Abstract
Background/objectives
Malnutrition in chronic obstructive pulmonary disease (COPD) patients is prevalent and usually assessed by body mass index (BMI), which can lead to misdiagnosis. The subjective global assessment (SGA) is the reference method for this diagnose in hospitalized patients. In the last decade, new tools have emerged Academy of Nutrition and Dietetics-American Society for Parenteral and Enteral Nutrition [AND-ASPEN], European Society for Clinical Nutrition and Metabolism [ESPEN], and Global Leadership Initiative on Malnutrition [GLIM]). Therefore, this study aimed to assess the concurrent and predictive validity of these tools in acute exacerbated COPD (AECOPD) patients.
Subjects/methods
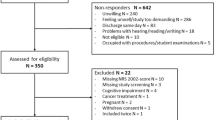
Prospective cohort study with hospitalized AECOPD patients. Malnutrition was diagnosed by SGA (reference method), AND-ASPEN, ESPEN, and GLIM consensus. Hospital length of stay (LOS) and mortality were the outcomes evaluated.
Results
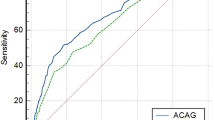
In 241 patients (46.5% males; 68.3 ± 10.2 years), malnutrition was found in 50.0% by SGA, 54.4% by AND-ASPEN, 20.2% by ESPEN, and 47.8% by GLIM. AND-ASPEN had the best accuracy (AUC = 0.837; 95% CI 0.783–0.841) and concordance (kappa = 0.674) with SGA and it was an independent predictor of prolonged LOS (OR = 1.73; 95% CI 1.01–3.37). ESPEN consensus did not agree with SGA, but was associated with prolonged LOS (OR = 2.57 95% CI, 1.27–5.20). The GLIM had good concordance (kappa = 0.533) and accuracy with SGA (AUC = 0.768; 95% CI 0.701–0.835), but was not associated with outcomes.
Conclusions
The AND-ASPEN was the most accurate tool for diagnosing malnutrition in AECOPD patients and was an independent predictor of prolonged LOS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Global Initiative for Chronic Obstructive Lung Disease; Global Strategy for the diagnosis, management and prevention of COPD. (2020 Report). Link: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf. Last access February 2020. Acessed in Mar 2020.
Aaron SD, Donaldson GC, Whitmore GA, Hurst JR, Ramsay T, Wedzicha JA. Time course and pattern of COPD exacerbation onset. Thorax 2012;67:238–43.
Baig MMA, Hashmat N, Adnan M, Rahat T. The relationship of dyspnea and disease severity with anthropometric indicators of malnutrition among patients with chronic obstructive pulmonary disease. Pak J Med Sci. 2018;34:1408–11.
Eriksson B, Backman H, Bossios A, Bjerg A, Hedman L, Lindberg A, et al. Only severe COPD is associated with being underweight: results from a population survey. ERJ Open Res. 2016;2:00051–2015.
Ter Beek L, van der Vaart H, Wempe JB, Krinjnen WP, Roodenburg JLN, van der Schans CP, et al. Coexistence of malnutrition, frailty, physical frailty and disability in patients with COPD starting a pulmonary rehabilitation program. Clin Nutr. 2019;19:33143–7.
Marco E, Sánchez-Rodríguez D, Dávalos-Yerovi VN, Duran X, Pascual EM, Muniesa JM, et al. Malnutrition according to ESPEN consensus predicts hospitalizations and long-term mortality in rehabilitation patients with stable chronic obstructive pulmonary disease. Clin Nutr. 2019;38:2180–6.
de Blasio F, Di Gregorio A, de Blasio F, Bianco A, Bellofiore B, Scalfi L. Malnutrition and sarcopenia assessment in patients with chronic obstructive pulmonary disease according to international diagnostic criteria, and evaluation of raw BIA variables. Respir Med. 2018;134:1–5.
Sami R, Sadegh R, Esmailzadehha N, Mortazian S, Nazem M, Zohal M. Association of Anthropometric Indexes With Disease Severity in Male Patients With Chronic Obstructive Pulmonary Disease in Qazvin, Iran. Am J Mens Health. 2018;12:1023–8.
Hoong JM, Ferguson M, Hukins C, Collins PF. Economic and operational burden associated with malnutrition in chronic obstructive pulmonary disease. Clin Nutr. 2017;36:1105–9.
Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield M, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1–6.
Vermeeren MA, Schols AM, Wouters EF. Effects of an acute exacerbation on nutritional and metabolic profile of patients with COPD. Eur Respir J. 1997;10:2264–9.
Chatila WM, Thomashow BM, Minai OA, Criner GJ, Make BJ. Comorbidities in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5:549–55.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31..
Chen R, Xing L, You C, Ou X. Prediction of prognosis in chronic obstructive pulmonary disease patients with respiratory failure: A comparison of three nutritional assessment methods. Eur J Intern Med. 2018;57:70–5.
Horadagoda C, Dinihan T, Roberts M, Kairaitis K. Body composition and micronutrient deficiencies in patients with an acute exacerbation of chronic obstructive pulmonary disease. Intern Med J. 2017;47:1057–63.
Girón R, Matesanz C, García-Río F, Santiago E, Mancha A, Rodríguez-Salvanés E, et al. Nutritional state during COPD exacerbation: clinical and prognostic implications. Ann Nutr Metab. 2009;54:52–8.
Ranieri P, Bianchetti A, Margiotta A, Virgillo A, Clini EM, Trabucchi M. Predictors of 6-month mortality in elderly patients with mild chronic obstructive pulmonary disease discharged from a medical ward after acute nonacidotic exacerbation. J Am Geriatr Soc. 2008;56:909–13.
Soler-Cataluña JJ, Sánchez-Sánchez L, Martínez-García MA, Sánchez PR, Salcedo E, Navarro M. Mid-arm muscle area is a better predictor of mortality than body mass index in COPD. Chest 2005;128:2108–15.
Soler JJ, Sánchez L, Román P, Martínez MA, Perpiñá M. Prevalence of malnutrition in outpatients with stable chronic obstructive pulmonary disease. Arch Bronconeumol. 2004;40:250–8.
Thorsdottir I, Gunnarsdottir I, Eriksen B. Screening method evaluated by nutritional status measurements can be used to detect malnourishment in chronic obstructive pulmonary disease. J Am Diet Assoc. 2001;101:648–54.
Budweiser S, Meyer K, Jörres R, Heinemann F, Wild PJ, Pfeifer M. Nutritional depletion and its relationship to respiratory impairment in patients with chronic respiratory failure due to COPD or restrictive thoracic diseases. Eur J Clin Nutr. 2008;62:436–43.
Shepherd AB, Bowell K. ‘Mind the gap’: the importance of managing malnutrition in chronic obstructive pulmonary disease. Br J Nurs. 2019;28:1442–9.
Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association Between Malnutrition and Clinical Outcomes in the Intensive Care Unit: A Systematic Review. JPEN J Parenter Enter Nutr. 2017;41:744–58.
Gupta D, Vashi PG, Lammersfeld CA, Braun DP. Role of nutritional status in predicting the length of stay in cancer: a systematic review of the epidemiological literature. Ann Nutr Metab. 2011;59:96–106.
Hogan D, Lan LT, Diep DT, Gallegos D, Collins PF. Nutritional status of Vietnamese outpatients with chronic obstructive pulmonary disease. J Hum Nutr Diet. 2017;30:83–9.
Nguyen HT, Collins PF, Pavey TG, Nguyen NV, Pham TD, Gallegos DL. Nutritional status, dietary intake, and health-related quality of life in outpatients with COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:215–26.
Günay E, Kaymaz D, Selçuk NT, Ergün P, Sengül F, Demir N. Effect of nutritional status in individuals with chronic obstructive pulmonary disease undergoing pulmonary rehabilitation. Respirology. 2013;18:1217–22.
Gupta B, Kant S, Mishra R. Subjective global assessment of nutritional status of chronic obstructive pulmonary disease patients on admission. Int J Tuberc Lung Dis. 2010;14:500–5.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - An ESPEN Consensus Statement. Clin Nutr. 2015;34:335–40.
White JV, Guenter P, Jensen G, Malone A, Schofield M, Academy Malnutrition Work Group; A.S.P.E.N. Malnutrition Task Force. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enter Nutr. 2012;36:275–83.
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle. 2019;10:207–17.
Hipskind P, Rath M, JeVenn A, Galang M, Nawaya A, Smith E, et al. Correlation of New Criteria for Malnutrition Assessment in hospitalized patients: AND-ASPEN versus SGA. J Am Coll Nutr. 2019;39:518–27.
Abahuje E, Niyongombwa I, Karenzi D, Bisimwa JA, Tuyishime E, Ntirenganya F, et al. Malnutrition in acute care surgery patients in Rwanda. World J Surg. 2020;44:1361–7.
Ceniccola GD, Okamura AB, Neta JSS, Lima FC, de Deus ACS, Oliveira JA, et al. Association between AND-ASPEN Malnutrition Criteria and hospital mortality in Critically Ill Trauma Patients: a prospective cohort study. JPEN J Parenter Enter Nutr. 2020;44:1347–54.
Rattanachaiwong S, Zribi B, Kagan I, Theilla M, Heching M, Singer P. Comparison of nutritional screening and diagnostic tools in diagnosis of severe malnutrition in critically ill patients. Clin Nutr. 2020;39:3419–25.
Fink JS, Marcadenti A, Rabito EI, Silva FM. The New European Society for Clinical Nutrition and Metabolism Definition of Malnutrition: Application for Nutrition Assessment and Prediction of Morbimortality in an Emergency Service. JPEN J Parenter Enter Nutr. 2018;42:550–56.
Allard JP, Keller H, Gramlich L, Jeejeebhoy KN, Laporte M, Duerksen DR. GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin Nutr. 2019;39:2771–7.
Beaudart C, Sanchez-Rodriguez D, Locquet M, Reginster JY, Lengelé L, Bruyère O. Malnutrition as a Strong Predictor of the Onset of Sarcopenia. Nutrients. 2019;11:2883.
Burgel CF, Teixeira PP, Leites GM, Carvalho GD, Modanese PVG, Rabito EI, et al. Concurrent and Predictive Validity of AND-ASPEN Malnutrition Consensus Is Satisfactory in Hospitalized Patients: a longitudinal study. JPEN J Parenter Enter Nutr. 2020;45:1061–71.
Bestall J, Paul E, Garrod R, Garnham R, Jones P, Wedzchia J. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–6.
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN. Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enter Nutr. 1984;8:153–9.
Budziareck MB, Pureza Duarte RR, Barbosa-Silva MCG. Reference values and determinants for handgrip strength in healthy subjects. Clin Nutr. 2008;27:357–62.
Fischer M, JeVenn A, Hipskind P. Evaluation of muscle and fat loss as diagnostic criteria for malnutrition. Nutr Clin Pract. 2015;30:239–48.
Gonzalez MC, Orlandi SP, Santos LP, Barros AJD. Body composition using bioelectrical impedance: development and validation of a predictive equation for fat-free mass in a middle-income country. Clin Nutr. 2019;38:2175–9.
Kyle UG, Genton L, Slosman DO, Pichard C. Fat-free and fat mass percentiles in 5225 healthy subjects aged 15 to 98 years. Nutrition. 2001;17:534–41.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, et al. Position of the Academy of Nutrition and Dietetics: Malnutrition (Undernutrition) Screening Tools for All Adults. J Acad Nutr Diet. 2019; pii: S2212-2672: 31366-8.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Perrot L, Greil A, Boirie Y, Farigon N, Mulliez A, Costes F, et al. Prevalence of sarcopenia and malnutrition during acute exacerbation of COPD and after 6 months recovery. Eur J Clin Nutr. 2020;74:1556–64.
Maia I, Peleteiro B, Xará S, Amaral TF. Undernutrition Risk and Undernutrition in Pulmonology Department Inpatients: a Systematic Review and Meta-Analysis. J Am Coll Nutr. 2017;36:137–47.
de van der Schueren MAE, Keller H, GLIM Consortium, Jensen GL, Barazzoni R, Compher C, et al. Global Leadership Initiative on Malnutrition (GLIM): Guidance on validation of the operational criteria for the diagnosis of protein-energy malnutrition in adults. Clin Nutr. 2020;39:2872–80.
Hiller LD, Shaw RF, Fabri PJ. Difference in Composite End Point of Readmission and Death between Malnourished and Non malnourished Veterans assessed using Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition Clinical Characteristics. JPEN J Parenter Enter Nutr. 2017;41:1316–24.
Ingadottir AR, Beck AM, Baldwin C, Weekes CE, Geirsdotti OG, Ramel A, et al. Two components of the new ESPEN diagnostic criteria for malnutrition are independent predictors of lung function in hospitalized patients with chronic obstructive pulmonary disease (COPD). Clin Nutr. 2018;37:1323–31.
Ceniccola GD, Holanda TP, Pequeno RSF, Mendonça VS, Oliveira ABM, Carvalho LSF, et al. Relevance of AND-ASPEN criteria of malnutrition to predict hospital mortality in critically ill patients: a prospective study. J Crit Care. 2018;44:398–403.
Guerra RS, Fonseca I, Pichel F, Restivo MT, Amaral TF. Usefulness of six diagnostic and screening measures for undernutrition in predicting length of hospital stay: a comparative analysis. J Acad Nutr Diet. 2015;115:927–38.
Mosquera C, Koutlas NJ, Edwards KC, Strickland A, Vohra NA, Zervos EE, et al. Impact of malnutrition on gastrointestinal surgical patients. J Surg Res. 2016;205:95–101.
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A. Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections - Results from a National Quality Registry. Clin Nutr. 2019;261:30285–7.
Acknowledgements
We thank Nossa Senhora da Conceição Hospital for supporting the conduct of this study and thank the patients for their participation. We also thank the researchers Paula Portal Teixeira and Kamila Valduga for their valuable assistance during this study. The corresponding author received a productivity scholarship (PQ2) from the Brazilian National Council for Scientific and Technological Development (CNPq).
Author information
Authors and Affiliations
Contributions
FMS and BEA contributed to study conception. BEA, VK and GLM contributed to data acquisition. FMS contributed to data analysis and interpretation. BEA and FMS drafted the paper. All authors critically revised the paper, provided final approval, and agreed to be accountable for all aspects of the work, ensuring its integrity and accuracy.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Araújo, B.E., Kowalski, V., Leites, G.M. et al. AND-ASPEN and ESPEN consensus, and GLIM criteria for malnutrition identification in AECOPD patients: a longitudinal study comparing concurrent and predictive validity. Eur J Clin Nutr 76, 685–692 (2022). https://doi.org/10.1038/s41430-021-01025-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-01025-x