Abstract
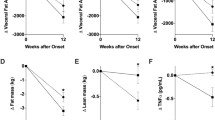
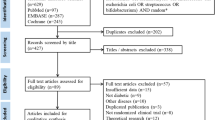
Probiotics are shown to alter the microbiota, leading to a favorable environment, in which weight loss and metabolic parameters are improve. However, the results on probiotics’ effect on specific types of central adipose tissues, mainly visceral (VAT) and subcutaneous adipose tissue (SAT), are conflicting. Therefore, we conducted a systematic review, aimed to evaluate the effects of probiotics on VAT and SAT. PubMed, SCOPUS, EBSCO, and LILACS databases were searched for studies that investigated the effect of probiotics on VAT and SAT. Fixed effects were used to calculate the pooled difference in means (DM) and 95% confidence intervals (95%CI). Fourteen publications met the inclusion criteria, which consisted of 1523 participants. For VAT, overall, there was a significant decrease (DM = −3.63 cm2, 95% CI: −5.08 to −2.17, p < 0.001). When stratified by type of probiotic, single Bifidobacterium (DM = −4.49 cm2, 95% CI:−7.37 to −1.61, p = 0.002) and single Lactobacillus probiotics (DM = −3.84 cm2, 95% CI:−5.74 to −1.93, p < 0.001) resulted in significant reductions. Mixed probiotics had no effect. For SAT, overall, there was a significant decrease (DM = −2.91 cm2, 95% CI:−4.82 to −1.01, p = 0.003), and when stratified by type of probiotic, single Lactobacillus (DM = −3.39 cm2, 95% CI:−5.90 to −0.88, p = 0.008) and mixed probiotics (DM = −5.97 cm2, 95% CI:−10.32 to −1.62, p = 0.007) resulted in a significant decrease. Single Bifidobacterium probiotics had no effect. Using meta-regression, no association was observed between the total daily probiotic dose and VAT or SAT reduction. This study shows that probiotics have a beneficial effect on central adiposity. Single Lactobacillus-based probiotics reduced VAT and SAT, whereas Bifidobacterium-based probiotics reduce VAT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplement information files.
References
Romieu I, Dossus L, Barquera S, Blottière HM, Franks PW, Gunter M, et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control. 2017;28:247–58. https://doi.org/10.1007/s10552-017-0869-z
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10:207–15. https://doi.org/10.1159/000471488
Abraham TM, Pedley A, Massaro JM, Hoffmann U, Fox CS. Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Circulation. 2015;132:1639–47. https://doi.org/10.1161/circulationaha.114.015000
Burhans MS, Hagman DK, Kuzma JN, Schmidt KA, Kratz M. Contribution of adipose tissue inflammation to the development of Type 2 Diabetes Mellitus. Compr Physiol. 2018;9:1–58. https://doi.org/10.1002/cphy.c170040
Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11:11–8. https://doi.org/10.1111/j.1467-789X.2009.00623.x
Markowiak P, Śliżewska K. Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. 2017;9:1021. https://doi.org/10.3390/nu9091021
Vissers D, Hens W, Hansen D, Taeymans J. The effect of diet or exercise on visceral adipose tissue in overweight youth. Med Sci Sports Exerc. 2016;48:1415–24. https://doi.org/10.1249/mss.0000000000000888
Liu FX, Flatt SW, Nichols JF, Pakiz B, Barkai HS, Wing DR, et al. Factors associated with visceral fat loss in response to a multifaceted weight loss intervention. J Obes Weight Loss Ther. 2017;7:346. https://doi.org/10.4172/2165-7904.1000346
Ruan Y, Sun J, He J, Chen F, Chen R, Chen H. Effect of probiotics on glycemic control: a systematic review and meta-analysis of randomized, controlled trials. PLoS One. 2015;10:e0132121. https://doi.org/10.1371/journal.pone.0132121
Kim YA, Keogh JB, Clifton PM. Probiotics, prebiotics, synbiotics and insulin sensitivity. Nutr Res Rev. 2018;31:35–51. https://doi.org/10.1017/s095442241700018x
Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, et al. Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr. 2010;64:636–43. https://doi.org/10.1038/ejcn.2010.19
Kim J, Yun JM, Kim MK, Kwon O, Cho B. Lactobacillus gasseri BNR17 supplementation reduces the visceral fat accumulation and waist circumference in obese adults: a randomized, double-blind, placebo-controlled trial. J Med Food. 2018;21:454–61. https://doi.org/10.1089/jmf.2017.3937
Angelakis E, Armougom F, Million M, Raoult D. The relationship between gut microbiota and weight gain in humans. Future Microbiol. 2012;7:91–109. https://doi.org/10.2217/fmb.11.142
Maurovich-Horvat P, Massaro J, Fox CS, Moselewski F, O’Donnell CJ, Hoffmann U. Comparison of anthropometric, area- and volume-based assessment of abdominal subcutaneous and visceral adipose tissue volumes using multi-detector computed tomography. Int J Obes. 2007;31:500–6. https://doi.org/10.1038/sj.ijo.0803454
Bertin E, Marcus C, Ruiz JC, Eschard JP, Leutenegger M. Measurement of visceral adipose tissue by DXA combined with anthropometry in obese humans. Int J Obes Relat Metab Disord. 2000;24:263–70. https://doi.org/10.1038/sj.ijo.0801121
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. https://doi.org/10.1007/s10654-010-9491-z
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 2011 [updated March 2011; cited 2021 Feb 27]. Available from: https://handbook-5-1.cochrane.org/
Miller JJ. The inverse of the Freeman–Tukey double arcsine transformation. Am Stat. 1978;32:138. https://doi.org/10.1080/00031305.1978.10479283
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. https://doi.org/10.1136/bmj.315.7109.629
Artene DV, Bordea CI, Blidaru A. Results of 1-year diet and exercise interventions for ER+/PR±/HER2- breast cancer patients correlated with treatment type. Chirurgia. 2017;112:457–68. https://doi.org/10.21614/chirurgia.112.4.457
Canfora EE, van der Beek CM, Hermes GDA, Goossens GH, Jocken JWE, Holst JJ, et al. Supplementation of diet with galacto-oligosaccharides increases Bifidobacteria, but not insulin sensitivity, in obese prediabetic individuals. Gastroenterology. 2017;153:87–97. https://doi.org/10.1053/j.gastro.2017.03.051
Matsuoka R, Kamachi K, Usuda M, Wang W, Masuda Y, Kunou M, et al. Lactic-fermented egg white improves visceral fat obesity in Japanese subjects-double-blind, placebo-controlled study. Lipids Health Dis. 2017;16:237. https://doi.org/10.1186/s12944-017-0631-2
Pan R, Xu T, Bai J, Xia S, Liu Q, Li J, et al. Effect of Lactobacillus plantarum fermented barley on plasma glycolipids and insulin sensitivity in subjects with metabolic syndrome. J Food Biochem. 2020;44:e13471. https://doi.org/10.1111/jfbc.13471
Artene DV, Bordea CI, Blidaru A. A moderately high protein diet is as effective during neoadjuvant chemotherapy as it is 2 years after breast cancer surgery–A pilot trial. Rom Med Rev. 2017;64:133–7.
Nomura N, Nishimura A, Miyoshi T, Kitazono E, Monta H, Matsui T. Anti-obesity effect of functional barley BARLEYmax (Tantangara) through gut microbiota: a double-blind, randomized, placebo-controlled, parallel-group comparison clinical trial. Jpn. Pharm Ther. 2018;46:2099–110. https://doi.org/10.1016/j.jcs.2020.102959
Leyrolle Q, Cserjesi R, DGHM M, Zamariola G, Hiel S, Gianfrancesco MA, et al. Prebiotic effect on mood in obese patients is determined by the initial gut microbiota composition: a randomized, controlled trial. Brain Behav Immun. 2021;94:289–98. https://doi.org/10.1016/j.bbi.2021.01.014
Mobini R, Tremaroli V, Ståhlman M, Karlsson F, Levin M, Ljungberg M, et al. Metabolic effects of Lactobacillus reuteri DSM 17938 in people with type 2 diabetes: a randomized controlled trial. Diabetes Obes Metab. 2017;19:579–89. https://doi.org/10.1111/dom.12861
Nakamura F, Ishida Y, Aihara K, Sawada D, Ashida N, Sugawara T, et al. Effect of fragmented Lactobacillus amylovorus CP1563 on lipid metabolism in overweight and mildly obese individuals: a randomized controlled trial. Micro Ecol Health Dis. 2016;27:30312. https://doi.org/10.3402/mehd.v27.30312
Pedret A, Valls RM, Calderón-Pérez L, Llauradó E, Companys J, Pla-Pagà L, et al. Effects of daily consumption of the probiotic Bifidobacterium animalis subsp. lactis CECT 8145 on anthropometric adiposity biomarkers in abdominally obese subjects: a randomized controlled trial. Int J Obes. 2019;43:1863–8. https://doi.org/10.1038/s41366-018-0220-0
Agerholm-Larsen L, Raben A, Haulrik N, Hansen AS, Manders M, Astrup A. Effect of 8 week intake of probiotic milk products on risk factors for cardiovascular diseases. Eur J Clin Nutr. 2000;54:288–97. https://doi.org/10.1038/sj.ejcn.1600937
Gomes AC, Hoffmann C, Mota JF. Gut microbiota is associated with adiposity markers and probiotics may impact specific genera. Eur J Nutr 2020;59:1751–62. https://doi.org/10.1007/s00394-019-02034-0
Ida M, Maekawa T, Izumo T, Shibata H, Fujisawa K. Reduction of abdominal fat mass by long-term intake of lactobacillus pentosus strain S-PT84 and safety assessment–A randomized, double-blind, placebo-controlled, parallel-group study. Jpn Pharm Ther. 2018;46:897–910.
Maekawa T, Izumo T, Ida M, Kitagawa Y, Shibata H, Fukuhara D. Reduction of abdominal visceral fat mass by long-term intake of Lactobacillus pentosus strain S-PT84 and its safety assessment in pilot study-A randomized, double-blind, placebo-controlled, parallel-group study. Jpn Pharm Ther. 2018;46:97–109.
Nakanishi N, Fusako Y, Notula Y, Ochitanic D, Oki M. Effect of long-term intake on abdominal body fat reduction by Lactobacillus plantarum PIONBN22 and Fructo-oligosaccharides in an investigation of a clinical triala randomized, double-blind, placebo-controlled, parallel group study. Jpn Pharm Ther. 2020;48:267–81.
Takano Y, Kobayashi T, Kawasaki Y, Akai Y, Ikuyama K, Tsuchida T. Visceral fat-reducing effect of fermented milk containing the probiotic Lactobacillus gasseri SBT2055. Jpn Pharm Ther. 2013;41:895–903.
Ruscica M, Pavanello C, Gandini S, Macchi C, Botta M, Dall’Orto D, et al. Nutraceutical approach for the management of cardiovascular risk - a combination containing the probiotic Bifidobacterium longum BB536 and red yeast rice extract: results from a randomized, double-blind, placebo-controlled study. Nutr J. 2019;18:13. https://doi.org/10.1186/s12937-019-0438-2
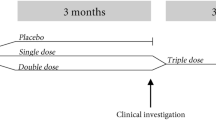
Szulińska M, Łoniewski I, van Hemert S, Sobieska M, Bogdański P. Dose-dependent effects of multispecies probiotic supplementation on the Lipopolysaccharide (LPS) level and cardiometabolic profile in obese postmenopausal women: a 12-week randomized clinical trial. Nutrients. 2018;10:773. https://doi.org/10.3390/nu10060773
Banach K, Glibowski P, Jedut P. The effect of probiotic yogurt containing Lactobacillus acidophilus LA-5 and Bifidobacterium lactis BB-12 on selected anthropometric parameters in obese individuals on an energy-restricted diet: a randomized, controlled trial. Appl Sci. 2020;10:5830. https://doi.org/10.3390/app10175830
Jones RB, Alderete TL, Martin AA, Geary BA, Hwang DH, Palmer SL, et al. Probiotic supplementation increases obesity with no detectable effects on liver fat or gut microbiota in obese Hispanic adolescents: a 16-week, randomized, placebo-controlled trial. Pediatr Obes. 2018;13:705–14. https://doi.org/10.1111/ijpo.12273
Smith-Ryan AE, Mock MG, Trexler ET, Hirsch KR, Blue MNM. Influence of a multistrain probiotic on body composition and mood in female occupational shift workers. Appl Physiol Nutr Metab. 2019;44:765–73. https://doi.org/10.1139/apnm-2018-0645
Vajro P, Mandato C, Licenziati MR, Franzese A, Vitale DF, Lenta S, et al. Effects of Lactobacillus rhamnosus strain GG in pediatric obesity-related liver disease. J Pediatr Gastroenterol Nutr. 2011;52:740–3. https://doi.org/10.1097/MPG.0b013e31821f9b85
Kim M, Kim M, Kang M, Yoo HJ, Kim MS, Ahn YT, et al. Effects of weight loss using supplementation with Lactobacillus strains on body fat and medium-chain acylcarnitines in overweight individuals. Food Funct. 2017;8:250–61. https://doi.org/10.1039/c6fo00993j
Fujiwara S, Shioya N, Sugawara T, Ishida Y, Sawada D, Aoki Y, et al. Regulation of adiposity by para-metabobiotic lactobacillus amylovorus CP1563 in healthy normal and pre-obese adult individuals-a randomized controlled trial. Jpn. Pharm Ther. 2018;46:1601–12.
Kadooka Y, Sato M, Ogawa A, Miyoshi M, Uenishi H, Ogawa H, et al. Effect of Lactobacillus gasseri SBT2055 in fermented milk on abdominal adiposity in adults in a randomised controlled trial. Br J Nutr. 2013;110:1696–703. https://doi.org/10.1017/s0007114513001037
Minami J, Iwabuchi N, Tanaka M, Yamauchi K, Xiao JZ, Abe F, et al. Effects of Bifidobacterium breve B-3 on body fat reductions in pre-obese adults: a randomized, double-blind, placebo-controlled trial. Biosci Microbiota Food Health. 2018;37:67–75. https://doi.org/10.12938/bmfh.18-001
Sugawara T, Sawada D, Yanagihara S, Aoki Y, Takehara I, Sugahara H, et al. Daily intake of paraprobiotic Lactobacillus amylovorus CP1563 improves pre-obese conditions and affects the gut microbial community in healthy pre-obese subjects: a double-blind, randomized, placebo-controlled study. Microorganisms. 2020;8:304. https://doi.org/10.3390/microorganisms8020304
Takahashi S, Anzawa D, Takami K, Ishizuka A, Mawatari T, Kamikado K, et al. Effect of Bifidobacterium animalis ssp. lactis GCL2505 on visceral fat accumulation in healthy Japanese adults: a randomized controlled trial. Biosci Microbiota Food Health. 2016;35:163–71. https://doi.org/10.12938/bmfh.2016-002
Toshimitsu T, Gotou A, Sashihara T, Furuichi K, Hachimura S, Shioya N. et al.Ingesting yogurt containing Lactobacillus plantarum OLL2712 reduces abdominal fat accumulation and chronic inflammation in overweight adults in a randomized placebo-controlled trial.Curr Dev Nutr. 2021;5:nzab006 :https://doi.org/10.1093/cdn/nzab006
Ahn SB, Jun DW, Kang BK, Lim JH, Lim S, Chung MJ. Randomized, double-blind, placebo-controlled study of a multispecies probiotic mixture in nonalcoholic fatty liver disease. Sci Rep. 2019;9:5688. https://doi.org/10.1038/s41598-019-42059-3
Song EJ, Han K, Lim TJ, Lim S, Chung MJ, Nam MH, et al. Effect of probiotics on obesity-related markers per enterotype: a double-blind, placebo-controlled, randomized clinical trial. EPMA J 2020;11:31–51. https://doi.org/10.1007/s13167-020-00198-y
Jung SP, Lee KM, Kang JH, Yun SI, Park HO, Moon Y, et al. Effect of Lactobacillus gasseri BNR17 on overweight and obese adults: a randomized, double-blind clinical trial. Korean J Fam Med. 2013;34:80–9. https://doi.org/10.4082/kjfm.2013.34.2.80
Jung S, Lee YJ, Kim M, Kim M, Kwak JH, Lee J-W, et al. Supplementation with two probiotic strains, Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032, reduced body adiposity and Lp-PLA2 activity in overweight subjects. J Funct Foods. 2015;19:744–52. https://doi.org/10.1016/j.jff.2015.10.006
Smarkusz-Zarzecka J, Ostrowska L, Leszczyńska J, Orywal K, Cwalina U, Pogodziński D. Analysis of the impact of a multi-strain probiotic on body composition and cardiorespiratory fitness in long-distance runners. Nutrients. 2020;12. https://doi.org/10.3390/nu12123758
Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7. https://doi.org/10.1038/nature05488
Kim S, Kim JY, Lee DC, Lee HS, Lee JW, Jeon JY. Distribution of abdominal obesity and fitness level in overweight and obese Korean adults. Int J Endocrinol. 2014;2014:854392. https://doi.org/10.1155/2014/854392
Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009;119:1322–34. https://doi.org/10.1172/jci37385
Tang WH, Martin KA, Hwa J. Aldose reductase, oxidative stress, and diabetic mellitus. Front Pharm. 2012;3:87. https://doi.org/10.3389/fphar.2012.00087
Wang S, Pan J, Zhang Z, Yan X. Investigation of dietary fructooligosaccharides from different production methods: Interpreting the impact of compositions on probiotic metabolism and growth. J Funct Foods. 2020;69:103955. https://doi.org/10.1016/j.jff.2020.103955
Janochova K, Haluzik M, Buzga M. Visceral fat and insulin resistance–what we know? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2019;163:19–27. https://doi.org/10.5507/bp.2018.062
DiNicolantonio JJ, Mehta V, Onkaramurthy N, O’Keefe JH. Fructose-induced inflammation and increased cortisol: a new mechanism for how sugar induces visceral adiposity. Prog Cardiovasc Dis. 2018;61:3–9. https://doi.org/10.1016/j.pcad.2017.12.001
Behnsen J, Deriu E, Sassone-Corsi M, Raffatellu M. Probiotics: properties, examples, and specific applications. Cold Spring Harb Perspect Med. 2013;3:a010074. https://doi.org/10.1101/cshperspect.a010074
Nishimura S, Manabe I, Nagai R. Adipose tissue inflammation in obesity and metabolic syndrome. Disco Med. 2009;8:55–60.
Zatterale F, Longo M, Naderi J, Raciti GA, Desiderio A, Miele C, et al. Chronic adipose tissue inflammation linking obesity to insulin resistance and Type 2 diabetes. Front Physiol. 2019;10:1607. https://doi.org/10.3389/fphys.2019.01607
Le Barz M, Daniel N, Varin TV, Naimi S, Demers-Mathieu V, Pilon G, et al. In vivo screening of multiple bacterial strains identifies Lactobacillus rhamnosus Lb102 and Bifidobacterium animalis ssp. lactis Bf141 as probiotics that improve metabolic disorders in a mouse model of obesity. FASEB J. 2019;33:4921–35. https://doi.org/10.1096/fj.201801672R
Zhao X, Higashikawa F, Noda M, Kawamura Y, Matoba Y, Kumagai T, et al. The obesity and fatty liver are reduced by plant-derived Pediococcus pentosaceus LP28 in high fat diet-induced obese mice. PLoS One. 2012;7:e30696. https://doi.org/10.1371/journal.pone.0030696
Moon YJ, Baik SH, Cha YS. Lipid-lowering effects of Pediococcus acidilactici M76 isolated from Korean traditional makgeolli in high fat diet-induced obese mice. Nutrients. 2014;6:1016–28. https://doi.org/10.3390/nu6031016
Higashikawa F, Noda M, Awaya T, Danshiitsoodol N, Matoba Y, Kumagai T, et al. Antiobesity effect of Pediococcus pentosaceus LP28 on overweight subjects: a randomized, double-blind, placebo-controlled clinical trial. Eur J Clin Nutr. 2016;70:582–7. https://doi.org/10.1038/ejcn.2016.17
Zhang Q, Kim JH, Kim Y, Kim W. Lactococcus chungangensis CAU 28 alleviates diet-induced obesity and adipose tissue metabolism in vitro and in mice fed a high-fat diet. J Dairy Sci. 2020;103:9803–14. https://doi.org/10.3168/jds.2020-18681
Million M, Angelakis E, Paul M, Armougom F, Leibovici L, Raoult D. Comparative meta-analysis of the effect of Lactobacillus species on weight gain in humans and animals. Micro Pathog. 2012;53:100–8. https://doi.org/10.1016/j.micpath.2012.05.007
Choi JH, Moon CM, Shin TS, Kim EK, McDowell A, Jo MK, et al. Lactobacillus paracasei-derived extracellular vesicles attenuate the intestinal inflammatory response by augmenting the endoplasmic reticulum stress pathway. Exp Mol Med. 2020;52:423–37. https://doi.org/10.1038/s12276-019-0359-3
Malaguarnera M, Vacante M, Antic T, Giordano M, Chisari G, Acquaviva R, et al. Bifidobacterium longum with fructo-oligosaccharides in patients with non alcoholic steatohepatitis. Dig Dis Sci. 2012;57:545–53. https://doi.org/10.1007/s10620-011-1887-4
Anwar MA, Kralj S, Piqué AV, Leemhuis H, van der Maarel M, Dijkhuizen L. Inulin and levan synthesis by probiotic Lactobacillus gasseri strains: characterization of three novel fructansucrase enzymes and their fructan products. Microbiology. 2010;156:1264–74. https://doi.org/10.1099/mic.0.036616-0
Díez-Sainz E, Milagro FI, Riezu-Boj JI, Lorente-Cebrián S, Effects of gut microbiota-derived extracellular vesicles on obesity and diabetes and their potential modulation through diet. J Physiol Biochem. 2021:1-15. https://doi.org/10.1007/s13105-021-00837-6
Tong L, Hao H, Zhang X, Zhang Z, Lv Y, Zhang L, et al. Oral administration of bovine milk-derived extracellular vesicles alters the gut microbiota and enhances intestinal immunity in mice. Mol Nutr Food Res. 2020;64:e1901251. https://doi.org/10.1002/mnfr.201901251
Chelakkot C, Choi Y, Kim DK, Park HT, Ghim J, Kwon Y, et al. Akkermansia muciniphila-derived extracellular vesicles influence gut permeability through the regulation of tight junctions. Exp Mol Med. 2018;50:e450. https://doi.org/10.1038/emm.2017.282
Islam SU. Clinical uses of probiotics. Medicine. 2016;95:e2658. https://doi.org/10.1097/md.0000000000002658
Ouwehand A. A review of dose-responses of probiotics in human studies. Beneficial Microbes. 2017;8:143–51. https://doi.org/10.3920/BM2016.0140
Brusaferro A, Cozzali R, Orabona C, Biscarini A, Farinelli E, Cavalli E, et al. Is it time to use probiotics to prevent or treat obesity? Nutrients. 2018;10:1613. https://doi.org/10.3390/nu10111613
Kligler B, Cohrssen A. Probiotics. Am Fam Physician. 2008;78:e1073-8. Available from: https://www.aafp.org/afp/2008/1101/p1073.html.
Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. 2000;21:697–738. https://doi.org/10.1210/edrv.21.6.0415
(UK) NCCfNaSC. Irritable Bowel Syndrome in Adults: Diagnosis and Management of Irritable Bowel Syndrome in Primary Care. 2008.
Zhang Y, Li L, Guo C, Mu D, Feng B, Zuo X, et al. Effects of probiotic type, dose and treatment duration on irritable bowel syndrome diagnosed by Rome III criteria: a meta-analysis. BMC Gastroenterol. 2016;16:1–11. https://doi.org/10.1186/s12876-016-0470-z
Borgeraas H, Johnson L, Skattebu J, Hertel J, Hjelmesaeth J. Effects of probiotics on body weight, body mass index, fat mass and fat percentage in subjects with overweight or obesity: a systematic review and meta‐analysis of randomized controlled trials. Obes Rev. 2018;19:219–32. https://doi.org/10.1111/obr.12626
John GK, Wang L, Nanavati J, Twose C, Singh R, Mullin G. Dietary alteration of the gut microbiome and its impact on weight and fat mass: a systematic review and meta-analysis. Genes 2018;9:167.
Plaza-Diaz J, Ruiz-Ojeda FJ, Gil-Campos M, Gil A. Mechanisms of action of probiotics. Adv Nutr. 2019;10:S49–S66. https://doi.org/10.1093/advances/nmy063
Piqué N, Berlanga M, Miñana-Galbis D, Health benefits of heat-killed (Tyndallized) Probiotics: an overview. Int J Mol Sci. 2019;20. https://doi.org/10.3390/ijms20102534
Wilkins T, Sequoia J. Probiotics for gastrointestinal conditions: a summary of the evidence. Am Fam Physician. 2017;96:170–8.
Pisanu S, Palmas V, Madau V, Casula E, Deledda A, Cusano R, et al. Impact of a moderately hypocaloric mediterranean diet on the gut microbiota composition of Italian obese patients. Nutrients. 2020;12:2707. https://doi.org/10.3390/nu12092707
Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, et al. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019;7:14. https://doi.org/10.3390/microorganisms7010014
Rautio M, Jousimies-Somer H, Kauma H, Pietarinen I, Saxelin M, Tynkkynen S, et al. Liver abscess due to a Lactobacillus rhamnosus strain indistinguishable from L. rhamnosus strain GG. Clin Infect Dis. 1999;28:1159–60. https://doi.org/10.1086/514766
Nam SY. Obesity-related digestive diseases and their pathophysiology. Gut Liver. 2017;11:323–34. https://doi.org/10.5009/gnl15557
Wang X, Rao H, Liu F, Wei L, Li H, Wu C, Recent advances in adipose tissue dysfunction and its role in the pathogenesis of non-alcoholic fatty liver disease. Cells. 2021;10. https://doi.org/10.3390/cells10123300
Nawrot M, Peschard S, Lestavel S, Staels B. Intestine-liver crosstalk in Type 2 Diabetes and non-alcoholic fatty liver disease. Metabolism. 2021;123:154844. https://doi.org/10.1016/j.metabol.2021.154844
Yang R, Shang J, Zhou Y, Liu W, Tian Y, Shang H. Effects of probiotics on nonalcoholic fatty liver disease: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2021;15:1401–9. https://doi.org/10.1080/17474124.2022.2016391
Tang Y, Huang J, Zhang WY, Qin S, Yang YX, Ren H, et al. Effects of probiotics on nonalcoholic fatty liver disease: a systematic review and meta-analysis. Ther Adv Gastroenterol. 2019;12:1756284819878046. https://doi.org/10.1177/1756284819878046
Aller R, De Luis DA, Izaola O, Conde R, Gonzalez Sagrado M, Primo D, et al. Effect of a probiotic on liver aminotransferases in nonalcoholic fatty liver disease patients: a double blind randomized clinical trial. Eur Rev Med Pharm Sci. 2011;15:1090–5.
Asgharian A, Mohammadi V, Gholi Z, Esmaillzadeh A, Feizi A, Askari G. The effect of synbiotic supplementation on body composition and lipid profile in patients with NAFLD: a randomized, double blind, placebo-controlled clinical trial study. Iran Red Crescent Med. 2017;19:e42902. https://doi.org/10.5812/ircmj.42902
Acknowledgements
The authors would like to express their gratitude to Mtro. Ricardo Villegas Tovar, Coordinator of Scientific Production and International Visibility, BUAP.
Funding
This work was supported by grants from the Programa para el Desarrollo Profesional Docente (CA-160 FACMED) and the Vicerrectorıa de Investigacion, Benemerita Universidad Autonoma de Puebla, Mexico (GOMM-SAL21-G). The funders had no role in the study’s design, data collection or analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
LMP was responsible for designing the review protocol, writing the protocol, conducting the search, screening potentially eligible studies, extracting and analyzing data, interpreting results, the meta-regression analyses, updating reference lists, creating’ Summary of findings’ tables, and writing the report. GVM was responsible for conducting the search, screening potentially eligible studies, analyzing data, interpreting results, and writing the report. RGER was responsible screening potentially eligible studies, extracting and analyzing data, interpreting results, and writing the report. RPF was responsible for writing the protocol and provided feedback on the report. MEGM was responsible for designing the review protocol, writing the protocol, conducting the search, screening potentially eligible studies, arbitrating potentially eligible studies, interpreting results, making the artwork, updating reference lists, provided feedback on the report, and writing the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
No ethical approval was required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Porchia, L.M., Vazquez-Marroquin, G., Ochoa-Précoma, R. et al. Probiotics’ effect on visceral and subcutaneous adipose tissue: a systematic review of randomized controlled trials. Eur J Clin Nutr 76, 1646–1656 (2022). https://doi.org/10.1038/s41430-022-01135-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01135-0