Abstract
Background and Objective
Inconsistent evidence showed that folate supplementation may be associated with reduced risk of cancer due to improved metabolic profiles and reduced markers of oxidative stress and inflammation. The aim of this investigation was to quantify the effects of folate supplementation on the recurrence and other metabolic factors of women with cervical intraepithelial neoplasia grade 2/3 (CIN2/3).
Methods
This randomized, double-blind, placebo-controlled clinical trial was performed among 60 overweight/obese women with CIN2/3. Definitive CIN2/3 confirmation was done via biopsy, pathological diagnosis, as well as colposcopy. Participants were randomly assigned to the intervention group to take 5 mg/day folate supplements or placebo group (n = 30 in each group) for 12 weeks.
Results
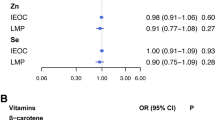
The results of the current study showed a non-significant decrease in recurrence of CIN2/3 in the folate group in comparison with the placebo group (3.3% vs. 16.7%, P = 0.08). Compared with the placebo, folate supplementation significantly decreased plasma homocysteine (Hcy) levels (P < 0.001), serum insulin values (in the crude model) (P = 0.01), and homeostasis model assessment of insulin resistance (P = 0.01). Also, folate supplementation resulted in a significant improvement in the quantitative insulin sensitivity check index (P = 0.002) and total antioxidant capacity (P = 0.04) and a significant reduction in high-sensitivity C-reactive protein (P = 0.015) in comparison with the placebo group.
Conclusions
In conclusion, folate supplementation for 12 weeks among overweight/obese women with CIN2/3 showed a non-significant decrease in its recurrence and had beneficial effects on insulin sensitivity, inflammation, and oxidative stress markers.
Similar content being viewed by others
Introduction
Cervical intraepithelial neoplasia (CIN) is a potential precancerous change and unusual growth of squamous epithelial cells on the ectocervix [1]. CIN2 or CIN3 (high-grade CIN) has the potential to progress to an invasive form of cancer [2]. In 2012, the worldwide prevalence of cervical cancer women and deaths were 528,000 and 266,000, respectively [3]. Various factors including genetics, immune response, and human papillomavirus (HPV)-16 variants are associated with the increased risk of HPV-induced squamous intraepithelial neoplasia conversion to cancerous lesions [4]. In addition, lipid peroxidation, impaired antioxidant system, and elevated inflammatory biomarkers are involved in the pathogenesis of cervical dysplasia [5, 6]. Also, it is shown that obesity has a positive significant association (OR: 1.353, 95%CI: 1.013–1.812; P value = 0.04) with abnormalities in the cervical epithelial cell [7]. The result of a meta-analysis on observational studies has confirmed the positive association between obesity and cervical cancer (OR = 1.40, 95% CI: 1.08, 1.71) [8].
Limited and inconsistent data are available about the beneficial effects of folate administration on CIN recurrence and other metabolic profiles among the involved patients. A previous study has shown that 6-month folate supplementation (5 mg/day) could regress CIN1 and improve homocysteine (Hcy) levels, insulin metabolism, and few markers of inflammation and oxidative stress [9]. In addition, previous studies have reported that folate deficiency and aberrant expression of DNA methyltransferase 1 are associated with an additive effect on cervical cancerization [4, 10]. Folate status and aberrant DNA methylation are also correlated with the natural history of HPV infection [11]. Furthermore, Piyathilake et al. [12] demonstrated that higher circulating folate level was negatively related to high-risk HPV positivity. Following 2.5 mg/day of folate supplementation in overweight subjects for 12 weeks, insulin sensitivity had significant improvement [13]. Also, 5 mg/day folate administration as a B-complex supplement for 14 days in subjects with acute ischemic stroke led to a significant reduction in C-reactive protein (CRP) concentrations [14]. However, folate intake for 12 weeks among participants with atherosclerosis risk factors did not influence inflammatory and lipid parameters [15].
This evidence suggests the importance of folate supplementation due to its anti-inflammatory and antioxidative effects. Based on the author’s knowledge, there is no study assessing the effects of folate supplementation on recurrence, lipid profiles, glycemic indices, inflammation, and oxidative stress markers among involved women with CIN2/3. Therefore, the objective of our study was to evaluate the effects of folate intake on the recurrence and metabolic factors of women with CIN2/3.
Materials and methods
Participants
This investigation was a randomized, double-blind, placebo-controlled parallel clinical trial (registry number in the Iranian registry of clinical trials (http://www.irct.ir: IRCT2017021417639N2); ethical committee number of Isfahan University of Medical Sciences: IR.MUI.REC.1395.3.733), performed in January–October 2017 at an oncology clinic under the supervision of Kashan University of Medical Sciences, Kashan, Iran. Inclusion criteria were folate-deficient women (folate serum levels < 1.8 ng/ml), aged 25–55 years, not pregnant, BMI > 25 kg/m2, no history of smoking, no history of cervical cancer or other cancer of the lower genital tract, with definitive CIN2/3 diagnosed through pathological assessment, colposcopy, and biopsy. According to the available equation for parallel studies, an adequate sample size to determine a significant regression rate percentage (31%) [9] in CIN1 patients (α = 0.05 and β = 20%) was 25 subjects in each group. To consider the potential drop out during the study, 30 participants were recruited for each arm of the study. Exclusion criteria were as follow: starting a destructive therapy of the cervix, diagnosis of chronic diseases like diabetes or immune system disorders such as lupus, any change in the prescribed medication regimen, hysterectomy, pregnancy, and not willing to complete the study.
Study design
Before the start of the study, all women signed written informed consent. Based on inclusion criteria, overweight/obese participants with folate deficiency and CIN2/3 (following loop electrical excision procedure (LEEP) treatment) were enrolled in this study. Researchers matched participants between two groups using age (<35 vs. ≥35 y) and body mass index (BMI) (<30 vs. ≥30 kg/m2) before the start of the study. Participants were randomly assigned to either 5 mg/day folate supplementation (n = 30) or placebo group (n = 30) for 12 weeks by a person who was not a member of the study staff. Randomization was done using a computer-generated random number table. A pharmaceutical company representative coded supplement and placebo to A and B and allocated treatments to two groups using the sealed envelopes. Randomization and allocation were blinded from the investigators and patients until the main analyses were completed. Folate supplement and its placebo were made by Iran Daru Co. (Tehran, Iran) and Barij Essence Co. (Kashan, Iran), respectively. The physical features of the placebo (shape, color, size, and packaging) were completely similar to supplements. The ingredient of each folate supplement was folic acid, microcrystalline cellulose, calcium carbonate, cellulose gel, povidone, citric acid, lactose monohydrate, and magnesium stearate. Placebo contained starch. Measurement of plasma Hcy levels and checking the empty container of medication were used to evaluate the compliance with the folate intake. Participants were asked not to change their usual diet and physical activity during the study. Twenty-four hours dietary recalls were collected at the beginning, middle, and end of the study from all participants. Dietary intakes were analyzed using a modified version of Nutritionist IV software (First Databank, San Bruno, CA) for Iranian food.
Assessment of outcomes
Neoplasia recurrence and metabolic profiles were considered as the primary and secondary endpoint, respectively.
Assessment of primary endpoint
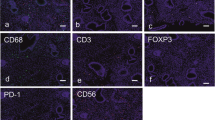
An expert pathologist determined the grade CIN2/3 and its recurrence by pathological diagnosis, colposcopy, and cervical biopsy, at the baseline and end of the intervention.
Secondary outcomes
Secondary outcomes were measured at the baseline and end of the trial. These variables were as follow: anthropometric measurements (height, weight, BMI), glycemic indices (fasting plasma glucose (FPG), insulin levels, homeostatic model of assessment for insulin resistance (HOMA-IR), and the quantitative insulin sensitivity check index (QUICKI)), lipid profiles (triglycerides, very-low-density lipoprotein cholesterol (VLDL-cholesterol), total cholesterol, low-density lipoprotein cholesterol (LDL-cholesterol) and high-density lipoprotein cholesterol (HDL-cholesterol)), inflammatory (high-sensitivity C-reactive protein (hs-CRP)) and oxidative stress markers (nitrite/nitrate (NO), total antioxidant capacity (TAC), total glutathione (GSH) and malondialdehyde (MDA)).
Anthropometric measurements
Weight was measured using a Seca scale without shoes and light clothing nearest to 0.1 kg. Height was measured barefoot using a wall-mounted tape nearest to 0.5 centimeters. BMI was obtained by dividing weight (kg) by height squared (m).
Biochemical assessment
Ten milliliters fasting blood samples were taken at baseline and end-of-trial at Kashan reference laboratory, Kashan, Iran. Plasma Hcy was assessed using an enzyme immunoassay method by Hcy kit (Axis-Shield Diagnostics, UK) with inter- and intra-assay coefficient variances (CVs) of lower than 7%. Commercial kits were used to determine FPG and lipid profiles (Pars Azmun, Tehran, Iran) with inter- and intra-assay CVs lower than 5%. Serum insulin and hs-CRP values were evaluated by ELISA kit (DiaMetra, Milano, Italy and LDN, Nordhorn, Germany) with inter- and intra-assay CVs lower than 5 and 7%, respectively. HOMA-IR and QUICKI were calculated based on suggested formulas [16]. Plasma NO using the Giess method modified by Tatsch et al. [17], TAC by Benzie and Strain method [18], GSH using the method of Beutler et al. [19], and MDA levels by the thiobarbituric acid reactive substance spectrophotometric test [20] were determined with inter- and intra-assay CVs lower than 4%.
Statistical analysis
The distribution of variables was assessed by the Skewness statistics and Kolmogorov-Smirnov test. Logarithmic transformation was run for variables with the abnormal distribution. Leven’s test of equality of error variances was done for all analyses. An independent sample t-test was applied to compare the general characteristics and mean dietary intakes of participants between the two groups. The categorical variable comparison was done using the Pearson Chi-square test. One-way repeated-measures analysis of variance was run to determine the effects of folate supplementation on metabolic profiles. To consider baseline values of variables as a potential confounder, univariate analysis of covariance (ANCOVA) was run. All variables were reported as mean ± standard deviation (SD). A two-tailed P < 0.05 was set as a statistically significant level. All statistical analyses were done using the SPSS 20 (Statistical Package for Social Science version; SPSS Inc., Chicago, Illinois, USA).
Results
All of the variables (except nitric oxide and malondialdehyde) had a normal distribution. Finally, sixty overweight/obese women completed this trial [folate (n = 30) and placebo (n = 30)] (Fig. 1). On average, more than 90% of tablets were taken and no significant side effects were reported following supplementation during the study.
There were no significant differences in the mean of anthropometric measurements at the beginning and end-of-study between the two groups (Table 1). Following the 12-week intervention, a non-significant decrease in recurrence of CIN2/3 was observed in the folate group compared to the placebo group (3.3% vs. 16.7%, P = 0.08).
Regarding the daily dietary intakes of participants, no significant changes were observed between the two groups (Table 2).
Baseline and end values of other biochemical markers are presented in Table 3. Compared with the placebo, folate supplementation significantly decreased Hcy levels of plasma. Also, folate supplementation significantly decreased serum insulin values (just in the crude model), and HOMA-IR, and increased QUICKI compared to the placebo. In addition, a significant elevation in TAC was observed following folate supplementation compared with the placebo. A significant decrease was observed in hs-CRP levels following 12-week of intervention in comparison with the placebo. Other metabolic profiles did not change after folate supplementation compared with the placebo.
Discussion
In the present study, although folate supplementation had beneficial effects on some biochemical markers (insulin metabolism and TAC levels), CIN2/3 recurrence did not change significantly in overweight/obese folate-deficient women. To our knowledge, the effects of folate supplementation on recurrence and metabolic status in patients with CIN2/3 have not been assessed previously.
It is shown that women with CIN2/3 are more prone (in a positive linear trend) to develop cervical cancer [21]. Although we could not document the significant effect of folate supplementation on CIN2/3 recurrence, a non-significant decreasing effect of folate administration on disease recurrence is still of obvious importance. It has previously demonstrated that taking folate at a dosage of 5 mg/day for 6 months in women with CIN1 resulted in its regression [9]. In another study, reduced levels of folate led to increased methylation of microRNA (miR)-203 and miR-375, which in turn participate in significant events during cervical carcinogenesis [22]. It seems that there is a linkage between lower folate levels of serum and increased risk of CIN [23], cervical cancer [10], cell proliferation, and reduced apoptosis in cervical cancer cells [24].
In the present study, folate supplementation significantly decreased serum insulin levels (in the crude model), and HOMA-IR, and significantly increased QUICKI over 12 weeks of intervention in women with CIN2/3 compared to the placebo. However, other biochemical factors including FPG and lipid profiles had no significant changes following folate supplementation. Few studies have shown a positive association between either glycemic load or glycemic index and the risk of endometrial cancer [25, 26]. In a study by Villa et al. [27], it was seen that 7.5 mg/day of folate supplementation for 8 weeks to normo-insulinemic women significantly increased insulin sensitivity, HDL-cholesterol, and improved atherosclerotic indexes including total-/HDL- and LDL-/HDL-cholesterol ratios. Results of a meta-analysis study demonstrated that folate supplementation to people with type 2 diabetes decreased Hcy levels and had an association with better glycemic control in comparison with the placebo [28]. However, 5 mg/day of folate administration had no significant impact on lipid profiles for 4 weeks in cigarette smokers [29]. Insulin resistance due to the elevated levels of sex hormones was proved to play a key role in the diabetes–cancer relationship [30]. Folate supplements may improve insulin metabolism through increased 5′ adenosine monophosphate-activated protein kinase (AMPK) activation [31] and inhibiting insulin-stimulated tyrosine phosphorylation [32].
This study proved that folate supplementation for 12 weeks in women with CIN2/3 significantly increased plasma TAC levels and decreased hs-CRP concentrations. However, folate intake did not influence other oxidative stress markers such as MDA, GSH, and NO compared to the placebo. It has previously proved that taking folate supplements (5 mg/day) for 12 weeks in polycystic ovary syndrome patients declined serum levels of hs-CRP and MDA, and increased plasma levels of TAC and GSH [33]. In addition, combined folate, vitamin B12, and omega-3 supplementation decreased Hcy, MDA, placental tumor necrosis factor-α concentration, and liver MDA in an animal model [34]. Antioxidants administration with B-group vitamins for 90 days in obese diabetic people increased antioxidant capacity and had an anti-inflammatory effect [35]. There is clear evidence that increased inflammatory markers and oxidative stress have an important role in the development of cardiovascular disease (CVD) [36]. Moreover, a large body of evidence confirms the increased levels of inflammation and oxidative stress among subjects with CIN and cervical cancer [37, 38]. Folate through its Hcy-lowering effects and antioxidant properties can reduce oxidative damage and as a consequence CVD risk [39, 40]. Less production of parathyroid hormone [40] and decreased activity of nuclear factor kappa B (NF-κB) [41] following folate supplementation may result in decreased inflammation and oxidative stress.
The strengths of the current study are as follow: (1) randomized, double-blind, placebo-controlled nature of this study was the best design to answer interesting questions including CIN2/3 recurrence; (2) a non-significant decreased recurrence in the folate group was found in this study. However, this finding needs to be confirmed in larger clinical trials. Our findings had some limitations too. Due to budget limitations, we could not assess the effects of folate supplementation on HPV, plasma folate levels, and signaling pathways related to inflammation and oxidative stress in women with CIN2/3. Our calculated sample size which was based on the effect of folate supplementation on the CIN 1 regression was not large enough to detect the potential effect of folate administration on CIN2/3 regression. This study was performed among folate-deficient, overweight/obese women with definitive CIN2/3 diagnosis. Therefore, the final results of folate intervention on cancer regression, metabolic, inflammatory, and oxidative stress markers can only be generalized to a similar population to the current study.
In conclusion, folate supplementation in overweight/obese folate-deficient women with CIN2/3 for 12 weeks demonstrated a non-significant decrease in its recurrence and improved insulin metabolism and TAC levels. More clinical trials should be performed to affirm the findings of the current study.
References
Uuskula A, Raag M, Uppin A, Raud T, Klaar U, Jurisson M, et al. Incidence of cervical intraepithelial neoplasia in Estonia. J Low Genit Trac Dis. 2013;17:129–36.
Jordan J, Martin-Hirsch P, Arbyn M, Schenck U, Baldauf JJ, Da Silva D, et al. European guidelines for clinical management of abnormal cervical cytology, part 2. Cytopathology. 2009;20:5–16.
McGuire S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press; 2015. Adv Nutr. 2016;7:418–9.
Pathak S, Bajpai D, Banerjee A, Bhatla N, Jain SK, Jayaram HN, et al. Serum one-carbon metabolites and risk of cervical cancer. Nutr Cancer. 2014;66:818–24.
Kim SY, Kim JW, Ko YS, Koo JE, Chung HY, Lee-Kim YC. Changes in lipid peroxidation and antioxidant trace elements in serum of women with cervical intraepithelial neoplasia and invasive cancer. Nutr Cancer. 2003;47:126–30.
Carrero Y, Mosquera J, Callejas D, Alvarez-Mon M. In situ increased chemokine expression in human cervical intraepithelial neoplasia. Pathol Res Pract. 2015;211:281–5.
Okoro SO, Ajah LO, Nkwo PO, Aniebue UU, Ozumba BC, Chigbu CO. Association between obesity and abnormal Papanicolau(Pap) smear cytology results in a resource-poor Nigerian setting. BMC Women’s Health. 2020;20:119.
Poorolajal J, Jenabi E. The association between BMI and cervical cancer risk: a meta-analysis. Eur J Cancer Prev. 2016;25:232–8.
Asemi Z, Vahedpoor Z, Jamilian M, Bahmani F, Esmaillzadeh A. Effects of long-term folate supplementation on metabolic status and regression of cervical intraepithelial neoplasia: a randomized, double-blind, placebo-controlled trial. Nutrition. 2016;32:681–6.
Wang JT, Ding L, Jiang SW, Hao J, Zhao WM, Zhou Q, et al. Folate deficiency and aberrant expression of DNA methyltransferase 1 were associated with cervical cancerization. Curr Pharm Des. 2014;20:1639–46.
Flatley JE, McNeir K, Balasubramani L, Tidy J, Stuart EL, Young TA, et al. Folate status and aberrant DNA methylation are associated with HPV infection and cervical pathogenesis. Cancer Epidemiol Biomark Prev. 2009;18:2782–9.
Piyathilake CJ, Henao OL, Macaluso M, Cornwell PE, Meleth S, Heimburger DC, et al. Folate is associated with the natural history of high-risk human papillomaviruses. Cancer Res. 2004;64:8788–93.
Solini A, Santini E, Ferrannini E. Effect of short-term folic acid supplementation on insulin sensitivity and inflammatory markers in overweight subjects. Int J Obes. 2006;30:1197–202.
Ullegaddi R, Powers HJ, Gariballa SE. Antioxidant supplementation with or without B-group vitamins after acute ischemic stroke: a randomized controlled trial. J Parenter Enter Nutr. 2006;30:108–14.
Mierzecki A, Makarewicz-Wujec M, Kloda K, Kozlowska-Wojciechowska M, Pienkowski P, Naruszewicz M. Influence of folic acid supplementation on coagulation, inflammatory, lipid, and kidney function parameters in subjects with low and moderate content of folic acid in the diet. Kardiol Pol. 2015;73:280–6.
Pisprasert V, Ingram KH, Lopez-Davila MF, Munoz AJ, Garvey WT. Limitations in the Use of Indices Using Glucose and Insulin Levels to Predict Insulin Sensitivity: Impact of Race and Gender and Superiority of the Indices Derived from Oral Glucose Tolerance Test in African Americans. Diabetes Care. 2013;36:845–53.
Tatsch E, Bochi GV, Pereira Rda S, Kober H, Agertt VA, de Campos MM, et al. A simple and inexpensive automated technique for measurement of serum nitrite/nitrate. Clin Biochem. 2011;44:348–50.
Benzie IF, Strain JJ. The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem. 1996;239:70–6.
Beutler E, Gelbart T. Plasma glutathione in health and in patients with malignant disease. J Lab Clin Med. 1985;105:581–4.
Janero DR. Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic Biol Med. 1990;9:515–40.
Agorastos T, Miliaras D, Lambropoulos AF, Chrisafi S, Kotsis A, Manthos A, et al. Detection and typing of human papillomavirus DNA in uterine cervices with coexistent grade I and grade III intraepithelial neoplasia: biologic progression or independent lesions? Eur J Obstet Gynecol Reprod Biol. 2005;121:99–103.
Hao M, Zhao W, Zhang L, Wang H, Yang X. Low folate levels are associated with methylation-mediated transcriptional repression of miR-203 and miR-375 during cervical carcinogenesis. Oncol Lett. 2016;11:3863–9.
Zhao W, Hao M, Wang Y, Feng N, Wang Z, Wang W, et al. Association between folate status and cervical intraepithelial neoplasia. Eur J Clin Nutr. 2016;70:837–42.
Ding L, Ma J, Zhou Q, Wang J. [Effect of folate on the proliferation of human cervical cancer cell and relationship with HPV16]. Wei Sheng Yan Jiu. 2013;42:748–53.
Silvera SA, Rohan TE, Jain M, Terry PD, Howe GR, Miller AB. Glycaemic index, glycaemic load and risk of endometrial cancer: a prospective cohort study. Public Health Nutr. 2005;8:912–9.
Larsson SC, Friberg E, Wolk A. Carbohydrate intake, glycemic index and glycemic load in relation to risk of endometrial cancer: a prospective study of Swedish women. Int J Cancer. 2007;120:1103–7.
Villa P, Perri C, Suriano R, Cucinelli F, Panunzi S, Ranieri M, et al. L-folic acid supplementation in healthy postmenopausal women: effect on homocysteine and glycolipid metabolism. J Clin Endocrinol Metab. 2005;90:4622–9.
Sudchada P, Saokaew S, Sridetch S, Incampa S, Jaiyen S, Khaithong W. Effect of folic acid supplementation on plasma total homocysteine levels and glycemic control in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2012;98:151–8.
O’Grady HL, Leahy A, McCormick PH, Fitzgerald P, Kelly CK, Bouchier-Hayes DJ. Oral folic acid improves endothelial dysfunction in cigarette smokers. J Surg Res. 2002;106:342–5.
Sun W, Lu J, Wu S, Bi Y, Mu Y, Zhao J, et al. Association of insulin resistance with breast, ovarian, endometrial and cervical cancers in non-diabetic women. Am J Cancer Res. 2016;6:2334–44.
Buettner R, Bettermann I, Hechtl C, Gabele E, Hellerbrand C, Scholmerich J, et al. Dietary folic acid activates AMPK and improves insulin resistance and hepatic inflammation in dietary rodent models of the metabolic syndrome. Horm Metab Res. 2010;42:769–74.
Marcucci R, Zanazzi M, Bertoni E, Rosati A, Fedi S, Lenti M, et al. Vitamin supplementation reduces the progression of atherosclerosis in hyperhomocysteinemic renal-transplant recipients. Transplantation. 2003;75:1551–5.
Bahmani F, Karamali M, Shakeri H, Asemi Z. The effects of folate supplementation on inflammatory factors and biomarkers of oxidative stress in overweight and obese women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled clinical trial. Clin Endocrinol. 2014;81:582–7.
Kemse NG, Kale AA, Joshi SR. A combined supplementation of omega-3 fatty acids and micronutrients (folic acid, vitamin B12) reduces oxidative stress markers in a rat model of pregnancy induced hypertension. PLoS ONE. 2014;9:e111902 https://doi.org/10.1371/journal.pone.0111902
Gariballa S, Afandi B, Abuhaltem M, Yassin J, Habib H, Ibrahim W. Oxidative damage and inflammation in obese diabetic Emirati subjects supplemented with antioxidants and B-vitamins: a randomized placebo-controlled trail. Nutr Metab. 2013;10:21 https://doi.org/10.1186/1743-7075-10-21
He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006;367:320–6.
Tong SY, Lee JM, Song ES, Lee KB, Kim MK, Lee JK, et al. Functional polymorphism in manganese superoxide dismutase and antioxidant status: their interactions on the risk of cervical intraepithelial neoplasia and cervical cancer. Gynecol Oncol. 2009;115:272–6.
de Castro-Sobrinho JM, Rabelo-Santos SH, Fugueiredo-Alves RR, Derchain S, Sarian LO, Pitta DR, et al. Bacterial vaginosis and inflammatory response showed association with severity of cervical neoplasia in HPV-positive women. Diagn Cytopathol. 2016;44:80–6.
Brattstrom L, Wilcken DE. Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr. 2000;72:315–23.
Zhao G, Ford ES, Li C. Associations of serum concentrations of 25-hydroxyvitamin D and parathyroid hormone with surrogate markers of insulin resistance among U.S. adults without physician-diagnosed diabetes: NHANES, 2003-2006. Diabetes Care. 2010;33:344–7.
Papatheodorou L, Weiss N. Vascular oxidant stress and inflammation in hyperhomocysteinemia. Antioxid Redox Signal. 2007;9:1941–58.
Acknowledgements
The present study was supported by Isfahan University of Medical Sciences, Isfahan, Iran (No. 395733). The sponsor had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SS was involved in conceptualization, methodology, software, validation, formal analysis, data curation, writing the original draft. ZV was responsible for performing investigation, and data curation. SSB was contributed in writing the original draft of the paper, review & editing the final manuscript. MN was responsible for conceptualization, methodology, writing the original draft, review & editing the final manuscript, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sabihi, S., Vahedpoor, Z., Saraf-Bank, S. et al. Effects of folate supplementation on recurrence and metabolic status of cervical intraepithelial neoplasia grade 2/3 in overweight and obese women: a randomized double-blind placebo-controlled trial. Eur J Clin Nutr 76, 666–670 (2022). https://doi.org/10.1038/s41430-021-01022-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-01022-0