated as implemented by the Statistical Package for the Social Sciences (SPSS, version 26.0, SPSS, Chicago, IL, USA).
Intervention group
The participant received nutrition therapy from the clinical nutritionist consisting of five home visits (1 day after discharge and one-, three-, six- and twelve weeks later) and three telephone calls in between the home visits. The nutrition therapy was implemented following the principles of Nutrition Care Process, which entails the following: nutritional assessment, diagnosis, intervention, monitoring, and evaluation of the nutrition therapy [16]. During the dietary counselling sessions, family members, relatives, friends, or home-care workers were invited to join as well. At the initial visit after discharge, the participant was educated about the importance of adequate energy and protein intake [24]. Nutrition-related problems were identified during the interviews, and suggestions given to resolve them. In addition to the dietetic counselling, participants received free supplemental energy- and protein-rich foods (1 hot meal/day and 2 in-between-meals/day; Supplementary Table 1) delivered once a week. During the first home delivery, study staff educated the participants on how to store the meals, how to open the packages and how to heat the meals.
Control group
At discharge, the control group received a booklet on good nutrition during aging published by The Icelandic Medical Directorate [24] and were encouraged to order MOW without any further dietary counselling during the study period, reflecting current standard care in Iceland for older adults discharged from hospital.
Participant characteristics
Background variables, e.g., age, sex, education, living arrangements, alcohol use and smoking habits, were assessed using questionnaires. Additional variables were collected from the Icelandic electronic hospital registry SAGA (TM software 3.1.39.9), e.g., height, number of diagnoses according to the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10), and number of different medications.
Outcomes assessed
All primary and secondary outcome measurements were conducted at baseline (at the hospital) and at endpoint (at the participants’ homes). These measurements were conducted in a predefined order and questions on food or diet were asked only at the very end of each assessment. As the outcome assessors (who did not deliver the intervention) were unaware whether a participant was in the control or intervention group, measurements of anthropometrics, physical function, muscular strength, and nutritional status were blinded.
Anthropometrics
Body weight was measured in light underwear/clothing on a calibrated scale (model no. 708, Seca, Hamburg, Germany) and height was taken from the Icelandic electronic hospital registry SAGA (TM software 3.1.39.9). Body mass index (BMI) was calculated from the height and weight (kg/m2). Participants were categorized into three BMI categories: low BMI < 23 kg/m2, middle BMI 23–30 kg/m2, or high BMI ≥ 30 kg/m2 [24]. Body composition was measured using a hand-held bioelectrical impedance analysis device (BIA, Omron HBF-306C, Kyoto, Japan) [25]. Calf circumference was measured in a seated position. The tape was wrapped around the right calf and moved up and down to locate the maximum circumference in a plane perpendicular to the long axis of the calf [26]. Midarm circumference was also measured in a seated position and was taken on the left upper arm, at the mid-point between the tip of the shoulder and the tip of the elbow (olecranon process and the acromion) [27].
Physical function
Physical function was assessed using the SPPB, which evaluates lower extremity function assessing (1) usual-paced gait speed over a four-meter-course, (2) standing balance, and (3) time to rise from a chair five times. For each test, a score of 0 to 4 is assigned using cut points [28]. The three test scores are summed, yielding a range from 0 to 12. As SPPB testing in this study was performed at the participants’ homes, it was shortened for practical reasons, and thus did not include the gait speed part. The possible score therefore ranged from 0 to 8. Additionally, participants were asked the question “Do you have difficulties walking?” (Yes vs. no).
Muscle strength
Handgrip strength was measured in a seated position with a hydraulic hand dynamometer (Baseline® Baseline Evaluations Corporation) set on position two and the maximal grip strength of two trials was registered as the subject’s grip force in kilograms using their dominant hand [27].
Dietary intake
Dietary intake was assessed using a 24-hour-dietary-recall interview (24-HR) to obtain estimates of intakes of fluids, energy, and energy-giving nutrients [29,30,31,32,33,34]. The results from the 24-HR were entered into the nutrition calculation program ICEFOOD originally developed for the National Survey of Icelandic Diet 2002 and continuously updated for consequent National Surveys of Icelandic Diet (2011 and currently ongoing) [35]. ICEFOOD relies on the Icelandic database of the chemical composition of food (ISGEM within the Icelandic Medical Directorate of Health) and on a database within the Medical Directorate containing information on several hundred recipes of common dishes and ready-to-eat meals on the Icelandic market [35, 36]. Additional food-related questions and frequency of intakes of hot meals, major food groups, and liquids were assessed at endpoint using a simple food frequency questionnaire [37].
Nutritional status and food-related adverse events
Nutritional status was assessed using the Icelandic Nutrition Screening Tool as recommended by the Icelandic Medical Directorate of Health [24]. This validated questionnaire [22] consists of 13 questions which are scored and summed, yielding a range from 0 to 30. A clinical nutritionist also assessed whether any food- related digestion issues, such as diarrhoea, nausea, constipation, or stomach pain, were experienced during the intervention.
Sample size considerations
Sample size calculations based on our previous studies on body weight change [19, 38] suggest that the number of participants n = 44 in each group was estimated to be sufficient to detect a body weight difference of 1.8 ± 3.0 kg between groups as significant. The corresponding numbers for SPPB were n = 45 in each group, detecting a significance by 1 as significant (assuming SD = 1.7) [39]. The recruitment of >50 participants in each group allowed around 10% drop out to still retain sufficient statistical power.
Statistical analysis
Data were analysed using statistical software (SPSS, version 26.0, SPSS, Chicago, IL, USA). Data were checked for normality using the Kolmogorov–Smirnov test. Data are presented as mean ± standard deviation (SD). Differences between groups at baseline were calculated using independent samples’ t-test (normally distributed variables) or Mann–Whitney U-test (not normally distributed variables). We used intention-to-treat analysis.
Despite randomization, sex distribution was slightly uneven between treatment and control groups. As a result, we corrected for sex in all multivariate statistical endpoint analyses. Unadjusted analyses are also presented for comparison as supplemental material (Supplementary Table 2). Differences in anthropometrics and physical outcomes (continuous variables) between the groups at endpoint were assessed using linear mixed models in SPSS. Results are shown as parameter estimates, in which B describes the estimated and adjusted differences in the outcome variables between groups.
Differences in the abilities to perform physical tasks (single items from SPPB and “Do you have difficulties walking?” all categorical variables, yes vs. no) between the groups at endpoint were assessed using a logistic regression model, in which we corrected for the corresponding baseline values and sex.
Subgroup analysis was performed by comparing body weight changes between intervention and control in subgroups of males vs. females, married/cohabitating vs. single/divorced/alone, and low BMI group vs. middle BMI group vs. high BMI group. The effects of the intervention within subgroups were investigated using an independent samples’ t-test (for two variable subgroups) or ANOVA including LSD post hoc test (for three variable subgroups). We tested for interaction between subgroups and intervention using a general linear model.
Endpoint calculations represent per-protocol analysis with those dropping out of the intervention included in the baseline, but not in endpoint assessment. The level of significance was set at P < 0.05.
Results
During the recruitment period, 1003 subjects were screened and of those 106 were recruited and randomized. Two subjects dropped out during the study period, one from each group (Fig. 1). The study was carried out as planned and all participants in the intervention group (with exception of the one dropout) received five home visits and three phone calls. No discomfort or adverse events relating to the intervention were observed among study participants.
Baseline characteristics of the participants are shown in Table 1. The intervention and control groups were similar in most measures, with the exception that there were significantly more females in the intervention group compared to controls (72 vs 53%). In agreement with this uneven sex distribution, the intervention group also had a higher body fat percentage (borderline significant).
Concerning the primary outcome, individual changes in body weight for participants in both groups are shown in Fig. 2. The intervention group experienced in absolute terms significant weight gain during the intervention period (1.7 kg ± 2.5 kg; which equals approximately 2% of body weight, 1 out of 53 individuals lost >1 kg body weight), while significant weight loss was observed among controls (−3.5 ± 3.9 kg; which equals approximately 5% of body weight, 42 out of 53 individuals lost >1 kg body weight). After adjustment for sex (Table 2) this corresponded to 5.1 kg (95% CI: 3.9, 6.4) higher body weight in the intervention group at endpoint compared to controls. The corresponding adjusted difference in lean body mass was 4.2 kg (95% CI: 2.7, 5.6). For other anthropometric outcomes, i.e., BMI, waist-, midarm- and calf circumference, the sex adjusted differences between groups showed significantly lower values in the control group (Table 2).
As expected, the highest increase in body weight was observed in participants in the low or middle BMI categories (Table 3). The unadjusted means for all anthropometric measures at baseline and endpoint are also shown in Supplementary Table 2.
With respect to measures of physical function, the SPPB score was significantly higher in the intervention group at endpoint (Table 2) and subjects in the intervention group were also more likely to improve in single physical performance tasks at endpoint (adjusted results in Table 4 and unadjusted results in Supplementary Table 2). Handgrip strength did not differ statistically between the groups at endpoint (Table 2).
In terms of nutritional status, the Icelandic Nutrition Screening Tool score at endpoint was significantly higher (higher score corresponds to a worse nutritional status) among controls compared to the intervention group (Table 2). No difference in dietary intake between the two groups were detected at baseline (i.e., at the hospital) but energy and macronutrient intake increased significantly in the intervention group and decreased significantly in the control group during the intervention period (Table 5). In the intervention group, ONS provided 24 and 29% of the total energy and protein at endpoint (which equals approximately 1.75 ONS servings/day), respectively. At endpoint, more than 94% of the intervention group also stated that they liked the provided food, reported a higher frequency of hot meals consumed, more frequent consumption of meat, and a higher intake of liquids compared to controls. No food related digestion issues, such as diarrhoea, nausea, constipation, or stomach pain were reported.
In terms of stability analyses our analyses indicated (Table 3) that neither sex, marital status, nor participant age affected the efficacy of the intervention. However, body weight changes differed by BMI categories and interaction between BMI categories and intervention was significant (P = 0.027).
Discussion
In this 6-month randomized, controlled intervention we examined the effects of nutrition therapy provided by a clinical nutritionist following the principles of NCP [16] in combination with freely delivered supplemental energy- and protein-dense foods in older adults after discharge from hospital. We found that this nutrition intervention had strong beneficial effects on body weight and other anthropometric measures; as well as SPPB score, and nutritional status. The observed effects in our study were more pronounced than what has been reported in previous nutritional interventions not combining ONS, MOW, and nutrition therapy from a nutritionist.
Changes in body weight were observed in both groups, with an average of 5.1 kg higher body weight (which equals roughly a 7% difference in body weight) among those receiving the intervention, who gained a moderate amount of weight, compared to controls, who lost weight, which agrees with changes in dietary intake recordings after hospital discharge. The fact that 42 out of 53 of participants in the control group lost more than 1 kg body weight while only one individual in the intervention lost that much weight demonstrates that individual and targeted nutrition therapy in combination with the provision of ONS and MOW, can largely prevent negative alterations in body weight after hospital discharge.
There are currently no studies available in public literature that use the combination of nutrition therapy, home delivered food, and ONS in older adults which would allow direct comparison of the results. However, two recent trials using three home visits by a registered dietitian as intervention showed significant body weight gain in discharged patients, resulting in significant endpoint differences of 1.4–1.8 kg (~2–3% of body weight) between intervention and control [14, 15], although these studies were shorter in length (12 weeks) and did not deliver food items. Recent review articles on the efficacy of ONS, MOW and dietary advice [9, 37, 40, 41] to increase dietary intake and body weight yielded results in the range of 200–400 kcal/d and 0.6–1.5 kg (~1.5-2% of body weight), respectively. Although significant, the effect sizes were small and possibly, long-term compliance to, e.g., ONS or MOW, decreases over time and ONS might displace food rather than serve as an addition to regular dietary intake in the long run [42, 43].
Although it is difficult to accurately estimate body composition during a home visit, we employed various methods (hand-held BIA, upper arm- and calf circumference) to get insight into changes in lean body mass during the intervention. Results from the various measurements were consistent and data from BIA showed that weight loss in the control group was mainly due to loss of lean body mass, and weight gain in the intervention group was mainly due to an increase in lean body mass (and not body fat).
In the present study the nutrition intervention also had favourable effects on physical function, although we could not detect any changes in muscular strength. We found that both objectively measured physical function (SPPB) as well as subjectively experienced difficulties in walking improved only in the intervention group during the 6 months. In general, the evidence on the effects of nutrition intervention on physical function and muscular strength in older adults is limited. Although several studies using either MOW or ONS found effects on physical function [44, 45] and muscular strength [44], other studies did not (physical function: [46], muscular strength: [45, 47,48,49]).
In the present study, dietary intake at baseline was similar between groups at around 1500 kcal and 75 g protein per day which reflects the food provided by the hospital. Similar numbers have been previously reported by other investigators as well [50]. However, after discharge, the dietary intake decreased dramatically in the control group despite being informed at discharge of the importance of nutrition, while intake increased considerably in the intervention group. Interestingly, a low dietary intake nearly identical to the control group’s intake was observed in a small pilot study in discharged hospital patients conducted by our research group in 2016 [19].
The results from our study are of potential public health importance for the following reasons: It is known that malnutrition is common in hospitalized older adults [1, 2, 51, 52] and unfortunately, our study demonstrates that weight loss continues after discharge in most participants who receive standard care, which has also been observed to some extent by other researchers [53]. Further, the treatment effects of our intervention, utilizing three components to improve nutritional status, were higher than reported from other studies having used only single modalities of nutrition intervention, e.g., ONS, MOW, or dietary advice [9, 40, 54,55,56,57]. It seems obvious that the wider approach of our nutrition therapy based on principles of NCP, in combination with the delivery of a variety of foods that were highly energetic and rich in protein while leaving space for individual needs and personal preferences, resulted in high acceptance of the delivered foods even after 6 months, satisfactory dietary intake, and body weight gain.
The current intervention was successful in improving body weight and maintaining muscle mass in discharged patients. The subgroup analysis indicated that the treatment effects were similar between subgroups, except in the three BMI categories, where participants in the high BMI category gained less body weight than participants in the middle and low BMI categories, which simply reflects different aims of the nutrition therapy dependent on individual characteristics of the participants. In our opinion the success of our study can be attributed to (1) the individualized and frequent nutritional therapy performed by a dedicated clinical nutritionist, (2) the provision of food developed to be palatable for older adults, rich in energy and protein as well as with the appropriate texture; and (3) the length of the intervention being 6 months leading to significant improvements in both nutritional status and physical function.
Strengths and limitations
It is a strength of the present study that it was a randomized, controlled trial with very low drop out and 100% delivery of the intended intervention in 52 of 53 participants. Although a study like this cannot be doubly blinded, it is of importance that the assessment of the main outcomes was single blinded. We think that both the time length (6 months) and the intensity of intervention (five visits, three phone calls and free home delivered food) were appropriate to be able to observe potential treatment effects.
There are several limitations to our study. One is the gender imbalance between the control and the intervention group. Despite this gender imbalance our adjusted and unadjusted outcomes reach the same conclusion; nearly all subjects in the control group lost weight while almost all in the intervention group gained or maintained their weight, which cannot be explained by sex alone. Also, with our sample size being 106, some imbalances in the baseline factors can be expected and the method used for randomization was valid. Another limitation was that as outcome measurements were conducted at the patients’ homes, we were limited in the assessment of physical function, i.e., lacking a measurement of gait speed, as well as in the measurement of body composition, i.e., having to rely on hand-held BIA and circumference measurements. However, we still collected valuable information about both body composition and physical function from which we can draw solid conclusions.
Conclusion
Our study shows that the time after hospital discharge leads to weight loss and loss of muscle mass, a decrease in food intake, and a deterioration in nutritional status in most older adults receiving the current standard care in Iceland. However, a 6-month nutrition therapy provided by a clinical nutritionist, following the principles of NCP in combination with freely delivered supplemental energy- and protein-dense foods, has beneficial effects on body weight, physical function, dietary intake, and nutritional status. The treatment effects were consistent across subgroups of study participants.
Data availability
Data described in the manuscript, code book, and analytic code are publicly and freely available without restriction at: [https://eur02.safelinks.protection.outlook.com/?url=https%3A%2F%2Fdataverse.harvard.edu%2Fdataset.xhtml%3FpersistentId%3Ddoi%3A10.7910%2FDVN%2F38X3LX&data=04%7C01%7Cbsb6%40hi.is%7C1e998a8333904a1087a008d9803f56dd%7C09fa5f0e211846568529677ed8fdbe78%7C0%7C0%7C637681831802708546%7CUnknown%7CTWFpbGZsb3d8eyJWIjoiMC4wLjAwMDAiLCJQIjoiV2luMzIiLCJBTiI6Ik1haWwiLCJXVCI6Mn0%3D%7C1000&sdata=LJU6Bm%2F9up1VO8rsWUdMnf5d5WewkRQpRUzfpmr8GgM%3D&reserved=0].
References
Corcoran C, Murphy C, Culligan EP, Walton J, Sleator RD. Malnutrition in the elderly. Sci Prog. 2019;102:171–80. https://doi.org/10.1177/0036850419854290.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC. et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr (Edinb, Scotl). 2017;36:49–64. https://doi.org/10.1016/j.clnu.2016.09.004.
Chan R, Leung J, Woo J, Kwok T. Associations of dietary protein intake on subsequent decline in muscle mass and physical functions over four years in ambulant older Chinese people. J Nutr Health Aging. 2014;18:171–7. https://doi.org/10.1007/s12603-013-0379-y.
Houston DK, Tooze JA, Garcia K, Visser M, Rubin S, Harris TB. et al. Protein intake and mobility limitation in community-dwelling older adults: the health ABC study. J Am Geriatr Soc. 2017;65:1705–11. https://doi.org/10.1111/jgs.14856.
Scott D, Blizzard L, Fell J, Giles G, Jones G. Associations between dietary nutrient intake and muscle mass and strength in community-dwelling older adults: the Tasmanian Older Adult Cohort Study. J Am Geriatr Soc. 2010;58:2129–34. https://doi.org/10.1111/j.1532-5415.2010.03147.x.
Avelino-Silva TJ, Jaluul O. Malnutrition in hospitalized older patients: management strategies to improve patient care and clinical outcomes. Int J Gerontol. 2017;11:56–61. https://doi.org/10.1016/j.ijge.2016.11.002.
Ijmker-Hemink VE, Dijxhoorn DN, Briseno Ozumbilla CM, Wanten GJA, van den Berg MGA. Effective elements of home-delivered meal services to improve energy and protein intake: A systematic review. Nutr (Burbank, Los Angeles Cty, Calif). 2020;69:110537. https://doi.org/10.1016/j.nut.2019.06.018.
Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Goisser S, Hooper L. et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr (Edinb, Scotl). 2019;38:10–47. https://doi.org/10.1016/j.clnu.2018.05.024.
Correa-Pérez A, Abraha I, Cherubini A, Collinson A, Dardevet D. de Groot LCPGM et al. Efficacy of non-pharmacological interventions to treat malnutrition in older persons: A systematic review and meta-analysis. The SENATOR project ONTOP series and MaNuEL knowledge hub project. Ageing Res Rev. 2019;49:27–48. 10.1016/j.arr.2018.10.011.
Bandayrel K, Wong S. Systematic literature review of randomized control trials assessing the effectiveness of nutrition interventions in community-dwelling older adults. J Nutr Educ Behav. 2011;43:251–62. https://doi.org/10.1016/j.jneb.2010.01.004.
Feldblum I, German L, Castel H, Harman-Boehm I, Shahar DR. Individualized nutritional intervention during and after hospitalization: the nutrition intervention study clinical trial. J Am Geriatr Soc. 2011;59:10–17. https://doi.org/10.1111/j.1532-5415.2010.03174.x.
Ha L, Hauge T, Spenning AB, Iversen PO. Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: A randomized, controlled trial. Clin Nutr. 2010;29:567–73. https://doi.org/10.1016/j.clnu.2010.01.011.
Ingstad K, Uhrenfeldt L, Kymre IG, Skrubbeltrang C, Pedersen P. Effectiveness of individualised nutritional care plans to reduce malnutrition during hospitalisation and up to 3 months post-discharge: a systematic scoping review. BMJ Open. 2020;10:e040439. https://doi.org/10.1136/bmjopen-2020-040439.
Beck A, Andersen UT, Leedo E, Jensen LL, Martins K, Quvang M. et al. Does adding a dietician to the liaison team after discharge of geriatric patients improve nutritional outcome: a randomised controlled trial. Clin Rehabilitation. 2015;29:1117–28. https://doi.org/10.1177/0269215514564700.
Beck AM, Kjaer S, Hansen BS, Storm RL, Thal-Jantzen K, Bitz C. Follow-up home visits with registered dietitians have a positive effect on the functional and nutritional status of geriatric medical patients after discharge: a randomized controlled trial. Clin Rehabilitation. 2013;27:483–93. https://doi.org/10.1177/0269215512469384.
Swan WI, Vivanti A, Hakel-Smith NA, Hotson B, Orrevall Y, Trostler N. et al. Nutrition care process and model update: toward realizing people-centered care and outcomes management. J Acad Nutr Diet. 2017;117:2003–14. https://doi.org/10.1016/j.jand.2017.07.015.
Mañas A, Del Pozo-Cruz B, García-García FJ, Guadalupe-Grau A, Ara I. Role of objectively measured sedentary behaviour in physical performance, frailty and mortality among older adults: A short systematic review. Eur J Sport Sci. 2017;17:940–53. https://doi.org/10.1080/17461391.2017.1327983.
Ritchie CS, Locher JL, Roth DL, McVie T, Sawyer P, Allman R. Unintentional weight loss predicts decline in activities of daily living function and life-space mobility over 4 years among community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008;63:67–75.
Blondal BS. Nutritional status of the elderly after discharge from the acute geriatric unit, a pilot study: Socioeconomic status, food security and food availability. MSc, University of Iceland, Digital repository of academic and research documents, 2017.
Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P. CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167:40–47. https://doi.org/10.7326/m17-0046.
World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Int Bioethique. 2004;15:124–9
Thorsdottir I, Gunnarsdottir I, Eriksen B. Screening method evaluated by nutritional status measurements can be used to detect malnourishment in chronic obstructive pulmonary disease. J Am Diet Assoc. 2001;101:648–54. https://doi.org/10.1016/s0002-8223(01)00163-8.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Gisladottir ETH, Geirsdottir OG, Jonsdottir AB, Jensdottir AB, Jonsdottir G, Hilmisdottir HB, et al. Ráðleggingar um mataræði fyrir hrumt eða veikt eldra fólk - ætlað fagfólki og öðrum umönnunaraðilum [Dietary advice for frail or sick old adults - for professionals and other caregivers]. In, 2018.
Ramel A, Geirsdottir OG, Arnarson A, Thorsdottir I. Regional and total body bioelectrical impedance analysis compared with DXA in Icelandic elderly. Eur J Clin Nutr. 2011;65:978–83. https://doi.org/10.1038/ejcn.2011.65.
Portero-McLellan KC, Staudt C, Silva FR, Delbue Bernardi JL, Baston Frenhani P, Leandro Mehri VA. The use of calf circumference measurement as an anthropometric tool to monitor nutritional status in elderly inpatients. J Nutr Health Aging. 2010;14:266–70. https://doi.org/10.1007/s12603-010-0059-0.
Damayanthi HDWT, Moy F-M, Abdullah KL, Dharmaratne SD. Handgrip strength and its associated factors among community-dwelling elderly in Sri Lanka: A cross-sectional study. Asian Nurs Res. 2018;12:231–6. https://doi.org/10.1016/j.anr.2018.08.008.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG. et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. https://doi.org/10.1093/geronj/49.2.m85.
Bauer JM, Kaiser MJ, Sieber CC. Evaluation of nutritional status in older persons: nutritional screening and assessment. Curr Opin Clin Nutr Metab care. 2010;13:8–13. https://doi.org/10.1097/MCO.0b013e32833320e3.
Zhai F-Y, Guo X, Popkin BM, Ma L, Wang Q, Yu W, et al. Evaluation of the 24-hour individual recall method in China. Food Nutr Bull. 1996;17:154–61.
Ma Y, Olendzki BC, Pagoto SL, Hurley TG, Magner RP, Ockene IS. et al. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol. 2009;19:553–9. https://doi.org/10.1016/j.annepidem.2009.04.010.
Kirkpatrick SI, Subar AF, Douglass D, Zimmerman TP, Thompson FE, Kahle LL. et al. Performance of the automated self-administered 24-hour recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am J Clin Nutr. 2014;100:233–40. https://doi.org/10.3945/ajcn.114.083238.
Riobo Servan P, Sierra Poyatos R, Soldo Rodriguez J, Gomez-Candela C, Garcia Luna PP, Serra-Majem L. Special considerations for nutritional studies in elderly. Nutricion Hospitalaria. 2015;31:84–90.
Tooze JA, Vitolins MZ, Smith SL, Arcury TA, Davis CC, Bell RA, et al. High levels of low energy reporting on 24-hour recalls and three questionnaires in an elderly low-socioeconomic status population. J Nutr. 2007;137:1286–93.
Thorgeirsdottir HVH, Gunnarsdottir I, Gisladottir E, Gunnarsdottir BE, Thorsdottir I What do Icelanders eat 2010-1. Main results. In: Embætti Landlæknis MoRín, (ed). https://www.landlaeknir.is/servlet/file/store93/item14901/Hva%C3%B0%20bor%C3%B0a%20%C3%8Dslendingar_april%202012.pdf: Landlæknir, 2012.
Gunnarsdottir I, Tryggvadottir EA, Birgisdottir BE, Halldorsson TI, Medek H, Geirsson RT. [Diet and nutrient intake of pregnant women in the capital area in Iceland]. Laeknabladid. 2016;102:378–84. https://doi.org/10.17992/lbl.2016.09.95.
Eysteinsdottir T, Thorsdottir I, Gunnarsdottir I, Steingrimsdottir L. Assessing validity of a short food frequency questionnaire on present dietary intake of elderly Icelanders. Nutr J. 2012;11:12–12. https://doi.org/10.1186/1475-2891-11-12.
Thorsdottir I, Tomasson H, Gunnarsdottir I, Gisladottir E, Kiely M, Parra MD. et al. Randomized trial of weight-loss-diets for young adults varying in fish and fish oil content. Int J Obes (Lond). 2007;31:1560–6. https://doi.org/10.1038/sj.ijo.0803643.
Losa-Reyna J, Baltasar-Fernandez I, Alcazar J, Navarro-Cruz R, Garcia-Garcia FJ, Alegre LM. et al. Effect of a short multicomponent exercise intervention focused on muscle power in frail and pre frail elderly: A pilot trial. Exp Gerontol. 2019;115:114–21. https://doi.org/10.1016/j.exger.2018.11.022.
Baldwin C, Weekes CE. Dietary advice with or without oral nutritional supplements for disease-related malnutrition in adults. Cochrane Database Syst Rev. 2011;2011:Cd002008.
Munk T, Tolstrup U, Beck AM, Holst M, Rasmussen HH, Hovhannisyan K. et al. Individualised dietary counselling for nutritionally at-risk older patients following discharge from acute hospital to home: a systematic review and meta-analysis. J Hum Nutr dietetics: Off J Br Dietetic Assoc. 2016;29:196–208. https://doi.org/10.1111/jhn.12307.
Geirsdottir OG, Arnarson A, Briem K, Ramel A, Jonsson PV, Thorsdottir I. Effect of 12-week resistance exercise program on body composition, muscle strength, physical function, and glucose metabolism in healthy, insulin-resistant, and diabetic elderly Icelanders. J Gerontol A Biol Sci Med Sci. 2012;67:1259–65. https://doi.org/10.1093/gerona/gls096.
Arnarson A, Gudny Geirsdottir O, Ramel A, Briem K, Jonsson PV, Thorsdottir I. Effects of whey proteins and carbohydrates on the efficacy of resistance training in elderly people: double blind, randomised controlled trial. Eur J Clin Nutr. 2013;67:821–6. https://doi.org/10.1038/ejcn.2013.40.
Lindhardt T, Nielsen MH. Older patients’ use of technology for a post-discharge nutritional intervention - A mixed-methods feasibility study. Int J Med Inf. 2017;97:312–21. https://doi.org/10.1016/j.ijmedinf.2016.10.017.
Kim CO, Lee KR. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: a community-based randomized controlled study. J Gerontol A Biol Sci Med Sci. 2013;68:309–16. https://doi.org/10.1093/gerona/gls167.
Denissen KF, Janssen LM, Eussen SJ, van Dongen MC, Wijckmans NE, van Deurse ND. et al. Delivery of nutritious meals to elderly receiving home care: feasibility and effectiveness. J Nutr Health Aging. 2017;21:370–80. https://doi.org/10.1007/s12603-016-0790-2.
Edington J, Barnes R, Bryan F, Dupree E, Frost G, Hickson M. et al. A prospective randomised controlled trial of nutritional supplementation in malnourished elderly in the community: clinical and health economic outcomes. Clin Nutr (Edinb, Scotl). 2004;23:195–204. https://doi.org/10.1016/s0261-5614(03)00107-9.
Price R, Daly F, Pennington CR, McMurdo ME. Nutritional supplementation of very old people at hospital discharge increases muscle strength: a randomised controlled trial. Gerontology. 2005;51:179–85. https://doi.org/10.1159/000083991.
Kretser AJ, Voss T, Kerr WW, Cavadini C, Friedmann J. Effects of two models of nutritional intervention on homebound older adults at nutritional risk. J Am Diet Assoc. 2003;103:329–36. https://doi.org/10.1053/jada.2003.50052.
Ingadottir AR, Beck AM, Baldwin C, Weekes CE, Geirsdottir OG, Ramel A. et al. Association of energy and protein intakes with length of stay, readmission and mortality in hospitalised patients with chronic obstructive pulmonary disease. Br J Nutr. 2018;119:543–51. https://doi.org/10.1017/s0007114517003919.
World Health Organization. Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity. World Health Organization. 2017. https://apps.who.int/iris/handle/10665/258981.
van Bokhorst-de van der Schueren MAE, Lonterman-Monasch S, de Vries OJ, Danner SA, Kramer MHH, Muller M. Prevalence and determinants for malnutrition in geriatric outpatients. Clin Nutr. 2013;32:1007–11. https://doi.org/10.1016/j.clnu.2013.05.007.
Laur C, Curtis L, Dubin J, McNicholl T, Valaitis R, Douglas P et al. Nutrition care after discharge from hospital: an exploratory analysis from the more-2-eat study. Healthcare (Basel). 2018;6. https://doi.org/10.3390/healthcare6010009.
Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A. et al. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev. 2013;12:967–81. https://doi.org/10.1016/j.arr.2013.06.002.
Collins J, Porter J. The effect of interventions to prevent and treat malnutrition in patients admitted for rehabilitation: a systematic review with meta-analysis. J Hum Nutr dietetics: Off J Br Dietetic Assoc. 2015;28:1–15. https://doi.org/10.1111/jhn.12230.
Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2009;2009:Cd003288.
Poscia A, Milovanovic S, La Milia DI, Duplaga M, Grysztar M, Landi F. et al. Effectiveness of nutritional interventions addressed to elderly persons: umbrella systematic review with meta-analysis. Eur J Public Health. 2018;28:275–83. https://doi.org/10.1093/eurpub/ckx199.
Acknowledgements
The authors also want to thank the study staff for their dedicated work, i.e., Ósk Guðmundsdóttir, Elfa Björk Rúnarsdóttir and Gunnhildur Olga Jónsdóttir as well as the Icelandic food companies Sláturfélag Suðurlands Ltd., Grimur kokkur Ltd. and MS Iceland Dairies for the collaboration and delivery of food items.
Funding
The study was funded by the Icelandic Centre for Research (174250-051), the Research Fund of the University of Iceland, the Research Fund of Hrafnista, the Icelandic Society of Geriatrics, and the Helga Jonsdottir and Sigurlidi Kristjansson Geriatric Research Fund. The authors want to state that neither the above-mentioned funding entities nor the food companies were involved in study design, implementation, statistical analysis, and/or interpretation of the data. The above-mentioned funding sources were not involved in study design; data collection, analysis, interpretation of data, writing of the report, and had no restrictions regarding the submission of the report for publication.
Author information
Authors and Affiliations
Contributions
BSB, OGG, KS, AMB, PVJ, and AR designed research; BSB and AR conducted research; BSB and AR analysed data; BSB, OGG, KS, AMB, PVJ, TIH, and AR wrote paper; AR had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blondal, B.S., Geirsdottir, O.G., Beck, A.M. et al. HOMEFOOD randomized trial—beneficial effects of 6-month nutrition therapy on body weight and physical function in older adults at risk for malnutrition after hospital discharge. Eur J Clin Nutr 77, 45–54 (2023). https://doi.org/10.1038/s41430-022-01195-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01195-2
This article is cited by
-
HOMEFOOD Randomised Trial–Six-Month Nutrition Therapy in Discharged Older Adults Reduces Hospital Readmissions and Length of Stay at Hospital Up to 18 Months of Follow-Up
The Journal of nutrition, health and aging (2023)