Abstract
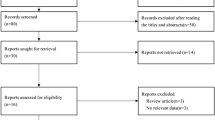
In order to evaluate the predictive effect of the controlled nutritional status (CONUT) score on the prognosis of patients with renal cell carcinoma (RCC) and upper urinary tract urothelial carcinoma (UTUC), a meta-analysis was performed. This systematic review has been registered on PROSPERO, the registration ID is CRD42021251879. A systematic search of the published literature using PubMed, Web of Science, Cochrane Library, EMBASE, and MEDLINE was performed. The fields of “renal cell cancer,” “upper tract urothelial cancer,” and “controlling nutritional status” and other fields were used as search terms. STATA 16 software was used to carry out data merging and statistical analysis of binary variables, Q test and χ2 tests were used to verify the heterogeneity between the included works of studies. Subgroup analysis and sensitivity analysis were used to explain the sources of heterogeneity between studies. Begg’s test was used to assess publication bias between studies. From the first 542 studies retrieved, through strict inclusion and exclusion criteria, 7 studies finally met the requirements and were included in the meta-analysis. Pooled results indicated that high CONUT indicates worse over survival (OS) [HR = 1.70, 95% CI (1.43–2.03), P = 0.02], cancer-specific survival (CSS) [HR = 1.84, 95% CI (1.52–2.23), P = 0.01], recurrence-free survival (RFS) [HR = 1.60, 95% CI (1.26–2.03), P = 0.116], and disease-free survival (DFS) [HR = 1.47, 95% CI (1.20–1.81), P = 0.03]. Based on cancer type, cutoff value, region, and sample size, a subgroup analysis was performed. The results showed that OS and CSS were not affected by the above factors, and the high CONUT score before surgery predicted worse OS and CSS. In conclusion, this meta-analysis revealed that the preoperative CONUT score is a potential independent predictor of the postoperative prognosis of RCC/UTUC patients. A high CONUT predicts worse OS/CSS/DFS and RFS in patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article.
References
Shuch B, Amin A, Armstrong AJ, Eble JN, Ficarra V, Lopez-Beltran A, et al. Understanding pathologic variants of renal cell carcinoma: distilling therapeutic opportunities from biologic complexity. Eur Urol. 2015;67:85–97. https://doi.org/10.1016/j.eururo.2014.04.029.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Kang B, Sun C, Gu H, Yang S, Yuan X, Ji C, et al. T1 stage clear cell renal cell carcinoma: a CT-based radiomics nomogram to estimate the risk of recurrence and metastasis. Front Oncol. 2020;10:579619 https://doi.org/10.3389/fonc.2020.579619.
Park YH, Baik KD, Lee YJ, Ku JH, Kim HH, Kwak C. Late recurrence of renal cell carcinoma >5 years after surgery: clinicopathological characteristics and prognosis. BJU Int. 2012;110(11 Pt B):E553–8. https://doi.org/10.1111/j.1464-410X.2012.11246.x.
Elghiaty A, Kim J, Jang WS, Park JS, Heo JE, Rha KH, et al. Preoperative controlling nutritional status (CONUT) score as a novel immune-nutritional predictor of survival in non-metastatic clear cell renal cell carcinoma of ≤7 cm on preoperative imaging. J Cancer Res Clin Oncol. 2019;145:957–65. https://doi.org/10.1007/s00432-019-02846-x.
Petros FG. Epidemiology, clinical presentation, and evaluation of upper-tract urothelial carcinoma. Transl Androl Urol. 2020;9:1794–8. https://doi.org/10.21037/tau.2019.11.22.
Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, et al. European Association of Urology Guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol. 2021;79:62–79. https://doi.org/10.1016/j.eururo.2020.05.042.
Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester RJ, Burger M, et al. European Association of Urology Guidelines on upper urinary tract urothelial carcinoma: 2017 update. Eur Urol. 2018;73:111–22. https://doi.org/10.1016/j.eururo.2017.07.036.
Su X, Lu X, Bazai SK, Compérat E, Mouawad R, Yao H, et al. Comprehensive integrative profiling of upper tract urothelial carcinomas. Genome Biol. 2021;22:7 https://doi.org/10.1186/s13059-020-02230-w.
Owens B. Kidney cancer. Nature. 2016;537:S97 https://doi.org/10.1038/537S97a.
Turajlic S, Swanton C, Boshoff C. Kidney cancer: the next decade. J Exp Med. 2018;215:2477–9. https://doi.org/10.1084/jem.20181617.
Kutikov A, Egleston BL, Wong YN, Uzzo RG. Evaluating overall survival and competing risks of death in patients with localized renal cell carcinoma using a comprehensive nomogram. J Clin Oncol. 2010;28:311–7. https://doi.org/10.1200/jco.2009.22.4816.
Costa-Pinheiro P, Montezuma D, Henrique R, Jerónimo C. Diagnostic and prognostic epigenetic biomarkers in cancer. Epigenomics. 2015;7:1003–15. https://doi.org/10.2217/epi.15.56.
Liang RF, Li JH, Li M, Yang Y, Liu YH. The prognostic role of controlling nutritional status scores in patients with solid tumors. Clin Chim Acta. 2017;474:155–8. https://doi.org/10.1016/j.cca.2017.09.021.
Linehan WM, Ricketts CJ. The metabolic basis of kidney cancer. Semin Cancer Biol. 2013;23:46–55. https://doi.org/10.1016/j.semcancer.2012.06.002.
Lee HY, Tang JH, Chen YH, Wu WJ, Juan YS, Li WM, et al. The metabolic syndrome is associated with the risk of urothelial carcinoma from a health examination database. Int J Clin Oncol. 2021;26:569–77. https://doi.org/10.1007/s10147-020-01834-3.
Kim HL, Han KR, Zisman A, Figlin RA, Belldegrun AS. Cachexia-like symptoms predict a worse prognosis in localized t1 renal cell carcinoma. J Urol. 2004;171:1810–3. https://doi.org/10.1097/01.ju.0000121440.82581.d3.
Galdiero MR, Marone G, Mantovani A. Cancer inflammation and cytokines. Cold Spring Harb Perspect Biol. 2018;10:a028662. https://doi.org/10.1101/cshperspect.a028662.
Harimoto N, Yoshizumi T, Inokuchi S, Itoh S, Adachi E, Ikeda Y, et al. Prognostic significance of preoperative controlling nutritional status (CONUT) score in patients undergoing hepatic resection for hepatocellular carcinoma: a multi-institutional study. Ann surgical Oncol. 2018;25:3316–23. https://doi.org/10.1245/s10434-018-6672-6.
Itami Y, Miyake M, Tatsumi Y, Gotoh D, Hori S, Morizawa Y, et al. Preoperative predictive factors focused on inflammation-, nutrition-, and muscle-status in patients with upper urinary tract urothelial carcinoma undergoing nephroureterectomy. Int J Clin Oncol. 2019;24:533–45. https://doi.org/10.1007/s10147-018-01381-y.
Ahiko Y, Shida D, Horie T, Tanabe T, Takamizawa Y, Sakamoto R, et al. Controlling nutritional status (CONUT) score as a preoperative risk assessment index for older patients with colorectal cancer. BMC Cancer. 2019;19:946. https://doi.org/10.1186/s12885-019-6218-8.
Kuroda D, Sawayama H, Kurashige J, Iwatsuki M, Eto T, Tokunaga R, et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer. 2018;21:204–12. https://doi.org/10.1007/s10120-017-0744-3.
Niu X, Zhu Z, Bao J. Prognostic significance of pretreatment controlling nutritional status score in urological cancers: a systematic review and meta-analysis. Cancer Cell Int. 2021;21:126 https://doi.org/10.1186/s12935-021-01813-2.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle Ottawa 1 Scale (NOS) for assessing the quality of nonrandomized studies in metaanalyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–34. 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8.
Le Chevalier T, Scagliotti G, Natale R, Danson S, Rosell R, Stahel R, et al. Efficacy of gemcitabine plus platinum chemotherapy compared with other platinum containing regimens in advanced non-small-cell lung cancer: a meta-analysis of survival outcomes. Lung Cancer. 2005;47:69–80. https://doi.org/10.1016/j.lungcan.2004.10.014.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.
Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37:1148–57. https://doi.org/10.1093/ije/dyn065.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74:785–94. https://doi.org/10.1111/biom.12817.
Bao Z, Li Y, Guan B, Xiong G, Zhang L, Tang Q, et al. High preoperative controlling nutritional status score predicts a poor prognosis in patients with localized upper tract urothelial cancer: a propensity score matching study in a large chinese center. Cancer Manag Res. 2020;12:323–35. https://doi.org/10.2147/cmar.S225711.
Ishihara H, Kondo T, Yoshida K, Omae K, Takagi T, Iizuka J, et al. Preoperative controlling nutritional status (CONUT) score as a novel predictive biomarker of survival in patients with localized urothelial carcinoma of the upper urinary tract treated with radical nephroureterectomy. Urologic Oncol. 2017;35:539.e539–539.e516. https://doi.org/10.1016/j.urolonc.2017.04.012.
Kang HW, Seo SP, Kim WT, Yun SJ, Lee SC, Kim WJ, et al. Prognostic impact of nutritional status assessed by the controlling nutritional status (CONUT) score in patients with surgically treated renal cell carcinoma. Nutr Cancer. 2018;70:886–94. https://doi.org/10.1080/01635581.2018.1490448.
Song H, Xu B, Luo C, Zhang Z, Ma B, Jin J, et al. The prognostic value of preoperative controlling nutritional status score in non-metastatic renal cell carcinoma treated with surgery: a retrospective single-institution study. Cancer Manag Res. 2019;11:7567–75. https://doi.org/10.2147/cmar.S209418.
Xu H, Tan P, Jin X, Ai J, Lin T, Lei H, et al. Validation of the preoperative controlling nutritional status score as an independent predictor in a large Chinese cohort of patients with upper tract urothelial carcinoma. Cancer Med. 2018;7:6112–23. https://doi.org/10.1002/cam4.1902.
Zheng Y, Bao L, Wang W, Wang Q, Pan Y, Gao X. Prognostic impact of the Controlling Nutritional Status score following curative nephrectomy for patients with renal cell carcinoma. Medicine. 2018;97:e13409 https://doi.org/10.1097/md.0000000000013409.
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Wang J, Liu Y, Mi X, Shao M, Liu L. The prognostic value of prognostic nutritional index (PNI) and neutrophil to lymphocyte ratio (NLR) for advanced non-small cell lung cancer treated with platinum-based chemotherapeutics. Ann Palliat Med. 2020;9:967–78. https://doi.org/10.21037/apm.2020.04.31.
Mao YS, Hao SJ, Zou CF, Xie ZB, Fu DL. Controlling Nutritional Status score is superior to Prognostic Nutritional Index score in predicting survival and complications in pancreatic ductal adenocarcinoma: a Chinese propensity score matching study. Br J Nutr. 2020;124:1190–7. https://doi.org/10.1017/s0007114520002299.
Yang C, Wei C, Wang S, Han S, Shi D, Zhang C, et al. Combined features based on preoperative controlling nutritional status score and circulating tumour cell status predict prognosis for colorectal cancer patients treated with curative resection. Int J Biol Sci. 2019;15:1325–35. https://doi.org/10.7150/ijbs.33671.
Yılmaz A, Tekin SB, Bilici M, Yılmaz H. The significance of controlling nutritional status (CONUT) score as a novel prognostic parameter in small cell. Lung Cancer Lung. 2020;198:695–704. https://doi.org/10.1007/s00408-020-00361-2.
Akabane M, Shindoh J, Kobayashi Y, Umino R, Kojima K, Okubo S, et al. Significance of preoperative nutritional status as a predictor for short-term and long-term outcomes of patients undergoing surgery for stage IV colorectal cancer. Langenbecks Arch Surg. 2021. https://doi.org/10.1007/s00423-021-02255-0. Online ahead of print.
Müller L, Hahn F, Mähringer-Kunz A, Stoehr F, Gairing SJ, Foerster F, et al. Immunonutritive scoring in patients with hepatocellular carcinoma undergoing transarterial chemoembolization: prognostic nutritional index or controlling nutritional status score? Front Oncol. 2021;11:696183 https://doi.org/10.3389/fonc.2021.696183.
Zhang G, Zhang Y, He F, Wu H, Wang C, Fu C. Preoperative controlling nutritional status (CONUT) score is a prognostic factor for early-stage cervical cancer patients with high-risk factors. Gynecol Oncol. 2021;162:763–9. https://doi.org/10.1016/j.ygyno.2021.06.012.
López Espuela F, Roncero-Martín R, Zamorano JDP, Rey-Sanchez P, Aliaga-Vera I, Portilla Cuenca JC, et al. Controlling Nutritional Status (CONUT) score as a predictor of all-cause mortality at 3 months in stroke patients. Biol Res Nurs. 2019;21:564–70. https://doi.org/10.1177/1099800419860253.
Liu J, Wang F, Li S, Huang W, Jia Y, Wei C. The prognostic significance of preoperative serum albumin in urothelial carcinoma: a systematic review and meta-analysis. Biosci Rep. 2018;38:BSR20180214. https://doi.org/10.1042/bsr20180214.
Sheth KR, Haddad AQ, Ashorobi OS, Meissner MA, Sagalowsky AI, Lotan Y, et al. Prognostic serum markers in patients with high-grade upper tract urothelial carcinoma. Urologic Oncol. 2016;34:418.e419–418.e416. https://doi.org/10.1016/j.urolonc.2016.04.009.
Rossi JF, Lu ZY, Jourdan M, Klein B. Interleukin-6 as a therapeutic target. Clin Cancer Res. 2015;21:1248–57. https://doi.org/10.1158/1078-0432.Ccr-14-2291.
Bekos C, Polterauer S, Seebacher V, Bartl T, Joura E, Reinthaller A, et al. Pre-operative hypoalbuminemia is associated with complication rate and overall survival in patients with vulvar cancer undergoing surgery. Arch Gynecol Obstet. 2019;300:1015–22. https://doi.org/10.1007/s00404-019-05278-7.
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39:534–40. https://doi.org/10.1016/j.ctrv.2012.08.003.
Omura S, Taguchi S, Miyagawa S, Matsumoto R, Samejima M, Ninomiya N, et al. Prognostic significance of the albumin-to-globulin ratio for upper tract urothelial carcinoma. BMC Urol. 2020;20:133 https://doi.org/10.1186/s12894-020-00700-8.
Tanriverdi O. A discussion of serum albumin level in advanced-stage hepatocellular carcinoma: a medical oncologist’s perspective. Med Oncol. 2014;31:282 https://doi.org/10.1007/s12032-014-0282-3.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69 https://doi.org/10.1186/1475-2891-9-69.
Silvente-Poirot S, Poirot M. Cancer. Cholesterol and cancer, in the balance. Science. 2014;343:1445–6. https://doi.org/10.1126/science.1252787.
Heilos D, Röhrl C, Pirker C, Englinger B, Baier D, Mohr T, et al. Altered membrane rigidity via enhanced endogenous cholesterol synthesis drives cancer cell resistance to destruxins. Oncotarget. 2018;9:25661–80. https://doi.org/10.18632/oncotarget.25432.
Zhang J, Li Q, Wu Y, Wang D, Xu L, Zhang Y, et al. Cholesterol content in cell membrane maintains surface levels of ErbB2 and confers a therapeutic vulnerability in ErbB2-positive breast cancer. Cell Commun Signal. 2019;17:15 https://doi.org/10.1186/s12964-019-0328-4.
Sung HH, Jeon HG, Jeong BC, Seo SI, Jeon SS, Choi HY, et al. Clinical significance of prognosis using the neutrophil-lymphocyte ratio and erythrocyte sedimentation rate in patients undergoing radical nephroureterectomy for upper urinary tract urothelial carcinoma. BJU Int. 2015;115:587–94. https://doi.org/10.1111/bju.12846.
Farhood B, Najafi M, Mortezaee K. CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: a review. J Cell Physiol. 2019;234:8509–21. https://doi.org/10.1002/jcp.27782.
Yap SA, Schupp CW, Chamie K, Evans CP, Koppie TM. Effect of age on transitional cell carcinoma of the upper urinary tract: presentation, treatment, and outcomes. Urology. 2011;78:87–92. https://doi.org/10.1016/j.urology.2011.03.032.
Znaor A, Lortet-Tieulent J, Laversanne M, Jemal A, Bray F. International variations and trends in renal cell carcinoma incidence and mortality. Eur Urol. 2015;67:519–30. https://doi.org/10.1016/j.eururo.2014.10.002.
Panian J, Lin X, Simantov R, Derweesh I, Choueiri TK, McKay RR. The impact of age and gender on outcomes of patients with advanced renal cell carcinoma treated with targeted therapy. Clin Genitourin Cancer. 2020;18:e598–e609. https://doi.org/10.1016/j.clgc.2020.03.010.
Nakagomi A, Kohashi K, Morisawa T, Kosugi M, Endoh I, Kusama Y, et al. Nutritional status is associated with inflammation and predicts a poor outcome in patients with chronic heart failure. J Atheroscler Thromb. 2016;23:713–27. https://doi.org/10.5551/jat.31526.
Wada H, Dohi T, Miyauchi K, Endo H, Tsuboi S, Ogita M, et al. Combined effect of nutritional status on long-term outcomes in patients with coronary artery disease undergoing percutaneous coronary intervention. Heart Vessels. 2018;33:1445–52. https://doi.org/10.1007/s00380-018-1201-x.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Acknowledgements
The author thanks Dr. Yunxiang Li for the funding support and technical route planning for this research.
Funding
This work was supported by the Sichuan Province Science and Technology Planning Project under Grant number 2020YFS0320 and Sichuan Provincial Health Committee Research Project under Grant number 20PJ305.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: YL and DC. Analyzed the data: LP, JL, and CM. Manuscript proofreading/grammar revision: CY, YD, WX, and ZX. Wrote the manuscript: LP and JL. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, L., Meng, C., Li, J. et al. The prognostic significance of controlling nutritional status (CONUT) score for surgically treated renal cell cancer and upper urinary tract urothelial cancer: a systematic review and meta-analysis. Eur J Clin Nutr 76, 801–810 (2022). https://doi.org/10.1038/s41430-021-01014-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-01014-0
This article is cited by
-
Prognostic and clinicopathological impacts of Controlling Nutritional Status (CONUT) score on patients with gynecological cancer: a meta-analysis
Nutrition Journal (2023)
-
Low prognostic nutritional index is associated with poor outcome in middle-aged and elderly patients with non-metastatic nasopharyngeal carcinoma: a retrospective cohort study
Supportive Care in Cancer (2022)