Abstract
Objectives
To register all symptoms reported by non-anemic menstruating women, and examine the links between these symptoms and iron status parameters available including serum ferritin (SF) in primary care.
Subjects and methods
In this cross-sectional study, we collected clinical and biological data from 780 French menstruating women aged 18–50 years. The data included an anonymous questionnaire (biometric information, physical and cognitive symptoms, reduction in physical performance, current quality of life with SF-36 questionnaire) and seven biological parameters available in primary care. We excluded women with anemia (hemoglobin < 12 g/dl) or chronic disease. Correlations were studied for 554 participants in bivariate analysis (BVA) and multivariate analysis (MVA), with adjusted odds ratio (OR). Receiver operating characteristic (ROC) curves were established for significant correlations in MVA (p < 0.05).
Results
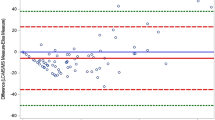
Among these 554 non-anemic women included, 304 (54.9%) had SF level below 50 µg/l, 103 (18.6%) had SF level below 20 µg/l, and 60 (10.8%) had SF level below 15 µg/l. Iron deficiency was significantly correlated with recent hair loss for SF ≤ 15 µg/l (OR = 2.19 with p = 0.02 in MVA) and SF ≤ 20 µg/l (OR = 2.26 with p < 0.01 in MVA). SF ≤ 20 µg/l was also correlated with limitations due to emotional problems according to SF-36 questionnaire (p = 0.01 in MVA). SF ≤ 50 µg/l was significantly correlated with restless legs syndrome (OR = 2.82 with p = 0.01 in MVA). Only one ROC curve for restless legs syndrome could suggest an optimal SF cut-off point at 39 µg/l (sensitivity 73%, specificity 61%).
Conclusion
We identified two symptoms significantly more reported by non-anemic iron-deficient menstruating women: recent hair loss for serum ferritin (SF) ≤ 20 µg/l and restless legs syndrome for SF ≤ 50 µg/l. Non-anemic iron deficiency may also impact their quality of life, but further investigation is needed. If one of these symptoms is reported in primary care, the possibility of a symptomatic iron deficiency cannot be ruled out, and iron supplementation should be considered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
ACC/SCN. Fourth report on the world nutrition situation. Washington, DC: ASS/SCN; 2000.
Galan P, Yoon HC, Preziosi P, Viteri F, Valeix P, Fieux B, et al. Determining factors in the iron status of adult women in the SU.VI.MAX study. Supplementation en vitamines et minéraux antioxydants. Eur J Clin Nutr. 1998;52:383–8.
Hinton PS, Giordano C, Brownlie T, Haas JD. Iron supplementation improves endurance after training in iron-depleted, nonanemic women. J Appl Physiol. 2000;88:1103–11.
Brutsaert TD, Hernandez-Cordero S, Rivera J, Viola T, Hughes G, Haas JD. Iron supplementation improves progressive fatigue resistance during dynamic knee extensor exercise in iron-depleted, nonanemic women. Am J Clin Nutr. 2003;77:441–8.
Crouter SE, DellaValle DM, Haas JD. Relationship between physical activity, physical performance, and iron status in adult women. Appl Physiol Nutr Metab. 2012;37:697–705.
Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet. 1996;348:992–6.
Murray-Kolb LE, Beard JL. Iron treatment normalizes cognitive functioning in young women. Am J Clin Nutr. 2007;85:778–87.
Grondin MA, Ruivard M, Perrève A, Derumeaux-Burel H, Perthus I, Roblin J, et al. Prevalence of iron deficiency and health-related quality of life among female students. J Am Coll Nutr. 2008;27:337–41.
Verdon F, Burnand B, Stubi CL, Bonard C, Graff M, Michaud A, et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ. 2003;326:1124.
Vaucher P, Druais PL, Waldvogel S, Favrat B. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. CMAJ. 2012;184:1247–54.
Favrat B, Balck K, Breymann C, Hedenus M, Keller T, Mezzacasa A, et al. One 1000 mg iron dose of ferric carboxymaltose improved fatigue in iron-deficient, non-anaemic women in the randomised placebo-controlled study PREFER. BJOG. 2012;119:232–3.
Krayenbuehl PA, Battegay E, Breymann C, Furrer J, Schulthess G. Intravenous iron for the treatment of fatigue in nonanemic, premenopausal women with low serum ferritin concentration. Blood. 2011;118:3222–7.
Sharma R, Stanek J, Koch T, Grooms L, O’Brien S. Intravenous iron therapy in non-anemic iron-deficient menstruating adolescent females with fatigue. Am J Hematol. 2016;91:973–7.
Tison F, Crochard A, Leger D, Boue´e S, Lainey E, El, et al. Epidemiology of restless legs syndrome in French adults: A nationwide survey: The INSTANT Study. Neurology. 2005;65:239–46. 26
O′Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–2.
Trenkwalder C, Allen R, Hogl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology. 2016;86:1336–43.
Allen RP, Adler CH, Du W, Butcher A, Bregman DB, Earley CJ. Clinical efficacy and safety of IV ferric carboxymaltose (FCM) treatment of RLS: a multi-centred, placebo-controlled preliminary clinical trial. Sleep Med. 2011;12:906–13.
Trenkwalder C, Winkelmann J, Oertel W, Virgin G, Roubert B, Mezzacasa. Ferric carboxymaltose in patients with restless legs syndrome and nonanemic iron deficiency: a randomized trial. Mov Disord. 2017;32:1478–82.
Vignatelli L, Billiard M, Clarenbach P, Garcia-Borreguero D, Kaynak D, Liesiene V, et al. EFNS guidelines on management of restless legs syndrome and periodic limb movement disorder in sleep. Eur J Neurol. 2006;13:1049–65.
Rushton DH. Nutritional factors and hair loss. Clin Exp Dermatol. 2002;27:396–404.
Trost LB, Bergfeld WF, Calogeras E. The diagnosis and treatment of iron deficiency and its potential relationship to hair loss. J Am Acad Dermatol. 2006;54:824–44.
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372:1832–43.
Author information
Authors and Affiliations
Contributions
JB and MR were responsible for designing the study. JB, CP, and EM were responsible for data collection and management. PB and LG were responsible for statistical analysis. JB and MR were responsible for writing and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Beatrix, J., Piales, C., Berland, P. et al. Non-anemic iron deficiency: correlations between symptoms and iron status parameters. Eur J Clin Nutr 76, 835–840 (2022). https://doi.org/10.1038/s41430-021-01047-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-01047-5