Abstract
Objectives
To determine predictors of 25-hydroxyvitamin D3 (25(OH)D3) concentrations (25th, 50th, and 75th percentiles) in the third trimester of pregnancy.
Subjects/methods
Data on sociodemographic, obstetric, lifestyle and pregnancy characteristics, including serum 25(OH)D3 and retinol, were collected among 448 pregnant women who participated in the Maternal and Child Health and Nutrition in Acre, Brazil (MINA-Brazil Study) in Cruzeiro do Sul, Brazilian Amazon (latitude 7°S). Simultaneous-quantile regression was fitted to prospectively assess predictors at the 25th, 50th and 75th percentiles of 25(OH)D3 concentrations.
Results
In the third trimester, 25(OH)D3 <50 nmol/L was observed in 26% of pregnant women. Exposure to the Amazonian dry season during follow-up and vitamin D status ≥75 nmol/L in the second trimester of pregnancy were positively associated with 25(OH)D3 concentrations in the third trimester. Pregnant women who were the main providers of family income presented lower 25(OH)D3 concentrations (50th and 75th percentiles: −15 nmol/L, 95%CI −24; −3, p = 0.02, and −22 nmol/L, 95%CI −36; −7, p = 0.004, respectively), as well as those with sustained vitamin A insufficiency (25th and 50th percentiles: −27 nmol/L, 95%CI −40; −15, p < 0.001, and −17 nmol/L, 95%CI −33; −1, p = 0.04, respectively). Sun protection practices had a smaller negative impact on 25(OH)D3, restricted to participants whose concentrations were at the 25th percentile of the distribution.
Conclusions
Seasonality and vitamin A status were important predictors of 25(OH)D3 concentrations in the third trimester. Adequate exposure to sunlight and dietary sources of vitamin A within safe intake levels may help ensuring a good nutritional status of vitamin D during pregnancy.
Similar content being viewed by others
Introduction
Vitamin D status, as assessed by 25-hydroxyvitamin D (25(OH)D) concentrations, has been a worldwide target of research [1]. According to a systematic review [2], deficient 25(OH)D concentrations (<50 nmol/L) were identified among 54% of pregnant women (42–72% in North America, 18–90% in Europe, 46% in Eastern Mediterranean, 66–96% in Southeast Asia, and 41–97% in the Western Pacific). Evidence mostly from developed countries points out to associations of vitamin D deficiency during pregnancy with perinatal complications as preeclampsia [3], gestational diabetes mellitus [3], spontaneous foetal loss [4], preterm birth, and adverse anthropometric and neurodevelopmental outcomes [5].
Decreased dietary sources of vitamin D and reduced exposure to sunlight, due to seasonality, time spent outdoors and type of clothing, have been identified as factors associated with gestational 25(OH)D concentrations <50 nmol/L in the Middle East (latitudes 12°N–42°N) [6]. Recent cross-sectional and cohort investigations have reported similar findings in China, Indonesia, Malaysia, Saudi Arabia and the Switzerland [7,8,9,10,11], but there is still a paucity of longitudinal studies on predictors of vitamin D status during pregnancy in tropical, low to middle-income countries, and notably in Latin America and Africa [2]. In such settings, the burden of malnutrition frequently clusters micronutrient inadequacies [12]. Among Brazilian infants, for instance, each 1 μmol/L increase in retinol concentrations was associated with a 1.38-fold higher prevalence of vitamin D sufficiency (95%CI 1.18; 1.61) [13], but comparable analyses among pregnant women are scarce. As vitamins D and A play immunomodulatory roles, novel investigations exploring their potential synergic relationship seem important in pregnancy, given the relevance of foetal-maternal immune balance and several inflammatory pathways for successful perinatal outcomes [14].
Also, a majority of studies has focused on the dichotomous outcome of vitamin D deficiency [2]. Some studies have suggested, however, that maternal 25(OH)D ≥50 nmol/L would not guarantee an adequate vitamin D status for the neonate, as assessed in the cord blood [15], and that the chance for preterm birth was 62% lower (95%CI 0.23; 0.63) among pregnant women with 25(OH)D ≥100 nmol/L compared to those with 25(OH)D <50 nmol/L [16].
The present study aimed to prospectively investigate predictors of 25(OH)D3 concentrations in the third trimester among pregnant women in the Brazilian Amazon. We provide a comprehensive characterisation of predictors of 25(OH)D3 at the 25th, 50th, and 75th percentiles of its distribution, in a low to medium-income region close to the tropics, to favour promotion of a healthier vitamin D status and timely prevention of perinatal complications.
Subjects and methods
Study design and participants
The Maternal and Child Health and Nutrition in Acre, Brazil (MINA-Brazil Study) [17] is a population-based birth cohort conducted in Cruzeiro do Sul (latitude: −7.7, longitude: −72.7), a municipality in the Brazilian Amazon area. The city had an estimated population of 87,673 inhabitants in 2018 [18], with a Human Development Index of 0.664, classified as medium (between 0.600 and 0.699) and below the Brazilian national average [19]. The present prospective analysis focused on participants from the urban area of Cruzeiro do Sul, whose recruitment took place during pregnancy in each of the 13 primary health care units of the Family Health Strategy, while booking an antenatal care appointment. Pregnant women were screened between February 2015 and January 2016 [17]. Inclusion criteria were gestational age up to 20 weeks according to the last menstrual period (LMP), fixed residence in the urban area and intention to give birth in Cruzeiro do Sul. We estimated to screen around 854 pregnant women, based on the number of deliveries in the maternity hospital (n = 1780, in 2013), the proportion of residents in the urban area (60%), and coverage of local primary health care services (80%). Eligible pregnant women were invited to a baseline interview and two clinical evaluations; gestational age based on LMP was confirmed by ultrasound examination during the antenatal period [20]. Multiple pregnancies and participants without complete information on 25(OH)D3 concentrations during follow-up were excluded for the present analysis.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving participants were approved by the Institutional Review Board of the School of Public Health of the University of São Paulo (protocol number 872.613/2014). Written informed consent was obtained from all participants. In case of teenage pregnancies, the adolescent’s legal guardian provided consent.
Data collection and laboratory procedures
At baseline (median [interquartile range, IQR] gestational age: 16.9 [14.8, 19.1] weeks), trained research assistants conducted structured face-to-face interviews during home visits to collect data on each participant’s age, self-reported skin colour (as defined by the Brazilian Institute of Geography and Statistics: white, mulatto, black, yellow or indigenous), schooling (≤9 or >9 years), ownership of household assets for generating a wealth index (divided into tertiles) [21], assistance from the Bolsa Família conditional cash transfer programme (no or yes), living in a masonry household (no or yes), access to treated water (no or yes), septic destination of sewage (no or yes), number of residents in the household (≤4 or >4 people), pregnant woman as the main provider of family income (no or yes), presence of a smoker in the household (no or yes), parity (nulliparous, primiparous or multiparous), pre-pregnancy smoking (no or yes), and pre-pregnancy obesity (no or yes, according to body mass index [BMI] >30 kg/m² for adult women [22] and BMI-for-age z-score >2 for adolescents) [23]. The participant’s history of morbidities was also assessed during these interviews, including elevated blood pressure, hypertensive disorders, diabetes mellitus, gestational diabetes, kidney diseases (no or yes).
Two clinical evaluations were sequentially scheduled during the antenatal period at local primary health care units, in the second trimester (19.9 [18.2, 21.6] gestational weeks) and afterwards in the beginning of the third trimester (27.6 [26.9, 28.4] gestational weeks). In each evaluation, structured interviews and blood collection were performed by the study team.
Information was gathered on physical activity (practice of leisure walk, commuting and/or physical exercises in the last week; no or yes) [24], use of multiple micronutrient supplementation with vitamin D (no or yes), sunlight exposure (>30 min in the last week; no or yes) [25], and sun protection practices (use of sunscreen, shade structures and face protection; never/rarely/sometimes or very often/always). A sun protection score was conceived to depict the cumulative occurrence of factors influencing vitamin D endogenous synthesis [26, 27]. Non-white skin colour, no exposure to sunlight, and frequent sun protection practices accounted each for 1 point of in the score, varying from 0 to 5 points. Considering the midpoint of the score range, lower sun protection was defined at ≤2 points, while higher sun protection was denoted by >2 points.
Trained nursing technicians collected 8-hour fasting venous blood samples (approximately 10 mL) from participants in the second and third trimesters of pregnancy. Sterile vacuum blood collection tubes, with protection from light, were used for serum determination. Blood samples were allowed to clot and then were centrifuged within two hours of collection, in a swinging bucket centrifuge for 10 minutes at 3000 × g. Serum aliquots were immediately stored in amber conical microtubes and frozen at −20 °C before being sent on dry ice to the Laboratory of Human Nutrition (School of Public Health, University of São Paulo), where tubes were kept at −70 °C until analysis, within six months of each blood collection.
Serum concentrations of 25(OH)D3 in the second and third trimesters were determined on an isocratic HPLC system with UV detector with Chromsystems components and HPLC column, equilibrated and with test chromatogram (Chromsystems Instruments & Chemicals GmbH, Gräfelfing, Germany). Sample preparation was standardised strictly according to the manufacturer’s instructions, in light-protected reaction vials for precipitation and elution procedures, followed by the reading into the HPLC system. The limit of quantification was equivalent to 3.5 nmol/L, with linearity up to at least 624 nmol/L. The method presented intraassay and interassay coefficients of variation for 25(OH)D3 of 3.0% and 3.3%, respectively. Considering that vitamin D fortification or supplementation programs were not implemented at the population level in the study area or as a policy by the Brazilian Ministry of Health and that multiple micronutrient supplements referred by participants included exclusively 25(OH)D3 forms, it is possible to assume that serum 25(OH)D3 concentrations properly depicted vitamin D status. Vitamin D deficiency was defined as 25(OH)D3 <50 nmol/L and insufficiency as 25(OH)D3 <75 nmol/L [28].
According to serum retinol concentrations in the second and third trimesters, also analysed by standardised HPLC (Chromsystems Instruments & Chemicals GmbH, Gräfelfing, Germany), vitamin A insufficiency was defined as <1.05 µmol/L [29]. Vitamin A insufficiency during follow-up was depicted by combining information from both trimesters (never insufficient, insufficient in the 2nd or 3rd trimester, or always insufficient) [12]. C-reactive protein (CRP), a marker of acute inflammation, was measured in the third trimester of pregnancy only, using an ultrasensitive immunoturbidimetric assay (Roche Diagnostics, Basel, Switzerland). A cut-off point of 5 mg/L was used [30]. Blind samples of internal and external quality control were routinely used for each run. Coefficients of variation for these analyses were below 7%.
Seasonality at blood drawn was categorised according to the Amazonian weather as rainy season (November to March) or dry season (April to October). A combination of classifications in the second and third trimesters generated a variable covering seasonality during follow-up (always Amazonian rainy season, change in seasonality, or always Amazonian dry season).
Statistical analyses
The main outcome of interest was 25(OH)D3 concentrations in the third trimester of pregnancy. A conceptual framework with variables at distal, intermediate and proximal levels of determination, according to their influence on the outcome, was conceived based on evidence from the literature [31], to guide variable selection. Predictors of interest included sociodemographic conditions, obstetric history, lifestyle and pregnancy characteristics. First, median and IQR of 25(OH)D3 concentrations were compared across categories of predictors using Mann-Whitney or Kruskal-Wallis tests in unadjusted analysis.
Predictors of 25(OH)D3 concentrations were investigated by fitting simultaneous-quantile regression with bootstrapped standard errors at the 25th, 50th and 75th percentiles of its distribution, with the command sqreg in Stata. Quantile regression does not rely on normality assumptions and the estimation of coefficients at a given percentile is based on the reduction of the median absolute deviation, including a check function with asymmetric weights depending on the percentile. This approach may reveal effects of predictors at different segments of the outcome distribution, which could be especially useful in exploring 25(OH)D3 concentrations. The command sqreg, in particular, allows for the simultaneous estimation of all equations at once, with assessment of correlations between parameters for different percentiles and an estimate of the entire variance-covariance matrix of the estimators by bootstrapping [32]. Variables were included in the model if they were considered conceptually relevant and also following a data-driven approach based on the unadjusted analyses. Statistical significance (P < 0.05) was an additional criterion for retaining variables. With adjustment for the participant’s age and gestational age, coefficients and 95% confidence intervals (95%CI) for the association of each predictor with 25(OH)D3 concentrations in the third trimester were estimated at the 25th, 50th and 75th percentiles of the distribution. Differences in coefficients between percentiles of the 25(OH)D3 distribution were tested with interquantile regressions, by using the command iqreg (75th vs. 25th, 50th vs. 25th, and 75th vs. 50th percentiles).
A set of sensitivity analyses was performed. We run two alternative models excluding: (i) adolescent pregnant women; and (ii) all participants who reported a history of elevated blood pressure, hypertensive disorders, diabetes mellitus, gestational diabetes, or kidney diseases, considering the potential relationship of such conditions with vitamin D status. We also conceived models with additional adjustment for: (i) the use of multiple micronutrient supplements with vitamin D before the third trimester, although this was not a broad practice among the study population; and (ii) concentrations of CRP, as measured in the third trimester, taking into account that lower concentrations of retinol are associated with higher concentrations of acute phase proteins in inflammatory processes [30].
All analyses were performed using Stata 15.1 (Stata Corp, College Station, TX, USA).
Results
From 860 pregnant women initially screened in primary health care units, 699 were eligible according to inclusion criteria, of whom 41 refused to participate and 71 were not found for invitation and enrolment by the research team. Of 587 pregnant women included in the study, 448 had data on 25(OH)D3 concentrations in the second and third trimesters (Fig. 1). Among participants included in the analysis (n = 448), 29.2% had ≤9 years of schooling, in contrast to 32.4% among those not included (n = 139); 30.6% of those who were successfully followed up were from the lowest third of household wealth index as defined at baseline (P < 0.05). There were no differences regarding age, skin colour, type of household, sun exposure, seasonality at blood drawn, and nutritional status of vitamins D and A at the beginning of pregnancy.
Between February 2015 and January 2016,pregnant women were screened while booking an antenatal care appointment in the primary health care units of the urban area of Cruzeiro do Sul, Brazil. Reasons for exclusion and the final number of participants who completed a baseline interview and two clinical evaluations in the second and third trimesters of pregnancy are indicated.
Mean age of participants was 25 years (SD 6) and 20% were teenagers; 15.2% self-declared as white, 76.8% as mulatto, 4.2% as black, 2.9% as yellow and 0.9% as indigenous. There was no statistical difference in 25(OH)D3 concentrations among non-white groups. In the third trimester of pregnancy, median concentration of 25(OH)D3 among participants was 79 nmol/L, with the 25th and 75th percentiles of the distribution of 25(OH)D3 at 49 nmol/L and 110 nmol/L, respectively.
Considering the cut-off points at 50 nmol/L and 75 nmol/L, prevalence of vitamin D deficiency and insufficiency in the third trimester of pregnancy was equal to 26% and 47%, respectively. Between the second and third trimesters of pregnancy, the cumulative incidence of vitamin D deficiency was 23%; that of vitamin D insufficiency was 37%.
Median 25(OH)D3 concentrations in the third trimester were lower among pregnant women who were the main providers of family income (P = 0.04; Table 1). While exposure to the Amazonian dry season and vitamin D status ≥75 nmol/L in the second trimester were positively associated with 25(OH)D3 concentrations in the third trimester (P < 0.001; Table 2), sustained vitamin A insufficiency throughout pregnancy was related to lower median 25(OH)D3 (P = 0.04).
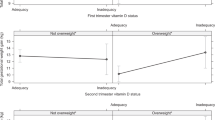
In adjusted simultaneous-quantile regression models (Table 3), we observed that 25(OH)D3 concentrations were significantly lower among pregnant women who were the main providers of family income, particularly at the 50th and 75th percentiles of the outcome distribution (−15 nmol/L, 95%CI −24; −3, and −22 nmol/L, 95%CI −36; −7, respectively), when compared to those who reported having a partner or other family members providing the majority of the income. A negative impact of sun protection practices was limited to pregnant women with 25(OH)D3 concentrations at the 25th percentile (−11 nmol/L, 95%CI −19; −3). As expected, exposure to the Amazonian dry season during follow-up and vitamin D status ≥75 nmol/L in the second trimester were consistently and positively associated with 25(OH)D3 concentrations in the third trimester of pregnancy. Interestingly, sustained vitamin A insufficiency during follow-up was associated with reductions in 25(OH)D3 concentrations (−27 nmol/L, 95%CI −40; −15 at the 25th percentile, and −17 nmol/L, 95%CI −33; −1 at the 50th percentile). Supplemental Fig. 1 illustrates the association of each predictor along the distribution of 25(OH)D3 concentrations in the third trimester of pregnancy. According to interquantile regression, significant differences were noted between coefficients estimated at each of the percentiles, as indicated in Table 3. Therefore, there is evidence that 25(OH)D3 concentrations were differently influenced by these predictors depending on the portion of the 25(OH)D3 distribution under examination.
In sensitivity analysis, there were no statistically significant differences to the final model in analysis excluding teenage participants or participants who reported a history of elevated blood pressure, hypertensive disorders, diabetes mellitus, gestational diabetes, or kidney diseases. Concentrations of 25(OH)D3 were not associated with the use of multiple micronutrient supplements with vitamin D after inclusion of this variable in the simultaneous-quantile regression model, and magnitude and direction of the coefficients related to all other predictors remained unchanged. No significant changes for the association with vitamin A status were observed with additional adjustment for CRP concentrations >5 mg/L.
Discussion
In this prospective study, 25(OH)D3 concentrations in the third trimester of pregnancy were positively associated with exposure to the Amazonian dry season and 25(OH)D3 ≥75 nmol/L in the second trimester, when compared, respectively, to those who were exposed to the Amazonian rainy season during pregnancy and those who had a vitamin D status <75 nmol/L in the second trimester. On the other hand, pregnant woman who reported being the main provider of family income and had insufficient vitamin A status presented lower 25(OH)D3 concentrations in the third trimester when compared to their counterparts.
We observed a median 25(OH)D3 concentration of 79 nmol/L among pregnant women in the present study, conducted at latitude 7°S. Overall, 26% of participants were vitamin D deficient in the third trimester. This figure was somewhat higher in comparison with a Brazilian prospective cohort conducted in Rio de Janeiro (10.2% in the third trimester, latitude 22°S) [33], but similar to a previous estimate from a population-based cohort (n = 7507) in the Netherlands (27% at 20.6 weeks of gestational age, 52°N) [34]. There is a remarkable difference, however, in relation to the occurrence of vitamin D deficiency among only 1% of pregnant women from traditional nomadic and semi-nomadic ethnical groups in Tanzania (2° to 4°S) [35]. Diverse latitudes and lifestyle factors regarding sun exposure habits should be highlighted, as well as differences in Human Development Index (0.761 for Rio de Janeiro; 0.922 for the Netherlands; 0.521 for Tanzania) [33,34,35,36], with the potential impact of inequalities on maternal health and vitamin D status.
In this sense, we noted that 25(OH)D3 concentrations were significantly lower among pregnant women who were the main providers of family income, particularly at the 50th and 75th percentiles of the outcome distribution, when compared to participants whose households were headed by other family members. This factor may be an indicative of greater socioeconomic vulnerability. There is evidence from studies in the Middle-East and Africa that household-heads have lower income and schooling level (below college education) in female-headed households than in male-headed households [37, 38]. While some studies from low and middle-income settings could not establish a relationship of socioeconomic variables with vitamin D status [8, 9, 39,40,41], a Saudi observational study has shown a protective role of higher maternal schooling on vitamin D deficiency in the first trimester among pregnant women in a tertiary antenatal care clinic (OR 0.32, 95%CI 0.12; 0.86) [7].
Importance of the endogenous synthesis of vitamin D through exposure to UVB light is well known. In our study, we observed a positive association of exposure to the Amazonian dry season during follow-up and 25(OH)D3 concentrations. Consistently, in a cross-sectional study with 147 Thai pregnant women from the University Hospital of Siriraj, blood collection during the rainy season was positively associated (OR 2.62, 95%CI 1.18; 5.85) with 25(OH)D <50 nmol/L at delivery [39]. Sun protection practices had a negative impact on 25(OH)D3 for participants whose concentrations were at the 25th percentile of the outcome distribution (49 nmol/L). According to NHANES 2003–2006, participants who reported frequently protecting themselves from sunlight with shade structures and clothing had twice the odds of vitamin D deficiency (OR 2.16, 95%CI 1.41, 3.32 for those who reported staying in the shade, and OR 2.11, 95%CI 1.48; 3.00 for those who reported wearing long sleeves, when compared to their counterparts), whilst use of sunscreen was not associated with vitamin D deficiency [42]. Our findings suggest that proper counselling on sun protection practices may be critical in the antenatal care devised to pregnant women with deficient 25(OH)D3 concentrations (<50 nmol/L).
Our analysis corroborated with evidence on the positive synergistic relationship between vitamins D and A during pregnancy. Analogously to our results, baseline data of a supplementation trial in Tanzania among 1,078 HIV-positive pregnant women between 12 and 27 gestational weeks showed that 25(OH)D <80 nmol/L was 13% lower with each 0.35 μmol/L increase in retinol concentrations [43]. The literature points that these fat-soluble vitamins have an interdependent role in regulating immune mechanisms, besides cellular apoptosis and gene transcription [44, 45]. At the nuclear level, retinoid X receptor can heterodimerise with vitamin D receptor into a complex that controls the expression of several genes involved in the inhibition of proinflammatory transcription factors and synthesis of inflammatory molecules [46]. While physiological changes induce an inflammatory state during pregnancy, the present observational finding supporting such interaction is of special interest given that exacerbated inflammatory responses may lead to gestational complications [14], outlining important roles for vitamins D and A in the third trimester. Of note, these findings were not substantially changed with further adjustment for C-reactive protein. Considering the frequent inadequacies in vitamin A status reported in pregnancy [47, 48], consumption of its dietary sources should be encouraged within safe intake levels, favouring fruits and vegetables high in carotenoids, with potential benefits for 25(OH)D3 concentrations.
There are some limitations to this study. First, losses to follow-up, mainly due to difficulties in contacting participants to attend the evaluations, were more frequent among poorer pregnant women, probably because poorer families move more frequently than the wealthier ones. Poorer areas lack standardisation of street and household numbers, and have more unstable cellular networks. Thus, selection bias cannot be completely ruled out. Given that our study population was from the urban area of Cruzeiro do Sul, caution is needed when extrapolating findings for pregnant women from rural regions, as patterns of work and sun exposure may vary. Although this study does not have detailed information on the consumption of dietary sources of vitamin D, their contribution to vitamin D status is apparently limited [27], especially considering the context of absence of vitamin D fortification or supplementation programs, as it is the case in Brazil and in the study area. In this sense, analysis further controlling for the use of multiple micronutrient supplements with vitamin D could not identify this practice as a significant predictor of 25(OH)D3 concentrations in the present study. Lack of information regarding dosage and frequency of these supplements may also be regarded as a limitation, as well as the use of self-reported questionnaires. Validity parameters for the proposed sun protection score would be desirable, in addition to the measurement of CRP also in the second trimester of pregnancy and other micronutrients and hormones related to vitamin D metabolism, but these were not available for this investigation. The present study has several strengths. We highlight its prospective design, with repeated data on biomarkers collected under high-quality conditions by periodically trained researchers. Moreover, the MINA-Brazil Study allowed the investigation of factors associated with 25(OH)D3 concentrations during pregnancy in a tropical middle-income area. The quantile regression approach added to the understanding of predictors along the distribution of 25(OH)D3 concentrations in the third trimester of pregnancy.
In conclusion, among pregnant women in the Brazilian Amazon, exposure to the dry season and vitamin D status ≥75 nmol/L in the second trimester were positively associated with 25(OH)D3 concentrations in the third trimester. Conversely, being the main provider of family income and presenting with sustained vitamin A insufficiency during pregnancy were associated with decreased 25(OH)D3 concentrations. These findings may contribute with tailoring of prevention and treatment strategies for optimising vitamin D status, taking into consideration the influence of predictors at different 25(OH)D3 concentrations that pregnant women may exhibit during the antenatal period. Counselling on adequate exposure to sunlight and dietary sources of vitamin A, amid better quality antenatal care, may help ensuring a good nutritional status of vitamin D during pregnancy and benefit maternal and child health.
Data availability
Additional data are available from the corresponding author on reasonable request.
References
Mulligan ML, Felton SK, Riek AE, Bernal-Mizrachi C. Implications of vitamin D deficiency in pregnancy and lactation. Am J Obstet Gynecol 2010;202:429,e1–9.
Saraf R, Morton SMB, Camargo CA, Grant CC. Global summary of maternal and newborn vitamin D status – a systematic review. Matern Child Nutr 2016;12:647–68.
Aghajafari F, Nagulesapillai T, Ronksley PE, Tough SC, O’Beirne M, Rabi DM. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: Systematic review and meta-analysis of observational studies. BMJ 2013;346:f1169.
Zhang H, Huang Z, Xiao L, Jiang X, Chen D, Wei Y. Meta-analysis of the effect of the maternal vitamin D level on the risk of spontaneous pregnancy loss. Int J Gynecol Obstet 2017;138:242–9.
Tous M, Villalobos M, Iglesias L, Fernández-Barrés S, Arija V. Vitamin D status during pregnancy and offspring outcomes: a systematic review and meta-analysis of observational studies. Eur J Clin Nutr 2020;74:36–53.
Hajizadeh S, Shary JR, Reed SG, Wagner CL. The prevalence of hypovitaminosis D and its risk factors in pregnant women and their newborns in the Middle East: A systematic review. Int J Reprod BioMed 2019;17:685–708.
Al-Musharaf S, Fouda MA, Turkestani IZ, Al-Ajlan A, Sabico S, Alnaami AM, et al. Vitamin D deficiency prevalence and predictors in early pregnancy among Arab Women. Nutrients 2018;10:489.
Woon FC, Chin YS, Ismail IH, Batterham M, Latiff AHA, Gan WY, et al. Vitamin D deficiency during pregnancy and its associated factors among third trimester Malaysian pregnant women. PLoS One 2019;14:e0216439.
Aji AS, Erwinda E, Yusrawati Y, Malik SG, Lipoeto NI. Vitamin D deficiency status and its related risk factors during early pregnancy: a cross-sectional study of pregnant Minangkabau women, Indonesia. BMC Pregnancy Childbirth 2019;19:183.
Cabaset S, Krieger JP, Richard A, Elgizouli M, Nieters A, Rohrmann S, et al. Vitamin D status and its determinants in healthy pregnant women living in Switzerland in the first trimester of pregnancy. BMC Pregnancy Childbirth 2019;19:10.
Shen Y, Pu L, Si S, Xin X, Mo M, Shao B, et al. Vitamin D nutrient status during pregnancy and its influencing factors. Clin Nutr 2020;39:1432–9.
Neves PAR, Castro MC, Oliveira CVR, Malta MB, Lourenço BH, Cardoso MA. Effect of Vitamin A status during pregnancy on maternal anemia and newborn birth weight: results from a cohort study in the Western Brazilian Amazon. Eur J Nutr 2020;59:45–56.
Lourenço BH, Silva LLS, Fawzi WW, Cardoso MA. Vitamin D sufficiency in young Brazilian children: associated factors and relationship with vitamin A corrected for inflammatory status. Public Health Nutr 2019;23:1226–35.
Momenttia AC, Estadella D, Pisani LP. Role of vitamin D in pregnancy and Toll-like receptor pathway. Steroids 2018;137:22–29.
Kiely ME, Wagner CL, Roth DE. Vitamin D in pregnancy: Where we are and where we should go. J Steroid Biochem Mol Biol 2020;201:105669.
McDonnell SL, Baggerly KA, Baggerly CA, Aliano JL, French CB, Baggerly LL, et al. Maternal 25(OH)D concentrations 40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS One 2017;12:e0180483.
Cardoso MA, Matijasevich A, Malta MB, Lourenco BH, Gimeno SGA, Ferreira MU, et al. Cohort profile: the Maternal and Child Health and Nutrition in Acre, Brazil, birth cohort study (MINA-Brazil). BMJ Open 2020;10:e034513.
Instituto Brasileiro de Geografia e Estatística. Cidades@ | Acre | Cruzeiro do Sul | Panorama. IBGE. 2019. https://cidades.ibge.gov.br/brasil/ac/cruzeiro-do-sul/panorama. Accessed 20 Sep 2021.
Programa das Nações Unidas para o Desenvolvimento, Instituto de Pesquisa Econômica Aplicada. Fundação João Pinheiro. Índice de Desenvolvimento Humano Municipal Brasileiro. Brasília: PNUD, Ipea, FJP. 2013. https://www.br.undp.org/content/brazil/pt/home/idh0/rankings/idhm-municipios-2010.html. Accessed 20 Sep 2021.
Lourenço BH, Lima DL, Vivanco E, Fernandes RB, Duarte M, Neves PAR, et al. Agreement between antenatal gestational age by ultrasound and clinical records at birth: A prospective cohort in the Brazilian Amazon. PLoS One 2020;15:e0236055.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data - or tears: An application to educational enrollments in states of India. Demography 2001;38:115–32.
World Health Organization. WHO Expert Committee on Physical Status. Physical status: the use of and interpretation of anthropometry, report of a WHO expert committee. WHO, Geneva. 1995. https://apps.who.int/iris/handle/10665/37003. Accessed 20 Sep 2021.
De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007;85:660–7.
Takito MY, Neri L de CL, Benício MHD. Evaluation of the reproducibility and validity of a physical activity questionnaire for pregnant women. Rev Bras Med Esport 2008;14(2):132–8.
World Health Organization . Vitamin and mineral requirements in human nutrition, 2nd ed. Geneva: WHO. 2004; p. 53. https://apps.who.int/iris/handle/10665/42716. Accessed 20 Sep 2021.
Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther 2010;23:48–60.
Holick MF. Vitamin D: A D-Lightful health perspective. Nutr Rev 2008;66:S182–194.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911–30.
World Health Organization. Global prevalence of vitamin A deficiency in population at risk 1995-2005. WHO, Geneva. 2009. https://apps.who.int/iris/bitstream/handle/10665/44110/9789241598019_eng.pdf. Accessed 20 Sep 2021.
Thurnham DI, McCabe GP, Northrop-Clewes CA, Nestel P. Effects of subclinical infection on plasma retinol concentrations and assessment of prevalence of vitamin A deficiency: meta-analysis. Lancet 2003;362:2052–8.
Victora CG, Huttly SR, Fuchs SC, Olinto MTA. The role of conceptual frameworks in epidemiological analysis: A hierarchical approach. Int J Epidemiol 1997;26:224–7.
StataCorp. Stata: Release 15. Statistical Software. College Station, TX: StataCorp LLC. 2017.
Figueiredo ACC, Cocate PG, Adegboye ARA, Franco-Sena AB, Farias DR, de Castro MBT, et al. Changes in plasma concentrations of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D during pregnancy: a Brazilian cohort. Eur J Clin Nutr 2017;57:1059–72.
Vinkhuyzen AAE, Eylesa DW, Burnea TH, Blanken LME, Kruithof CJ, Verhulst F, et al. Prevalence and predictors of vitamin D deficiency based on maternal mid-gestation and neonatal cord bloods: The Generation R Study. J Steroid Biochem Mol Biol 2016;164:161–7.
Luxwolda MF, Kuipers RS, Kema IP, van der Veer E, Dijck-Brouwer DA, Muskiet FA. Vitamin D status indicators in indigenous populations in East Africa. Eur J Nutr 2013;52:1115–25.
United Nations Development Program. Human Development Report. UNDP. 2015. http://hdr.undp.org/sites/default/files/hdr15_overview_pt.pdf. Accessed 20 Sep 2021.
Dominguez-Salas P, Alarcón P, Häsler B, Dohoo IR, Colverson K, Kimani-Murage EW, et al. Nutritional characterisation of low-income households of Nairobi: socioeconomic, livestock and gender considerations and predictors of malnutrition from a cross-sectional survey. BMC Nutr 2016;2:47.
Mohammadi-Nasrabadi F, Abdolahi M, Ghodsi D, Hoshiar-Rad A, Rezvani V, Ghafarpour M, et al. Do Iranian female-headed households have lower socio-economic and nutritional status compared to male-headed ones? Nutr Food Sci Res 2015;2:13–22.
Pratumvinit B, Wongkrajang P, Wataganara T, Hanyongyuth S, Nimmannit A, Chatsiricharoenkul S, et al. Maternal vitamin D status and its related factors in pregnant women in Bangkok, Thailand. PLoS One 2015;10:e0131126.
Lee CL, Ng BK, Wu LL, Cheah FC, Othman H, Ismail NAM. Vitamin D deficiency in pregnancy at term: Risk factors and pregnancy outcomes. Horm Mol Biol Clin Investig 2017;31:20170005.
Souza JRJL, Silva TSA, Figueredo ED. Hipovitaminose D na gestação: Um problema de saúde pública? Rev Bras Saúde Mater Infant 2019;19:207–15.
Linos E, Keiser E, Kanzler M, Sainani KL, Lee W, Vittinghoff E, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003–2006. Cancer Causes Control 2012;23:133–40.
Mehta S, Spiegelman D, Aboud S, Giovannucci EL, Msamanga GI, Hertzmark E, et al. Lipid-soluble vitamins A, D, and E in HIV-infected pregnant women in Tanzania. Eur J Clin Nutr 2010;64:808–17.
Shumutz EA, Zimmermann MB, Rohrmann S. The inverse association between serum 25‑hydroxyvitamin D and mortality may be modified by vitamin A status and use of vitamin A supplements. Eur J Nutr 2016;55:393–402.
Sha J, Pan J, Ping P, Xuan H, Li D, Bo J, et al. Synergistic effect and mechanism of vitamin A and vitamin D on inducing apoptosis of prostate cancer cells. Mol Biol Rep. 2013;40:2763–8.
Carazo A, Macáková K, Matoušová K, Krčmová LK, Protti M, Mladěnka P. Vitamin A update: Forms, sources, kinetics, detection, function, deficiency, therapeutic use and toxicity. Nutrients 2021;13:1703.
Neves PAR, Campos CAS, Malta MB, Lourenço BH, Castro MC, Cardoso MA. Predictors of vitamin A status among pregnant women in Western Brazilian Amazon. Br J Nutr 2019;121:202–11.
Santos Q, Sichieri R, Marchioni DML, Junior EV. Brazilian pregnant and lactating women do not change their food intake to meet nutritional goals. BMC Pregnancy Childbirth 2014;14:186.
Acknowledgements
The authors thank all the participants and health professionals involved in the study, as well as the State Health Secretariat of Acre, the Municipal Health Secretariat, the Primary Health Care Units of Cruzeiro do Sul.
Funding
This work is part of the MINA-Brazil Study, which was funded by the São Paulo Research Foundation (FAPESP grant 2016/00270-6; PI: MAC) and the Brazilian National Council for Scientific and Technological Development (CNPq grant 407255/2013-3; PI: MAC). CZR and TCC received scholarships from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES Finance Code 001). MAC is recipient of a senior research scholarship from CNPq. Organisations involved in the financial support of this work had no role in the design, analysis, or writing of this article.
Author information
Authors and Affiliations
Consortia
Contributions
CZR, TCC, and BHL conceived the analytical framework and performed the statistical analysis. PARN, MBM, MAC, and BHL participated in data collection and field overseen. MAC and BHL conceived the study design and methods. MAC was responsible for funding acquisition and project administration. CZR and TCC wrote the first draft of the paper, with critical appraisal by BHL. All authors reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving participants were approved by the Institutional Review Board of the School of Public Health of the University of São Paulo (protocol number 872.613/2014). Written informed consent was obtained from all participants. In case of teenage pregnancies, the adolescent’s legal guardian provided consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rodrigues, C.Z., Correia, T.C., Neves, P.A.R. et al. Predictors of 25-hydroxyvitamin D concentrations during pregnancy: A longitudinal analysis in the Brazilian Amazon. Eur J Clin Nutr 76, 1281–1288 (2022). https://doi.org/10.1038/s41430-022-01102-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01102-9