Abstract
Background/Objectives
Northeastern Indian region has a high density of marginalised populations with a concerning quality of health services. We observed the trends in prevalence of infectious diseases and nutritional disorders among children under-five years from 2006 to 2020 in the Northeastern states. We also assessed the distribution of their burden by place of residence.
Methods
A secondary data analysis of select indicators on infectious diseases and nutritional disorders in seven Northeastern states across three rounds of the National Family Health Survey (2005–06, 2015–16, 2019–20) was undertaken. We calculated outcome indicator mean prevalence, relative change and average annual rates of reduction of the indicators.
Results
A significant relative reduction between 2006–2020 in the prevalence of diarrhoea (0.4 [95CI:0.7,0.1]) at p < 0.05; acute respiratory illness (ARI) (0.7 [95CI:0.1,0.4]), stunting (0.3 [95CI: 0.3,0.12]) and underweight (0.3 [95CI:0.5,0.2]) at p < 0.001 were noted. However, overweight prevalence increased (10.1[95CI:4.3,16.0, p < 0.001]) due to a low annual reduction rate. The highest annual reduction rates were observed in Sikkim and Tripura for diarrhoea and ARI respectively (>10.0%), and in Meghalaya for wasting and severely wasting (6.3%). Rural areas had a higher burden of stunting, wasting (including severe), underweight, anaemia and diarrhoea; overweight was seen in both rural and urban settings.
Conclusion
Significant reductions were observed in ARI, diarrhoea, stunting and underweight prevalence between 2006–2020, with sub-regional variations and a greater burden in rural areas. During this period, overweight prevalence worsened; and anaemia showed a large increase from 2016. To reduce the equity-gap, programmes should be adapted to meet the differential needs of the Northeastern states.
Similar content being viewed by others
Background
Improving child health and nutrition have long been public health priorities. Over the last two decades, along with considerable gains in child health outcomes, there has been a decline in the global prevalence of childhood undernutrition- commonly measured as stunting, underweight and wasting; with a steady rise in overweight [1]. Nevertheless, the present levels of overall malnutrition (under-and over-nutrition) remain concerning.
South Asian countries- primarily driven by India- contribute the highest to the total numbers of malnourished children, and diarrhoeal and pneumonia-associated child deaths globally [2, 3]. In India, these factors along with poor environment and maternal nutrition chiefly lead to the high Under-five Mortality Rate (U5MR) [4].
India has made significant strides in reducing U5MR from 126.0 to 34.0 per 1,000 live births from 1990 to 2019. Despite this, it substantially lags behind high-income regions such as Europe (U5MR- 5.0 per 1,000 live births) [5, 6]. Moreover, India is still not on track to achieve any of the required 2025 reduction targets set by the World Health Organisation’s (WHO) Global Nutrition Targets and Global Action Plan for the Prevention and Control of Pneumonia and Diarrhoea [7,8,9]. India also ranks at the bottom of the Global Hunger Index 2021 with negligible change in the index from 2012 [10], indicating poor progress and an alarmingly high percentage of undernourished children.
India witnesses significant sub-national variations in critical child health indicators, which are masked within national-level estimates. Northeastern (NE) region not only has substantially higher U5MR compared to the national average (63.8 vs 47.8 per 1000 live births) and other Indian regions [11], but some NE states also contribute the highest proportion of undernourished children in India [12]. Despite a high burden, most of India’s child health schemes [13, 14] are focused around the populous and under-developed Central region with an intent to save more lives. This has inadvertently resulted in a relative lack of visibility of child health outcomes of the NE states. These factors combined with the unique geographical and socio-cultural conditions warrants deeper analyses and programmatic efforts in the Northeast. Moreover, sparse literature on the progress of child health indicators and policy action in NE contributes to lesser policy and programme attention in these states.
Given the above context, we sought to analyse and discuss key child health trends that contribute to the U5MR [11] in the NE region of India using the National Family Health Survey (NFHS). This paper brings forth policy areas requiring attention, specifically in the Northeast, that could aid effective programme planning by providing an insight into the contextual need.
Methods
We comparatively analysed the emerging trends of infectious diseases and nutritional disorders among children under-five years between 2006–2020 in Northeastern Indian states. The distribution of the health outcome by place of residence in 2020 was also assessed. This paper discusses the breadth of the findings with existing literature and comments on the policy and programmatic implications for these states.
Study design
Descriptive secondary data analysis was conducted using NFHS-3, NFHS-4 and NFHS-5 Phase-1 (factsheet) [15]. NFHS-3 was conducted in 2005-06, NFHS-4 in 2015-16 and NFHS-5 between 2019–2020. However, owing to COVID-19 related disruptions in 2020, factsheets from only 17 states and five union territories were released as part of the Phase-1 issue for NFHS-5. The data characteristics by rounds including sample size and data collection periods are presented in Supplementary (S1).
Study setting
NE region includes eight geographical states- Assam, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim, Tripura and Arunachal Pradesh. This analysis includes seven of the eight NE states and excludes Arunachal Pradesh due to it not being included in Phase-1.
NE states are forested mountainous regions that are rich in biodiversity. Connected to mainland India by a narrow land, they account for almost a tenth of total India’s geography [16] and are bordered by neighbouring countries. NE region has almost the same literacy rate as India, including women; however, the majority of states have substantially higher overall unemployment rates and lower per-capita income than the national average [17]. They have the highest density of tribal population and are culturally distinct from other Indian regions(S2). Most of the NE states experience frequent armed communal violence which impacts essential services [18] that are exacerbated by climate adversities, ill-equipped health facilities and geographically inaccessible regions in some states [19].
Data source
The Demographic Health Survey (DHS) of India- popularly known as the NFHS- is a nationally representative multi-round survey informing on the health and socio-demographic factors in India [15]. NFHS maintains data quality by pre-testing questionnaires, training surveyors and maintaining adequate gender mixes for sensitive questions. The questionnaires are translated into Hindi and English languages and administered in local languages. NFHS further employs a two-stage stratification sampling- selection of Primary Sampling Units (PSUs) based on residence (urban/rural); followed by systematic sampling from the PSUs. The details are presented elsewhere [20].
Participants
Women aged 15–49 years were interviewed and basic anthropometric measures were obtained from children under-five years of age.
Variables
The variables consistently reported across the three rounds were selected. These included diarrhoea, acute respiratory illness (ARI), stunting, wasting, severe wasting, underweight, overweight and anaemia impacting children under-five years. Refer to Table 1 for case definitions.
Statistical analysis
Data from NFHS were extracted in MS Excel and analysed in Stata v.16 [21]. Analysis was done between January-February 2021. The prevalence of the studied outcomes over rounds was extracted and their overall mean prevalence with the 95% confidence interval of all states was computed. Further, the relative change (RC) from NFHS-3 to NFHS-5 of the mean values was computed using the nlcom rel_delta command in Stata. Level of significance was set at 0.05. RC for individual states was also calculated and plotted on Microsoft Excel Bing Maps. The average annual rate of reduction (AARR) considering NFHS 3, 4 and 5 was calculated using the formula [22]:
where β is the linear regression coefficient of ln(prevalence) against time(years).
NFHS-5 data were also checked for the disparity in the distribution of the outcome prevalence by place of residence by plotting the percentage point difference.
Results
We draw our findings from 1,88,272 women respondents across the three NFHS rounds against eight indicators in the selected NE states. The findings present the trend in changing prevalence, relative change, average annual rate of reduction and distribution of disease burden by place of residence.
Trends in the prevalence of included childhood health outcomes
The prevalence of outcome indicators across all rounds is described in Table 2. Broadly, the prevalence of ARI, diarrhoea, stunting and underweight reduced over the last 15 years whereas overweight prevalence steadily increased. The largest reduction was observed in ARI from 6.2% to 1.2% between 2006 and 2020, followed by underweight from 31.1% to 20.7%. Moreover, the proportion of anaemia, wasting and severe wasting, although reduced between 2006–2016, increased from 2016 (S3). It is noteworthy that the levels of anaemia in 2020 for the majority of NE states worsened and regressed to the 2006-prevalence.
At the state level, Assam and Sikkim reported a reduction in diarrhoeal and ARI cases till 2016, followed by an increase in 2020. Similarly, the prevalence of stunting, wasting and underweight worsened from 2016 in Nagaland and Tripura. In the latest round, Meghalaya had the highest proportion of diarrhoea, ARI and stunting whilst Assam had the highest prevalence of wasting, severely wasting, underweight and anaemia compared to other NE states (S4).
Relative change
A statistically significant reduction in the mean prevalence of diarrhoea, ARI, stunting and underweight was observed in NFHS-5 relative to NFHS-3; however, ARI showed the largest improvement by 70% (RC: −0.7 [95% CI:−0.1,−0.4]). Additionally, the overweight prevalence worsened by 10-times in 2020 relative to 2006. This analysis showed insufficient evidence of a reduction in anaemia and wasting prevalence. Table 3 illustrates the relative change (ratio) of the mean of health indicators.
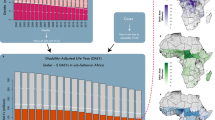
In state-specific changes, Assam, Manipur, Mizoram and Sikkim showed a reduction in the prevalence of diarrhoea up to 70%, ARI up to 90%, stunting and underweight up to 40% between 2006 and 2020. Nevertheless, they reported an increase in the prevalence of wasting and severe wasting. Tripura was the only state that observed a relative reduction in all outcomes from 2006, except overweight and anaemia. State-specific relative changes (ratios) are presented in Fig. 1.
Average annual rate of reduction
Diarrhoea and ARI collectively witnessed the highest overall annualised rate of reduction of all studied indicators from 2006 to 2020, followed by underweight.
While Sikkim had the poorest yearly reduction rates for ARI among all NE states, Tripura had the highest. Further, Meghalaya saw the lowest AARR for diarrhoea, whereas Sikkim showed the greatest progress. Within nutritional disorders, underweight and stunting showed modest annualised reduction rates across all states. Moreover, only Meghalaya showed the highest annual progress for wasting and severe wasting, whereas the remaining states observed slight to no change. Likewise, anaemia showed marginal changes over the years. Overweight witnessed the slowest AARR due to an exponential increase of the prevalence largely contributed by Tripura (Table 4).
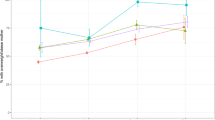
Prevalence distribution by place of residence
Overall, rural areas had a higher prevalence of all undernutrition indicators and anaemia than urban areas of residence in 2020. However, overweight was almost equally prevalent in both. Diarrhoea was modestly more prevalent in rural areas, while ARI was seen more in urban settings (Fig. 2). Rural households of Sikkim, Tripura and Assam experienced a higher burden of the studied indicators indicating a greater inequity in these states.
Distribution of the burden of health outcomes by place of residence. The point difference of prevalence (urban and rural) for diarrhoea, ARI, stunting, wasting, severe wasting, underweight, overweight and anaemia are presented for the states (A) Assam, B Manipur, C Meghalaya, D Mizoram, E Nagaland, F Sikkim, G Tripura.
Discussion
The findings are discussed by outcomes concerning their change from 2006, annual reduction rates, disparities in burden, and progress towards achieving their reduction targets.
Overall, for the NE states, a substantial reduction in ARIs with modest improvements in diarrhoea was seen between 2019 and 2020 compared to 2005 and 2006 and was supported with high AARRs. A similar trend is seen in India [15]; however, the mean NE prevalence is less than the Indian average. The reductions can be attributed to better coverage of safe drinking water, sanitation, clean cooking fuel, and distribution of Zinc tablets and ORS [15]. Conversely, the relatively slower ARI and diarrhoeal change observed in Meghalaya within the NE cluster could be due to a lack of clean cooking fuel, use of open fire for cooking, and faulty/ineffective drinking water treatment, as reported in NFHS-5. Notably, the data collection periods across the rounds are not consistent and could suggest seasonal prevalence. It is likely NFHS-5 overestimated diarrhoeal prevalence in most of the NE states as the data was collected in monsoon (July–Nov).
We note an overall slow, yet positive shift in underweight and stunting in NE states, although it is not met with expected reductions in wasting. We found insufficient evidence to suggest any reduction in the wasting prevalence. The AARRs corroborate with the observed changes across rounds; however, these rates, along with limited prevalence reductions from 2016, are insufficient to achieve the National Nutrition Mission’s (NNM) 2022 and WHO/UNICEF’s 2030 undernutrition targets [23,24,25]. The NFHS-5 estimates of stunting, underweight and wasting are broadly in line with another study [12]. Further, the average Indian estimates shares a similar trend with the NE. Bringing a simultaneous reduction in stunting and wasting has always been challenging [26]. We believe the observed reductions in underweight and stunting could broadly be an outcome of an overall improvement in the socioeconomic status and sanitation facilities in the last 15 years. Notably, between 2016 and 2020 a stagnancy in stunting and underweight rates were observed with a moderate increase in wasting. This trend could have resulted from an economic slowdown in India from 2016 [27] that pushed many vulnerable families into poverty, and experience acute food shortages; causing a rise in food insecurity [28]. Therefore, to achieve any further reductions in undernutrition it is pivotal to ensure food security and adequate dietary practices among children, which are presently lacking [15].
The inter-and intra-state variations of the nutritional indicators in NE states also reflect their socioeconomic differences. A past study reported coexistence of multiple nutritional disorders in children from the lower wealth strata in NE states and India [29]. We note a higher burden of stunting in rural Meghalaya and Sikkim, and severe/wasting in rural Tripura and urban Nagaland. Manipur had one of the lowest prevalence of malnutrition indicators in NE states and this could be attributed to the better socioeconomic status of the population [30]. Conversely, high stunting in Meghalaya—primarily driven by Khasi Hill tribes—can be linked with high food insecurity, low income, and over-reliance on commercial agricultural products and food provided through Public Distribution System [15, 31]. This is supported by a study of the Chakhesang tribe in Nagaland which attributed their lower undernutrition prevalence to greater consumption of indigenous food [32]. Similarly, Assam performed poorly in wasting, wherein the tea-estate districts performed worse. This could be broadly associated with frequent political strikes (bandhs) that obstruct agricultural products inflow, poor maternal health and wealth-quintile in Assam. This is further compounded in regions of tea-estates where women accompanied by children, experience poor sanitation facilities; lack dietary diversity and appropriate complementary feeding; and have maternal anaemia, resulting in low birthweight and successive wasting [15, 33].
Timely identification and case-management of undernutrition indicators are critical as their cyclical and complex nature make them interdependent [34]. However, these could be challenging in the NE due to inaccessibility owing to difficult terrain; high tribal density; health-service interruption caused by political tension [35]; and low technical competency of the healthworkers on anthropometric measuring and counselling [36]. To overcome malnutrition and improve child health, several preventive and curative programmes have been launched by the Indian government [13, 14, 37] in line with the Lives Saved Tool (LiST) [38]. Given the contextual background of the NE cluster, these states require a tailored approach to witness improvements. Robust monitoring and evaluation of service coverage indicators directly related to malnutrition tracking, identification and management is needed.
We found a progressive rise in overweight which is consistent with trends in India [12] and other low-and middle-income countries (LMIC) [39]. However, the NE states witnessed a larger shift than the Indian average between 2006 and 2020. The AARR trends strongly indicate a failure to achieve the 3% international target by 2030 [24]. However, due to their relatively low prevalence, now is an opportune time to introduce prevention strategies among young children. Failing this can lead to an uncontrolled increase across all wealth strata and settlements soon. We suggest equipping community healthworkers in identifying and counselling overnutrition cases in addition to undernutrition. Past literature, including a study on the Meitei tribe of Manipur, have found associations of childhood overweight with consumption of energy-dense or sugary food, sedentary lifestyle [40], lack of dietary diversity, maternal overweight, smoking, no breastfeeding and rapid urbanisation [30, 41].
A dramatic rise in childhood anaemia was observed in a majority of the NFHS-5 Phase-1 states/union territories from 2016, wherein five of the seven included NE states reported the highest increase. This trend, while could be an outcome of the rising inequities discussed previously, has led to a limited change in its prevalence from 2006 in NE. Except for Meghalaya, all states had poor AARRs and are far from achieving the NNM’s 3%-point annual reduction. Reducing anaemia for almost all age groups in India has been difficult yet the exceedingly high prevalence observed in NE states is worrying and calls for urgent action. The rising anaemia can be associated with an increased percentage of maternal anaemia, poor childhood consumption of iron-rich food, iron-supplements, deworming medicines and dietary diversity [15], and soil-helminth infections [42] in NE which are its known risk-factors [43,44,45]. Additionally, anaemia has also been linked with malaria [46], parasitic and worm infections, indoor pollution and home environment [47], however, it warrants more research in NE. To combat anaemia, India launched an umbrella programme called ‘Anaemia Mukht Bharat’ in 2018 which intends to reduce childhood anaemia to 40% by 2022 [48]; nevertheless, recent HMIS reports of the NE states suggest extremely poor coverage of its interventions [49].
One of the key contributions of this study is to bring policymakers attention to the growing need of analysing disease burden trends for various population groups and tailor programmes accordingly. The current programming approach rarely recognises such inequities, and may not be sufficient to improve the overall health of children, especially in the Northeast. As evidenced from our findings, a rise in prevalence of some indicators between 2016 and 2020 has impeded them from achieving effective AARRs and slowed progress [23]. High concentrations of marginalised populations and diverse social cultures in NE are complicated by difficult access to mainstream resources. This necessitates policies and programmes to make adaptability a fundamental element. Reporting childhood malnutrition data by socioeconomic groups in the national and state reports may assist in more granular programmatic decision-making for different communities. Further, developing India-specific overweight reduction targets can control its rise. Moreover, educating lower socioeconomic communities on proximal causal factors of child health could aid in reducing the equity-gap.
This study has some limitations. A large variation in the sample sizes of Assam and Meghalaya in NFHS-4 and NFHS-5 were noted which should be considered before interpreting their prevalence. It is also important to understand the linkages between childhood overweight/obesity and the concurrent occurrence of stunting and anaemia in these states [50]. We do not extensively compare our findings with NFHS-5 Phase-2 states as their data was collected after the onset of the COVID-19 pandemic, thereby making the two phases incomparable.
Conclusion
We note a high burden of the studied childhood health outcomes in the NE states, contributed by stagnant or worsening undernutrition and moderate levels of diarrhoea. A rapid rise in overweight and reversal of gains in anaemia since 2016 further complicate the inferences. While the trends in NE is similar to other parts of India, some of these states require special attention owing to the contextual challenges. A greater predisposition of these outcomes is noted among some tribal and marginalised populations. Evidently, past programmes have had limited impact on reduction, hence it is recommended that policymakers focus on improving the coverage, quality, accountability and acceptance of the existing programmes before launching new programmes. Periodic evaluations of active programmes are required to assess programme fitness and success specifically for vulnerable communities. Moreover, tribal populations should be encouraged to consume indigenous food to prevent food insecurity rather than commercial products; however, there is a need to assess the nutritional value of these in NE. Further epidemiological studies on the health outcomes and their causal factors, categorised by socioeconomic groups, using a gender-disaggregated approach are needed in NE. The impact of childhood endemic and parasitic diseases on child health in NE is required. The prevalence of the studied indicators is expected to worsen in the next round due to a rise in food insecurity and health-service interruption due to the COVID-19 pandemic.
Data availability
The data supporting the findings of this study are publicly available from NFHS at http://rchiips.org/nfhs/index.shtml; NFHS-3 and NFHS-4 data were obtained from the state reports and NFHS-5 was obtained from the state factsheets.
References
UNICEF, World Health Organization, World Bank. Levels and Trends in Child malnutrition. Key findings of the 2018 edition. 2018.
UNICEF. One is too many- Ending child deaths from pneumonia and Diarrhoea. 2016. Available from: https://data.unicef.org/wp-content/uploads/2016/11/UNICEF-Pneumonia-Diarrhoea-report2016-web-version_final.pdf
UNICEF. Children, food and nutrition-Growing well in a changing world. 2019.
Dandona R, Anil Kumar G, Henry NJ, Joshua V, Ramji S, Gupta SS, et al. Subnational mapping of under-5 and neonatal mortality trends in India: the Global Burden of Disease Study 2000-17. Lancet 2020;395:1640–58.
World Health Organization. Children: improving survival and well-being. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality
UNICEF. WHO. World Bank: UN DESA. Levels & Trends in Child Mortality 2019. UN IGME Rep. 2019;52.
2020 Global Nutrition Report—Global Nutrition Report. 2020. Available from: https://globalnutritionreport.org/reports/2020-global-nutrition-report/
World Health Organisation. Ending preventable deaths from pneumonia and diarrhoea by 2025. 2013. Available from: https://www.who.int/news/item/10-04-2013-ending-preventable-deaths-from-pneumonia-and-diarrhoea-by-2025
Sachs J, Schmidt-Traub, Kroll G, Fuller G The Sustainable Development Goals and COVID-19. Sustainable Development Report 2020. 2020. Available from: www.pica-publishing.com
Global Hunger Index Scores by 2021 GHI Rank - Global Hunger Index (GHI). 2021. Available from: https://www.globalhungerindex.org/ranking.html
Liu L, Chu Y, Oza S, Hogan D, Perin J, Bassani DG, et al. National, regional, and state-level all-cause and cause-specific under-5 mortality in India in 2000–15: a systematic analysis with implications for the Sustainable Development Goals. Lancet Glob Heal. 2019;7:e721–34.
Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF, Population Council. Comprehensive National Nutrition Survey (CNNS) National Report 2016-2018. New Delhi; 2109.
Press Information Bureau., Government of India., Ministry of Health and Family Welfare. Nutritional Rehabilitation Centres. 2018. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=186712
National food security Portal. Dept. of food and public distribution. Governement of India. National Food Security Act, (NFSA) 2013. 2013. Available from: https://nfsa.gov.in/portal/NFSA-Act
International Institute for Population Sciences. National Family Health Survey. Mumbai; Available from: http://rchiips.org/nfhs/
Office of the Registrar General & Census Commissioner. India. Census 2011 India. 2011. Available from: https://www.census2011.co.in/
Reserve Bank of India. Handbook of Statistics on Indian States. 2021. Available from: https://m.rbi.org.in/scripts/AnnualPublications.aspx?head=Handbook of Statistics on Indian States
Das TK, Das Gupta I, Haldar SK, Mitra S Conflicts and Socioeconomic Consequences in Northeast India. Asian Journal of Humanities and Social Studies. 2015. Available from: https://www.researchgate.net/publication/279200696
Singh KD, Alagarajan M, Ladusingh L. What explains child malnutrition of indigenous people of Northeast India? PLoS ONE. 2015;10:e0130567.
National Family Health Survey 2019-20: DATA QUALITY ASSURANCE AND QUALITY CONTROL MECHANISMS. 2021.
StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019.
Statistics and Monitoring Section. Division of Policy and Practice. UNICEF. Technical Note: How to calculate average annual rate of reduction (AARR) of underweight prevalence—UNICEF DATA. 2007. Available from: https://data.unicef.org/resources/technical-note-calculate-average-annual-rate-reduction-aarr-underweight-prevalence/
Swaminathan S, Hemalatha R, Pandey A, Kassebaum NJ, Laxmaiah A, Longvah T, et al. The burden of child and maternal malnutrition and trends in its indicators in the states of India: the Global Burden of Disease Study 1990–2017. Lancet Child Adolesc Heal. 2019;3:855–70.
WHO/UNICEF. WHO/UNICEF discussion paper: The extension of the 2025 maternal, infant and young child nutrition targets to 2030—UNICEF DATA. 2019. Available from: https://data.unicef.org/resources/who-unicef-discussion-paper-nutrition-targets/
Press Information Bureau, Government of India., Ministry of Women and Child Development. PM launches National Nutrition Mission, and pan India expansion of Beti Bachao Beti Padhao, at Jhunjhunu in Rajasthan. 2018. Available from: https://pib.gov.in/newsite/PrintRelease.aspx?relid=177166
Emergency Nutrition Network. Undersized Indian children: nutrients-starved or hungry for development. Field Exchange 59. Emergency Nutrition Network (ENN); 2019. p. 41. Available from: www.ennonline.net/fex/59/undersizedindianchildren. Accessed Feb 2021
Drèze J, Gupta A, Parashar SA, Sharma K. Pauses and Reversals of Infant Mortality Decline in India in 2017 and 2018. SSRN Electronic Journal. 2020. Available from: https://www.ssrn.com/abstract=3727001. Accessed Feb 2022
FAO UN, WFP, WHO, UNICEF, IFAD. Transforming Food Systems for Affordable Healthy Diets. The State of Food Security and Nutrition in the World 2020. 2020.
Jith JR, Bedamatta R. Child undernutrition in the states of india: an analysis based on change in composite index of anthropometric failure from 2006 to 2016. Rev Dev Chang. 2021;26:104–26.
Loukrakpam B, Rajendran A, Madhari RS, Boiroju NK, Longvah T. Dietary adequacy and nutritional status of Meitei community of Manipur, Northeast India. Matern Child Nutr. 2020;16(S3):1–12.
Chyne DAL, Meshram II, Rajendran A, Kodali V, Getti N, Roy P, et al. Nutritional status, food insecurity, and biodiversity among the Khasi in Meghalaya, North-East India. Matern Child Nutr. 2017;13:e12557.
Longvah T, Khutsoh B, Meshram II, Krishna S, Kodali V, Roy P, et al. Mother and child nutrition among the Chakhesang tribe in the state of Nagaland, North-East India. Matern Child Nutr. 2017;13:1–12.
Rajbangshi PR, Nambiar D. “who will stand up for us?” the social determinants of health of women tea plantation workers in India. Int J Equity Health. 2020;19:1–10.
Myatt M, Khara T, Schoenbuchner S, Pietzsch S, Dolan C, Lelijveld N, et al. Children who are both wasted and stunted are also underweight and have a high risk of death: a descriptive epidemiology of multiple anthropometric deficits using data from 51 countries. Arch Public Heal. 2018;76:28.
Ganesan L, Kashyap A. Problems and prospects of implementing ICDS in the States of Tamil Nadu and Assam. Shanlax. Int J Econ. 2016;4:53–63.
Barua K, Baruah R. Application of growth monitoring charts by health care providers in Village Health and Nutrition Day (VHND) setting in rural Kamrup. Indian J Community Heal. 2015;26:322–6.
Ministry of Health and Family Welfare. Ministry of Health and Family Welfare Government of India Programme for Promotion of Breastfeeding. 2016. Available from: https://nhm.gov.in/MAA/Operational_Guidelines.pdf
Stegmuller AR, Self A, Litvin K, Roberton T. How is the Lives Saved Tool (LiST) used in the global health community? Results of a mixed-methods LiST user study. BMC Public Health 2017;17(Suppl 4):773.
UNICEF, World Health Organization, World Bank. Levels and trends in child malnutrition. 2018.
Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev. 2010;11:695–708.
Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child. 2012;97:1019–26.
Salam N, Azam S. Prevalence and distribution of soil-transmitted helminth infections in India. BMC Public Health. 2017;17:201.
Pasricha SR, Black J, Muthayya S, Shet A, Bhat V, Nagaraj S, et al. Determinants of anemia among young children in rural India. Pediatrics 2010;126:140.
Ngui R, Lim YAL, Chong Kin L, Sek Chuen C, Jaffar S. Association between anaemia, iron deficiency anaemia, neglected parasitic infections and socioeconomic factors in rural children of West Malaysia. de Silva N, editor. PLoS Negl Trop Dis. 2012;6:e1550.
Molla E, Mamo H. Soil-transmitted helminth infections, anemia and undernutrition among schoolchildren in Yirgacheffee, South Ethiopia. BMC Res Notes. 2018;11:585.
Douglas NM, Lampah DA, Kenangalem E, Simpson JA, Poespoprodjo JR, Sugiarto P, et al. Major Burden of Severe Anemia from Non-Falciparum Malaria Species in Southern Papua: A Hospital-Based Surveillance Study. Hviid L, editor. PLoS Med. 2013;10:e1001575.
Baranwal A, Baranwal A, Roy N. Association of household environment and prevalence of anemia among children under-5 in India. Front Public Heal. 2014;2:196.
Adolescent Division. Ministry of Health and Family Welfare. Government of India. Guidelines for Control of Iron Deficiency Anaemia. 2018. Available from: http://nhm.gov.in/images/pdf/programmes/wifs/guidelines/Guidelines_for_Control_of_Iron_Deficiency_Anaemia.pdf
Poshan Abhiyan. National Health Mission. An introduction to Anemia Mukt Bharat. 2019. Available from: https://anemiamuktbharat.info/wp-content/uploads/2019/09/INFO-sheet-3-About-Anemia-Mukt-Bharat.pdf
Susan K, Guy P, Grace E, Bart van den B. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr Bull. 2014;35:167–78.
Acknowledgements
The authors thank NFHS for their data. The authors also appreciate the support of Solomon Salve from Oxford Policy Management for reviewing the manuscript. No funding was sought for this study.
Author information
Authors and Affiliations
Contributions
A.M. was responsible for conceiving and designing the study. She drafted the manuscript, extracted the data, conducted the analyses, and wrote the Results and Discussion sections. She coordinated with co-authors and integrated the feedback, and revised the manuscript. R.R. was responsible for rechecking the data analyses and writing the initial Introduction. She also reviewed the complete manuscript. R.P. was responsible for conceiving and designing the study. He reviewed the draft, provided feedback and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mukherjee, A., Rizu & Parashar, R. Longitudinal trends in the health outcomes among children of the North Eastern States of India: a comparative analysis using national DHS data from 2006 to 2020. Eur J Clin Nutr 76, 1528–1535 (2022). https://doi.org/10.1038/s41430-022-01147-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01147-w