Abstract
Background/Objectives
A few studies reported association between placenta praevia (PP) and placental abruption (PA) with maternal iron deficiency anaemia (IDA), which is not an established risk factor for these conditions. This retrospective case-control study was performed to determine the relationship between IDA with PP and PA.
Methods
Maternal characteristics, risk factors for and incidence of antepartum haemorrhage overall, and PP and PA, were compared between women with IDA only and controls without IDA or haemoglobinopathies matched for exact age and parity (four controls to each index case), who carried singleton pregnancy to ≥22 weeks and managed under our care from 1997 to 2019.
Results
There were 1,176 women (0.8% of eligible women in the database) with IDA only, who exhibited slightly but significantly different maternal characteristics, and increased antepartum haemorrhage overall (3.4% versus 2.2%, p = 0.031, OR 1.522, 95% CI 1.037–2.234) and PP (1.8% versus 0.9%, p = 0.010, OR 1.953, 95% CI 1.164–3.279), but not PA (1.2% versus 1.1%, p = 0.804, OR 1.077, 95% CI 0.599–1.936). When stratified by parity status, increased PP was found in nulliparous women only. On multivariate analysis adjusting for parity, previous abortion history, overweight and obesity, short stature, other antenatal complications as a composite factor, preterm (<37) delivery, previous caesarean delivery, and infant gender, IDA was associated with PP (aOR 3.485, 95% CI 1.959–6.200) and PA (aOR 2.181, 95% CI 1.145–4.155).
Conclusions
Both PP and PA are increased in women with IDA, the prevention of which could be a means to reduce the occurrence of both PP and PA.
Similar content being viewed by others
Introduction
Anaemia is probably the commonest pregnancy complication with global prevalence of 38% [1], and prevalence of 21–35% [2] and 25.9% [3] in European countries and Canada respectively. The leading cause of anaemia is iron deficiency, which was found to increase from 6.9% to 14.3% to 28.4% from the first to the third trimester in the US [4], and in one of every five women at the beginning of pregnancy in Australia [5]. Maternal anaemia leads to compensatory placenta hypertrophy, manifesting by the significant correlation between reductions in haemoglobin (Hb) [6,7,8] and mean cell volume (MCV) [9] with placental weight. Hence the placenta becomes larger relative to fetal size, so that the placental-to-fetal weight ratio (placental ratio) is increased in both iron deficiency anaemia (IDA) and thalassaemia traits [9,10,11]. Placental hypertrophy is accomplished through increased villus proliferation [12] resulting in a significant inverse correlation between the absolute volume and surface area of the intervillous space and villi with maternal Hb [13] There is in addition increased density and reduced apoptotic rate in the extravillous trophoblast, which invades deeper from the endometrial-myometrial border into the myometrium [14] and greater invasion into the spiral arteries increases the lumen of spiral arteries thus increasing perfusion of the intervillous space [15]. These are seen as compensatory measures to enhance maternal-fetal gas exchange in face of maternal anaemia.
Whether these placental adaptive changes could lead to increased risk of antepartum haemorrhage (APH) is unclear, but there are occasional reports on an association between IDA with placenta praevia (PP) [16] and placental abruption (PA) [17, 18]. Yet the literature on risk factors for PP and PA include advancing maternal age, multiparity, previous caesarean delivery (CD) and abortion, being Asian or African in a multiracial society, and carrying a male fetus [19,20,21,22,23,24,25], but not anaemia nor IDA. Nevertheless, placental implantation abnormalities increase both preterm delivery (PTD) and low birthweight (LBW) infants [26,27,28,29] which are also associated with IDA [30,31,32]. Therefore placental compensatory changes could have resulted in implantation abnormalities which in turn lead to PTD and LBW infants.
In view of the reported increasing incidence of PP [28, 33], and the revelation of the persistently high prevalence of anaemia and iron deficiency globally, even in developed countries [1,2,3,4,5], we hypothesize that IDA could have been an overlooked factor contributing to placentation abnormalities manifesting as PP and PA, and its high prevalence and often overlooked presence [1,2,3,4,5] could have contributed to the the increasing prevalence of PP [28, 33]. This retrospective case-control study was therefore conducted in the obstetric population served by our hospital to clarify the relationship between IDA with PP and PA.
Materials and methods
This is a single-centre retrospective case-control study on the pregnant women with singleton pregnancies carried to 22 completed weeks of gestation and beyond, who were delivered in our hospital between January 1997 and December 2019. During this period there were a total of 147,473 women registered in our obstetric database. Our hospital is one of eight public obstetric units operating under the local Hospital Authority to provide free obstetric care to residents, and serves a population of 1.7 million with an annual delivery rate of 7000. At antenatal booking, a medical and obstetric history is taken by midwives, and then checked by the medical staff for referrals where appropriate. Routine measurements of maternal height and weight are taken at booking to calculate the body mass index (BMI). Maternal blood is drawn for the routine antenatal tests which include measurement of Hb and red cell indices using an automated counter. Antenatal anaemia is defined as a Hb level of <10 g/dL at any time during pregnancy. If the MCV is <80 fL, further investigations including Hb pattern and serum ferritin level are arranged. If the MCV is normal, only iron profile is assessed, and IDA is diagnosed by a serum ferritin level of <15 μg/L, for which oral ferrous sulphate tablets 300 mg daily are prescribed. Parenteral iron therapy is not given. If the serum ferritin is between 15 and <30 μg/L, either ferrous sulphate or a proprietary preparation of minerals and multivitamin supplement (Materna®) is prescribed. Depending on the initial Hb level, repeat measurement is arranged at intervals or at the third trimester. Obstetric management is based on medical indications and protocol-driven. Any finding of low-lying placenta or placenta praevia by ultrasonography is confirmed at delivery. The diagnosis of PA is based on the clinical evidence of antepartum haemorrhage and retroplacental blood collection/clots found at delivery. The medical and obstetric history, results of antenatal investigations, current obstetric complications, and pregnancy outcome, are captured in an electronic record system. The data is then extracted, anonymised and summarised to generate statistics for regular auditing and submission to the Hospital Authority. The patients’ electronic records are not accessible to maintain confidentiality. This study utilised the statistical database, the accuracy of which was validated before [34]. The study was approved by the Institutional Review Board (Joint Chinese University of Hong Kong—New Territories East Cluster Clinical Research Ethics Committee, Reference Number CRE-2017.442).
The inclusion criteria for the cases were women carrying singleton pregnancy carried to 22 weeks gestation or more, with a diagnosis of IDA. Women with haemoglobinopathies were excluded. For each case, four controls matched for exact age and parity, and similarly carried singleton pregnancy to 22 weeks gestation and beyond, were selected at random from the women without IDA or haemoglobinopathies in the database for comparison. Owing to the lower prevalence of PP in nulliparous women, and the fact about half of our parturients were nulliparous over some of these years, for each case we selected four matched controls for comparison. For cases of higher order of parity (>3), controls with age varying by ± one year or parity varying by ± 1 would be selected if there were insufficient fully matched controls for an index case. The following parameters were compared between women with and without IDA: demographic and anthropometric parameters including previous abortion history, overweight (BMI ≥ 25 kg/m2 at booking), and short stature (defined as height ≤ the 25th percentile value of 154 cm in our population [34]) which increases the risk of CD; overall incidence of antenatal complications (including pregnancy hypertensive disorders, gestational diabetes mellitus, APH, and PTD) grouped together as a composite factor, PTD (<37 completed weeks) specifically, previous CD among the multiparous cases and controls, fetal non-cephalic presentation, incidence of CD, and infant gender. These factors examined were common risk factors for PP and PA as described previously [19,20,21,22,23,24,25]. The comparison of APH consisted of APH overall (including women with history of APH the cause of which could not be clearly defined at delivery) and PP and PA as specific diagnosis of APH. The data was expressed in mean ± standard deviation (SD) and analysed with the t test for continuous variables, and in number and / or percentage and analysed with the chi square test (Fisher’s exact test if the number in any cell was ≤5), generating the odds ratio (OR) and 95% confidence intervals (CI), for categorical variables with the data of the controls serving as the referent. The independent association of IDA and the other confounding factors with overall APH, PP and PA was finally examined by multiple logistic regression analysis, adjusting for the parameters which demonstrated significant differences in the univariate analysis and entered into the equation. In the analysis, the cases and controls were amalgamated. The results of the multiple logistic regression analysis were expressed as adjusted odds ratio (aOR) with 95% CI. Statistical analysis was performed using a commercially available statistical package (PASW Statistics 26.0, SPSS Inc., Chicago, Il).
Results
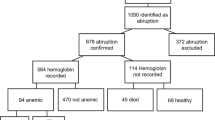
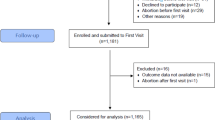
During the period there were 147,473 women in the database, 1176 women (0.8%) were eligible and included in the study. A total of 4704 controls were selected from the database matched for exact parity and age for all nulliparous women, exact parity and age for women with parity = 1, 2, and 3, and parity ±1 or age ±1 year for women at parity >3. The mean age of cases and controls was 30.2 ± 6.0 years, 25.6% and 3.3% of each group were at/above age 35 years and <20 years respectively. Nulliparous women accounted for 44.9% in each group, while among the multiparous women those with previous CD were found in 21.4% and 20.4% respectively (Table 1). The cases were slightly but significantly shorter, heavier, with a higher BMI (p < 0.001), and they had higher incidence of short stature (31.5% versus 24.7%, OR 1.273, 95% CI 1.154–1.405) and high BMI (29.1% versus 22.9%, OR 1.273, 95% CI 1.148–1.412). The cases had a lower incidence of previous abortion (40.9% versus 45.0%, OR 0.910, 95% CI 0.843–0.981) which was related to a significantly lower incidence among the multiparas (46.9% versus 52.4%, or 0.895, 95% CI 0.818–0.979). The cases also had a lower overall incidence of obstetric complications (20.7% versus 32.4%, OR 0.640, 95% CI 0.568–0.721) and PTD at <37 weeks (6.8% versus 9.8%, OR 0.697, 95% CI 0.555–0.876). There was no difference in non-cephalic and breech presentation, or in the incidence of male infants, but both the mean gestational age and birthweight were slightly but significantly greater among the cases.
When the occurrence of APH was analysed, the cases had a higher incidence of APH overall (3.4% versus 2.2%, OR 1.522, 95% CI 1.037–2.234) which was due to the higher incidence among nulliparous women (3.8% versus 1.3%, OR 2.938, 95% CI 1.589–5.433) only (Table 2). For PP, again the overall incidence was higher among the cases (1.8% versus 0.9%, OR 1.953, 95% CI 1.164–3.279) which was due to the higher incidence among the nulliparous women (1.7% versus 0.4%, OR 4.500, 95% CI 1.745–11.61). For PA, there was no significant difference between cases and controls overall or for either nulliparous or multiparous women.
On multiple logistic regression analysis (Table 3), the significant independent factors associated with APH overall included PTD (aOR 1.930, 95% CI 1.305–2.855) and IDA (aOR 2.660, 95% CI 1.726–4.098), whereas high BMI was associated with reduced APH (aOR 0.498, 95% CI 0.314–0.788). The factors associated with increased PP were similarly PTD (aOR 2.706, 95% CI 1.564–4.684) and IDA (aOR 3.485, 95% CI 1.959–6.200). However, for PA, only IDA was associated with an increase (aOR 2.181, 95% CI 1.145–4.155) whereas high BMI was associated with reduced (aOR 0.282, 95% CI 0.125–0.634) incidence.
Discussion
This study demonstrated that even when matched for age and parity, women with IDA still exhibited different characteristics, with lower incidence of previous abortion and obstetric complications, but no difference in the incidence of previous CD. Yet, they had significantly increased overall APH and PP, which were confined to nulliparous women. On multivariate analysis, IDA was found to be associated with not only overall APH and PP, but also with PA as well, thus confirming the findings in the previous reports [16,17,18]. In our model, the only other significant factor found was PTD, which was more likely consequential to rather than causative of PA and PP. This would suggest that PTD attributed to IDA could have PP and PA as one of the underlying mechanisms.
Limited by the lack of data, we could not correlate the lowest Hb level or maternal iron status with the position of the placenta and type of placenta praevia at delivery, and the estimated amount of blood clots found in the cases of PA. However, as the timing and duration of both IDA and iron deficiency would have been variable, any attempts at the correlation between these continuous parameters with the types of PP and retroplacental clots in PA may not be meaningful, especially when oral iron treatment would have been promptly prescribed. Indeed, the 0.8% prevalence of IDA was suggestive of a low prevalence of underlying iron deficiency, probably related to improvements in socioeconomic condition and nutritional status in our society over the past two decades, as well as the liberal intake of antenatal supplements. By the exclusion of women with haemoglobinopathies, our cases and controls represented a homogenous group. This factor, together with the relatively large sample size, the single centre nature with standard protocols and uniform approach in antenatal care and management, would ensure consistency and robust results, and indicated that notwithstanding its low prevalence, IDA is still an independent risk factor for both PP and PA, and the fact that the association with PP was confined to nulliparous gravidae indicated that the mechanism most probably involved interference with placental migration in an unscarred uterus.
The strengths of this study are first, the women were all from the same population and ethnic background. Second, although retrospective in nature, this was a single centre study where the diagnosis and management of APH have remained uniform and consistent throughout the study period. Third, with a reasonable sample size of >1100 cases and four matched controls selected for each index case, our study was estimated to have sufficient power to discriminate the effects of confounding conditions with even single-digit incidence which could have served as risk factors or causes of APH in women with and without IDA. The limitations include the lack of detailed information regarding the actual placental location (in terms of distance from or the extent of covering the internal os) in women with placenta praevia, the size of the retroplacental clot in women with placental abruption, the latest and the lowest Hb level, serum parameters of iron deficiency and ferritin levels, and the gestation at diagnosis of IDA, which were not captured in the statistics database. Thus we were unable to examine the relationship between the severity of iron deficiency and IDA with the extent of placenta praevia and severity of placental abruption. However, with the relationship between IDA and placenta praevia and placental abruption established in this study, prospective observational studies can now be designed and conducted in the future to address these questions.
The likelihood of an initially low-lying placenta evolving into PP at delivery is related to the distance of its lower edge from the internal os, and the rate of migration towards the upper uterine segment which, in turn, is influenced by its location relative to the internal os. For placentas with the edge within 3 cm of the internal os, migration reduced this incidence from 8.08% at 18–20 weeks gestation to 2.36% at term [35] and for placentas with the edge at between -20 to +20 mm from the internal os, 88.5% of the cases migrated without the need for CD [36]. If the placental edge was within 3 cm of the internal os at ≥26 weeks gestation, those who required CD had a mean rate of migration of 0.3 mm/week, whereas those who did not require CD had a migration rate of 5.4 mm/week [36]. Even when the placenta was low-lying at 30–37 weeks, none of those which migrated at >2.0 mm/week required CD, in contrast to 56.3% in those migrating at <2.0 mm/week [37]. The final distance of the placental edge from the internal os correlates with the rate of migration [38] which is influenced by previous obstetric history, being 78.6%, 62.5%, and 40% for women with previous normal delivery, prior history of dilatation and curettage or manual removal of placenta, and prior CD respectively [35]. Indeed, for low-lying placenta at 28 weeks, women with parity ≥2 or prior CD showed no significant migration at 28–36 weeks gestation, and the influence of maternal age on rate of migration was negated by parity or prior CD or placental location [39]. The effect of multiparity on placental migration could be related to placental scars and is influenced by the number of previous pregnancy, as demonstrated in laboratory animals [40, 41], which probably explains the impact of parity ≥2 on placental migration [39]. On the basis of these reports, the association between IDA with PP in nulliparous women would suggest that IDA-induced increased extravillous trophoblast invasion [14, 15] interferes with placental migration, while the increased relative placental size has increased the likelihood of its lower edge extending closer to the internal os from early pregnancy when the uterus is still small. Thus increased likelihood of a shorter distance to the internal os and reduced rate of migration would have rendered the placenta at greater risk of being praevia at delivery among nulliparas. Whereas in multiparas, the presence of placental scars and/or scars from previous CD would be sufficient to interfere with placental migration anyway so that the effect of IDA becomes negligible.
The demonstration of the association between IDA with PA only through multivariate analysis indicates that the association is generally masked by other conditions, and suggests that the underlying process is most likely mediated through a series of mechanisms. The increased luminal dilatation of the uterine spiral arteries induced by greater extravillous trophoblast invasion [14, 15], concomitant with increased placental production of vascular endothelial growth factor, placental growth factor, nitrotyrosine residues, and nitric oxide synthase (NOS) in the villous trophoblast [42, 43], probably results in sustained maternal vasodilatation and increased blood flow especially in the last trimester. As increased blood flow per se could induce oxidative stress through an endothelium- and nitric oxide-independent mechanism [44], and as oxidative stress leads to tissue injury, endothelial dysfunction and inflammation [45], this sequence could eventually result in acute vasospasm and rupture of the decidual blood vessels, events found to precede PA [46]. In addition to PA, the cumulative effects, or a sudden and exaggerated episode of this process, could lead to release of decidual-cell expressed tissue factor and thrombin generation, increased expression of matrix metalloproteinases, and attraction of neutrophil-chemoattracting and –activating cytokines, which together induce preterm labour [47]. Although the aforementioned hypothesis remains to be proven, this could explain the independent association between IDA with PA after adjustment for PTD in our model, and the increase in PTD reported before [30,31,32].
Conclusion
Globally, the prevalence of PP is highest in studies from Asia (12.2/1000 pregnancies) and lower among studies from Europe (3.6/1000 pregnancies), North America (2.9/1000 pregnancies) and Sub-Saharan Africa (2.7/1000 pregnancies) [48]. Similarly the rates of PA varied across two North American (US and Canada) and five European (Sweden, Norway, Finland, Denmark, and Spain) countries (from 3–10 per 1000), exhibiting opposite temporal trends, and the period effects could only be partially explained by changes in smoking prevalence in the US and Sweden [49]. The global prevalence of iron deficiency was highest in Southeast Asia (49–60%) but only 8% in North America [50], while that of IDA in pregnant women aged 15–49 years was 23% in high income regions, 34–53% in Asia, and 34–61% in Africa [1]. The similarities between the patterns of iron deficiency and IDA with those of PP and PA, together with the results of this study, would suggest that IDA has probably played a hitherto overlooked role in the development of PP and PA. There is consensus on the role of iron supplementation in optimising the outcome of pregnancy and the offspring, and the finding of this study has added yet another reason of why it is so important to prevent the development of IDA especially in nulliparous women. While our finding needs to be confirmed in prospective observational studies and randomised controlled trials of sufficient sample size, it is prudent meanwhile to advise routine maternal iron supplementation especially in high-risk populations and vulnerable social groups in order to reduce the incidence and consequences of IDA.
References
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16–25. https://doi.org/10.1016/S2214-109X(13)70001-9.
Milman N, Taylor CL, Merkel J, Brannon PM. Iron status in pregnant women and women of reproductive age in Europe. Am J Clin Nutr. 2017;106:1655S–1662S. https://doi.org/10.3945/ajcn.117.156000.
Tang G, Lausman A, Abdulrehman J, Petrucci J, Nisenbaum R, Hicks LK, et al. Prevalence of iron deficiency and iron deficiency anemia during pregnancy: a single centre Canadian study. Blood. 2019;134:3389 https://doi.org/10.1182/blood-2019-127602.
Cantor AG, Bougastsos C, Dana T, Blazina I, McDonagh M. Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:566–76. https://doi.org/10.7326/M14-2932.
Khambalia AZ, Collins CE, Roberts CL, Morris JM, Powell KL, Tasevski V, et al. Iron deficiency in early pregnancy using serum ferritin and soluble transferrin receptor concentrations are associated with pregnancy and birth outcomes. Eur J Clin Nutr. 2016;70:358–63. https://doi.org/10.1038/ejcn.2015.157.
Beischer NA, Sivasamboo R, Vohra S, Silpisornkosal S, Reid S. Placental hypertrophy in severe pregnancy anaemia. J Obstet Gynaecol Br Commw. 1970;77:398–409. https://doi.org/10.1111/j.1471-0528.1970.tb03541.x.
Jwa SC, Fujiwara T, Yamanobe Y, Kozuka K, Sago H. Changes in maternal haemoglobin during pregnancy and birth outcomes. BMC Pregnancy Childbirth. 2015;15:80 https://doi.org/10.1186/s12884-015-0516-1.
Larsen S, Bjelland EK, Haavaldsen C, Eskild A. Placental weight in pregnancies with high or low haemoglobin concentrations. Eur J Obstet Gynecol Reprod Biol. 2016;206:48–52. https://doi.org/10.1016/j.ejogrb.2016.08.039.
Godfrey KM, Redman CWG, Barker DJP, Osmond C. The effect of maternal anaemia and iron deficiency on the ratio of fetal weight to placental weight. Br J Obstet Gynaecol. 1991;98:886–91.
Lao TT, Wong WM. Placental ratio—its relationship with mild maternal anaemia. Placenta. 1997;18:593–6. https://doi.org/10.1016/0143-4004(77)90015-7.
Lao TT, Tam KF. Placental ratio and anemia in third trimester pregnancy. J Reprod Med. 2000;45:923–8. PMID:11127105.
Kosanke G, Kadyrov M, Korr H, Kaufmann P. Maternal anemia results in increased proliferation in human placental villi. Trophobl Res. 1998;11:339–57. https://doi.org/10.1016/S0143-4004(98)80024-6.
Huang A, Zhang R, Yang Z. Quantitative (stereological) study of placental structures in women with pregnancy iron-deficiency anemia. Eur J Obstet Gynecol Reprod Biol. 2001;97:59–64.
Kadyrov M, Schmitz C, Black S, Kaufmann P, Huppertz B. Pre-eclampsia and maternal anaemia display reduced apoptosis and opposite invasive phenotypes of extravillous trophoblast. Placenta. 2003;24:540–8. https://doi.org/10.1053/plac.2002.0946.
Kadyrov M, Kingdom JCP, Huppertz B. Divergent trophoblast invasion and apoptosis in placental bed spiral arteries from pregnancies complicated by maternal anemia and early-onset preeclampsia/intrauterine growth restriction. Am J Obstet Gynecol. 2006;194:557–63. https://doi.org/10.1016/j.ajog.2005.07.035.
Smith C, Teng F, Branch E, Chu S, Joseph KS. Maternal and perinatal morbidity and mortality associated with anemia in pregnancy. Obstet Gynecol. 2019;134:1234–44. https://doi.org/10.1097/AOG.0000000000003557.
Arnold DL, Williams MA, Miller RS, Qiu C, Sorensen TK. Iron deficiency anemia, cigarette smoking and risk of abruptio placentae. J Obstet Gynaecol Res. 2009;35:446–52.
Beckert RH, Baer RJ, Anderson JG, Jelliffe-Pawlowski LL, Rogers EE. Maternal anemia and pregnancy outcomes: a population-based study. J Perinatol. 2019;39:911–9. https://doi.org/10.1038/s41372-019-0375-0.
Taylor VM, Peacock S, Kramer MD, Vaughn TL. Increased risk of placenta previa among women of Asian Origin. Obstet Gynecol. 1995;86:805–8.
Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of caesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol. 1997;177:1071–8.
Demissie K, Breckenbridge MB, Joseph L, Rhoads GG. Placenta previa: preponderance of male sex at birth. Am J Epidemiol. 1999;149:824–30.
Wen SW, Demissie K, Liu S, Marcoux S, Kramer MS. Placenta praevia and male sex at birth: results from a population-based study. Paediatr Perinat Epidemiol. 2000;14:300–4.
Johnson LG, Mueller BA, Daling JR. The relationship of placenta previa and history of induced abortion. Int J Gynecol Obstet. 2003;81:191–8.
Kim LH, Caughey AB, Laguardia JC, Excobar GJ. Racial and ethnic differences in the prevalence of placenta previa. J Perinat. 2012;32:260–4.
Aliyu MH, Salihu HM, Lynch O, Alio AP, Marty PJ. Placental abruption, offspring sex, and birth outcomes in a large cohort of mothers. J Matern Fetal Neonatal Med. 2012;25:248–52.
Crane JMG, Van den Hof MC, Dodds L, Armson BA, Liston R. Neonatal outcomes with placenta previa. Obstet Gynecol. 1999;93:541–4.
Zlatnik MG, Cheng YW, Norton ME, Thiet M-P, Caughey AB. Placenta previa and the risk of preterm delivery. J Matern Fetal Neonatal Med. 2007;20:719–23.
Kollmann M, Gaulhofer J, lang U, Klaritsch P. Placenta praevia: incidence, risk factors and outcome. J Matern Fetal Neonatal Med. 2016;29:1395–8.
Vahanian SA, Lavery JA, Ananth CV, Vintzileos A. Placental implantation abnormalities and risk of preterm delivery: a systematic review and metaanalysis. Am J Obstet Gynecol. 2015;213 Suppl 4:S78–S90 .https://doi.org/10.1016/j.ajog.2015.05.058.
Malhotra M, Sharma JB, Batra S, Sharma S, Murthy NS, Arora R. Maternal and perinatal outcome in varying degrees of anemia. Int J Gynecol Obstet. 2002;79:93–100.
Levy A, Fraser D, Katz M, Mazor M, Sheiner E. Maternal anemia during pregnancy is an independent risk factor for low birthweight and preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2005;122:182–6.
Tzur T, Weintraub AY, Sergienko R, Sheiner E. Can anemia in the first trimester predict obstetrical complications later in pregnancy? J Matern Fetal Neonatal Med. 2012;25:2454–7.
Roberts CL, Algert CS, Warrendorf J, Olive EC, Morris JM, Ford JB. Trends and recurrence of placenta praevia: a population-based study. Aust N Z J Obstet Gynaecol. 2012;52:483–6.
Lao TT, Hui ASY, Sahota DS, Leung TY. Maternal height and risk of hypertensive disorders in pregnancy. J Matern Fetal Neonatal Med. 2019;32:1420–5. https://doi.org/10.1080/14767058.2017.1410786.
Shravage JC, Dhumale HA, Bellad MB. Assessment of placental migration in mid trimester low lying placenta. J Obstet Gynecol India. 2009;59:317–9.
Oppenheimer L, Holmes P, Simpson N, Dabrowski A. Diagnosis of low-lying placenta: can migration in the third trimester predict outcome? Ultrasound Obstet Gynecol. 2001;18:100–2.
Ohira S, Kikuchi N, Kobara H, Osada R, Ashida T, Kanai M, et al. Predicting the route of delivery in women with low-lying placenta using transvaginal ultrasonography: significance of placental migration and marginal sinus. Gynecol Obstet Invest. 2012;73:217–22.
Predanic M, Perni SC, Baergen RN, Jean-Pierre C, Chasen ST, Chervenak FA. A sonographic assessment of different patterns of placenta previa “migration” in the third trimester of pregnancy. J Ultrasound Med. 2005;24:773–80.
Predanić M, Perni SC, Baergen RN, Chasen ST. Ultrasound assessment of placenta previa “migration” in relationship to maternal demographic factors. Gynaecol Perinatol. 2007;16:9–13.
Davis DE, Emlen JT Jr. The placental scar as a measure of fertility in rats. J Wildl Manag. 1948;12:162–6.
Momberg H, Conaway C. The distribution of placental scars of first and second pregnancies in the rat. J Embryol Exp Morph. 1956;4:376–84.
Al-Hijji J, Andolf E, Laurini R, Batra S. Nitric oxide synthase activity in human trophoblast, term placenta and pregnant myometrium. Reprod Biol Endocrinol. 2003;1:51 http://www.RBEj.com/content/1/1/51.
Surekha MV, Singh S, Sarada K, Sailaja G, Balakrishna N, Srinivas M, et al. Study on the effect of severity of maternal iron deficiency anaemia on regulators of angiogenesis in placenta. Fetal Pediatr Pathol. 2019;38:361–75. https://doi.org/10.1080/15513815.2019.1587120.
Fong P, Stafforini DM, Brown NJ, Pretorius M. Increased blood flow induces oxidative stress through an endothelium- and nitric oxide-independent mechanism. Free Radic Biol Med. 2010;49:301–5.
Sena CM, Leandro A, Azul L, Seiça R, Perry G. Vascular oxidative stress: impact and therapeutic approaches. Front Physiol. 2018;9:1668 https://doi.org/10.3389/fphys.2018.01668.
Tikkanen M. Etology, clinical manifestations, and prediction of placental abruption. Acta Obstet Gynecol Scand. 2010;89:732–40.
Buhimschi CS, Schatz F, Krikun G, Buhimschi IA, Lockwood CJ. Novel insights into molecular mechanisms of abruption-induced preterm birth. Expert Rev Mol Med. 2016;12:e35 https://doi.org/10.1017/S1462399410001675.
Cresswell JA, Ronsmans C, Calvert C, Filippi V. Prevalence of placenta previa by world region: a systematic review and meta-analysis. Trop Med Intern Health. 2013;18:712–24.
Ananth CV, Keyes KM, Hamilton A, Gissler M, Wu C, Liu S, et al. An international contrast of rates of placental abruption: an age-period-cohort analysis. PLoS ONE. 2015;10:e0125246 https://doi.org/10.1371/journal.pone.0125246.
Stoltzfus RJ. Iron deficiency: global prevalence and consequences. Food Nutr Bull. 2003;24:S99–S103. 4 Suppl.
Author information
Authors and Affiliations
Contributions
TTL—conceived and designed the study, analysed and interpreted the data, performed the literature search and wrote the manuscript. SYAH—contributed to the design, obtained ethical approval, contributed to data interpretation, literature search, and preparation of the manuscript, approved the manuscript. LLW—assisted in data checking and literature search, contributed to interpretation of the results, and preparation and approval of the manuscript. DSS—set up the database, participated in data analysis and interpretation, contributed to the discussion and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lao, T.Th., Hui, S.Y.A., Wong, L.L. et al. Iron deficiency anaemia associated with increased placenta praevia and placental abruption: a retrospective case-control study. Eur J Clin Nutr 76, 1172–1177 (2022). https://doi.org/10.1038/s41430-022-01086-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01086-6