Abstract
Objective
To examine trends and projections of underweight (Body Mass Index, BMI < 18.5 kg/m2) and overweight (BMI ≥ 25.0 kg/m2) in women of reproductive age in 55 low- and middle-income countries (LMICs).
Methods
We used data from 2,337,855 women aged 15–49 years from nationally representative Demographic and Health Survey conducted between 1990 and 2018. Bayesian linear regression analyses were performed.
Results
During 1990–2018, the prevalence of underweight decreased in 35 countries and overweight increased in 50 countries. The highest underweight increase was in Morocco (5.5%) and overweight in Nepal (12.4%). In 2030, >20% of women in eight LMICs will be underweight, with Madagascar (36.8%), Senegal (32.2%), and Burundi (29.2%) projected to experience the highest burden of underweight. Whereas >50% of women in 22 LMICs are projected to be overweight, with Egypt (94.7%), Jordan (75.0%), and Pakistan (74.1%) projected to have the highest burden of overweight. 24 LMICs are projected to experience the double burden of malnutrition (both underweight and overweight >20%) in 2030. Noticeable variations in underweight and overweight were observed across wealth, residence, education, and age of women, with a higher rate of overweight in high-income, high-education, and urban women. These inequalities have widened in many countries and are projected to continue. The probability of eradicating overweight and underweight is nearly 0% for all countries by 2030, except Egypt is on track to eradicate underweight.
Conclusions
Although the prevalence of underweight declined, this decline has been superseded by the dramatic increase of overweight. None of the 55 LMICs is likely to eradicate malnutrition in women by 2030.
Similar content being viewed by others
Introduction
The double burden of malnutrition (DBM), characterized by the coexistence of both undernutrition and overweight/obesity, among women of reproductive age continues as a major public health problem worldwide. At the population level, women’s DBM is defined as the concurrent high prevalence of underweight and overweight/obesity at the same time [1]. Women of reproductive age group are particularly important in facing the DBM paradox and are the host of continuing this paradox during the life course by generating malnourished birth outcome [2,3,4]. Also, underweight women are at increased risk of experiencing cardiovascular diseases (CVD) including stroke, heart attack, and coronary artery disease [5]. Women who are overweight/obese are at greater long-term risks of experiencing CVD, chronic kidney diseases, some cancers, and musculoskeletal disorders [6,7,8,9,10,11,12], resulting in three million global deaths annually [7, 10, 11, 13, 14].
High rates of underweight among women have been a major public health concern in LMICs for several decades. However, growing urbanization and globalization in LMICs and associated lifestyle and behavioural changes led to a significant shift in epidemiological trend from underweight to overweight [15] and nutritional transitions [16] that further affected health, including CVD and diabetes pandemic [17, 18]. Concerning the burden of overweight, the global non-communicable disease targets highlighted to halt the rise of obesity prevalence at the level of 2010 [19, 20]. Concurrently, eradicating all forms of malnutrition is an integral component of the global agenda for Sustainable Development Goals 2 (SDG-2) [21].
Evidence showed growing rates of overweight and obesity in women from South and Southeast Asian countries [22], and geographical variations in these burdens in India [23]. However, these inadequate shreds of evidence affect the outlining and planning of future initiatives for reducing the DBM. The recent Lancet series on the DBM highlighted the dynamics of the DBM, its health consequences and economic burden, and seizing opportunities to address malnutrition [24,25,26,27]. However, identifying populations who are at greater risk of suffering from the DBM is limited in the literature to further guide policy makers in addressing this burden.
In this study, we examined trends and projections of underweight and overweight in women at the national level and across subpopulations regarding the important determinants, e.g., wealth, place of residence, education, and age of women in LMICs.
Materials and methods
Data
We used large-scale, nationally representative repeated cross-sectional data from the Demographic and Health Surveys (DHS) [28] conducted between 1990 and 2018. A total of 55 countries surveyed at least twice, with 192 surveys, were included for trends and projections analysis. A detailed description of the survey year, sample size, and sample characteristics is presented in the supplementary (Table S1). The DHS generally applies a uniform procedure by using a multistage sampling technique to conduct the survey. The DHS survey methodology and questionnaire were reviewed and approved by the ICF Institutional Review Board. Upon taking informed consent, the DHS collected data from respondents, and we are using these publicly available anonymous data.
Indicators, definitions, and measurement approaches
We considered the global cut-off to classify Body Mass Index (BMI), calculated as dividing the weight in kilogram by square of height in meter, to define underweight (BMI < 18.5 kg/m2) and overweight (BMI ≥ 25.0 kg/m2) of women [29]. Women who were pregnant or lactating during the data collection were excluded from the analyses. According to the World Health Organization (WHO), <10% prevalence of underweight nationally refers to the warning sign of a country that requires monitoring while 10–19% underweight prevalence refers the medium prevalence, but ≥20% is considered as high or very high prevalence of underweight that further refers to a serious or critical situation of the country for public health significance [29]. However, the prevalence of underweight >20% and a variety of overweight prevalence (>20% or >30% or >40%) were used in defining the DBM among women at population level [24]. We used >20% cut-off of the concurrent presence of both underweight and overweight at the same time among women in the population level to assess the DBM.
For this study, we categorized education as below secondary (no education and primary) and secondary+ (secondary or higher) education and age as 15–19 years (adolescents) and 20–49 years (adults). Also, we used place of residence (as rural and urban) and wealth quintiles (as poorest (1st quintile), poorer, middle, richer, and richest (5th quintile)) that the DHS provided with the survey data.
Statistical analyses
We estimated the weighted prevalence of underweight and overweight as proportions from the original survey data. We calculated these prevalences across subgroups in terms of women’s residence, education, age, and wealth quintiles that the DHS constructed based on household assets by applying principal component analysis [30]. Notably, we restricted our analysis at the country level but not at the regional level for two reasons. First, there were very few countries in some regions with heterogeneity between survey years, and second, we were interested in assessing progress across individual countries so that country-level programs and policies can be implemented.
To examine trends, a Bayesian linear regression model that used the Markov Chain Monte Carlo algorithm of multiple imputations for missing data was applied to estimate both underweight and overweight and its trend from 1990 and 2030 (appendix). We reported credible intervals (CrI) along with these estimates. Aligning with the SDG-2 of eradicating malnutrition [21], we calculated the probability of reducing malnutrition at ≤0.5% by 2030 to understand which country and population within the country are on track to achieve the target.
We used Stata (version 15.1) and R (version 3.5) statistical software to analyze the data.
Results
Sample characteristics
Our study included 2,337,855 women 15–49 years of age. According to the latest survey, the mean age of women was lowest in Comoros (mean ± standard deviation: 27.7 ± 9.4) and highest in Jordan (36.1 ± 8.2), and mean BMI was lowest in Madagascar (20.3 ± 3.0) and highest in Egypt (30.3 ± 5.5). The majority of the study women were from rural areas, had below secondary education, and roughly one-fifth belonged to households with the lowest wealth quintile (Table S1). All the fitted models for projection analysis achieved convergence. The potential scale reduction factor values are summarized in the supplementary (Table S2 for underweight and Table S3 for overweight).
Trends and projections in malnutrition of women
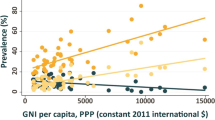
Among 55 countries during 1990–2018, the prevalence of underweight women declined in 35 countries (Fig. 1A) while 50 countries experienced an upward trend in the prevalence of overweight (Fig. 1B). The countries with the greatest reduction in the prevalence of underweight were Egypt (−11.4%), Turkey (−10.7%), and Pakistan (−6.9%), and with the highest increase of overweight was noted in Nepal (12.4%) followed by Bangladesh (12.0%) and Timor-Leste (7.0%) (Fig. 2). However, the prevalence of underweight in women increased in 20 countries, with the highest increase in Morocco (5.5%) followed by Maldives (2.7%) and Peru (2.7%). On the other hand, overweight is decreasing in Sierra Leone (−6.5%), Kazakhstan (−4.3%), Burundi (−1.0%), Senegal (−0.5%), and the Republic of the Congo (−0.1%) (Fig. 2). Nevertheless, if the current trends continue, it is projected that in 2030, the prevalence of underweight in women is expected to be ≥10% in 24 countries, with the highest burden estimated for Madagascar (36.8%, 95% CrI: 6.2–77.8%), Senegal (32.2%, 13.6–57.7%), Burundi (29.2%, 4.6–76.8%), and Morocco (29.0%, 3.8–75.9%). Whereas, it is projected that by 2030, >20% of women will be overweight in 52 of 55 countries. Projection analysis also showed that eight countries will be in critical situations (underweight in women ≥10%) in 2030 (Fig. S1). For overweight, Egypt will have the highest prevalence of overweight (94.7%, 88.4–98.2%) in 2030, while Sierra Leone (6.6%, 0.1–45.3%) will have the lowest (Fig. S1). The probability of eradicating underweight (≤0.5%) in women was 100% for Egypt and 55% for Nicaragua. All other countries have nearly a 0% chance to attain this target. The predictive probability of eradicating overweight (≤0.5%) in women is highest for Kazakhstan (23.0%). However, the probability of attaining this target is close to 0% for all other LMICs (data not shown).
Trends and projections of malnutrition in women across subpopulations
The trends in the prevalence of underweight and overweight in women varied across sociodemographic subpopulations. The prevalence of underweight in women decreased in 35 countries among the poorest (Fig. 3A), with the largest decrease observed in Tajikistan (−7.1%). Intriguingly, 20 countries saw an increasing rate of underweight, with Burkina Faso topping the list (3.3%). The number of countries which saw an increase or decrease in underweight were similar among women in the richest quintile (Table S4). Egypt had the largest decrease (−25.9%), and Morocco had the highest increase (9.4%) in underweight in the richest women. Based on these trends, Senegal (52.3%, 4.5–95.2%) is expected to have the highest prevalence of underweight among the poorest women, and Morocco (49.0%, 9.5–88.6%) among the richest women in 2030. Only two countries, Egypt (96%) and Kazakhstan (65%), have >50% probability of meeting the target of eradicating underweight among the poorest women, and only one country, Egypt, has a 100% probability of eradicating underweight among the richest women (Table S4). The trends in the prevalence of underweight in women also varied when women were stratified by their place of residence (Fig. S2 and Table S5), education (Fig. S3 and Table S6), and age (Fig. S4 and Table S7).
The trends in the prevalence of overweight also varied across sociodemographic subpopulations (Fig. 3B and Fig. S5–Fig. S7). Across subpopulations, the increase of overweight in women was highest in Bangladesh among the poorest (14.7%), rural (13.4%), below secondary educated (14.2%), and adult (11.6%) women; in Nepal among richest (8.6%), urban (10.5%) and secondary+ educated women (9.2%), and in Pakistan among adolescents (20.1%). In 2030, Egypt is projected to have the highest prevalence of overweight among poorest (94.9%, 86.4–98.6%), richest (92.7%, 80.0–98.4%), rural (95.0%, 89.5–98.0%), urban (95.0%, 88.6–98.2%), below secondary educated (95.7%, 90.4–98.5%), secondary+ educated (91.1%, 81.5–96.6%), and adult (95.1%, 89.3–98.4%) women (Table S8–Table S11).
Projected gaps in malnutrition of women across subpopulations
The projections also indicate that while underweight in women decreases in most countries, some countries will have large gaps in the prevalence of underweight in women across wealth, residence, education, and age. In 2030, the gaps in the prevalence of underweight between the poorest and the richest will be most prominent in Burkina Faso (Q1: 47.0% vs Q5: 6.0%) and least noticeable in Lesotho (Q1: 7.8% vs Q5: 7.8%). Conversely, some countries, e.g., Kazakhstan, will have a higher prevalence of underweight women in the highest quintile of wealth than their counterparts in 2030 (Q1: 4.3% vs Q5: 44.0%) (Fig. 4A). The gaps in the prevalence of underweight are also projected to be visible across the place of residence, education, and age of women. The highest rural-urban gaps in underweight will be in Burkina Faso where underweight will be higher in rural than urban areas and in the Maldives where underweight will be greater in urban than rural areas (Fig. S8). Morocco will have greater underweight prevalence among women with secondary+ education (Fig. S9) and Armenia will have the highest underweight prevalence among the adolescents (Fig. S10).
Although the gaps in the prevalence of overweight are decreasing across the levels of sociodemographic factors in some countries, most of the LMICs are projected to witness further widening of the difference in overweight prevalence, specifically across the levels of wealth distribution. The projected gaps in the prevalence of overweight in women are starkly different than underweight. In 2030, the richest women will have a higher prevalence of overweight than the poorest, with the highest gaps projected for Nepal (Q5: 80.3%, Q1: 23.8%) and lowest for Cambodia (Q5: 37.6%, Q1: 35.8%) (Fig. 4B). Overweight will be widely prevalent among urban women than rural, with the highest gaps in Mozambique (Fig. S8), and among adult women than adolescents, with the highest gaps in Nepal (Fig. S9). On the other hand, women with below secondary education will suffer from overweight than women with secondary+ education, with the highest gaps in Turkey (Fig. S10).
The double burden of malnutrition in women
The DBM varied across LMICs during the latest DHS rounds between 1999 and 2018, with the prevalence of underweight ranged from 0.2% in Egypt in 2014 to 26.7% in Madagascar in 2009 and overweight ranged from 6.3% in Madagascar in 2009 to 84.6% in Egypt in 2014 (Table 1). The DBM further varied across subpopulations (Table S12–Table S15). The trend analysis revealed that while the prevalence of underweight in LMICs is declining, overweight is sharply increasing. In the earliest DHS rounds, the prevalence of overweight was greater than underweight in 37 of 55 countries. Overweight crossed over underweight in 47 countries during their latest DHS round. However, based on the projected estimates, 45 countries will suffer from a higher prevalence of overweight (>20%) in 2030. Also, two countries are currently facing the DBM but seven countries are likely to experience the DBM in 2030 (Table 1). Similar to underweight and overweight, the status of DBM also varied across subpopulations (see Table S12–Table S15 for more details).
Discussion
This comprehensive study to assess the projected burden of underweight and overweight in women in LMICs highlights a rapid increase in the prevalence of overweight in many countries. Our results project that by 2030, no LMICs will be able to eradicate malnutrition in women for any subgroup of people. It is projected that most of the LMICs will have prevalence gaps in women’s underweight and overweight across the spectrum of socioeconomic disadvantages. The analyses of trends and projections at sociodemographic levels can help policy makers better identify and locate the population groups at risk for better allocation of resources and services considering the vulnerability of the disadvantaged population.
Our findings on the increasing trends of overweight and declining of underweight are consistent with previous studies in LMICs [22, 31,32,33]. Trends on reducing underweight and increasing overweight among women correspond with the similar trends identified in a recent study [34]. Similar to the previously reported epidemiological studies [15, 32], we also found a rapid shift in both these conditions. However, we found noticeable variations in the changes of underweight and overweight across subpopulations, with a sharp increase of overweight among the disadvantaged populations that may be attributed to growing urbanization and industrialization rates.
The data-driven analysis depicts that overweight among Egyptian women is sharply increasing nationally and in all subgroups studied, and projected nearly all women to be overweight at 2030. The ever-increasing prevalence of overweight among these women is likely due to their common practice of consuming fast-fried foods, sugary beverages, low intake of fruits and vegetables, unemployment, lack of physical activity, and sedentary behaviour [35, 36]. On the other hand, Sierra Leone is projected to control malnutrition among women in 2030. This might be driven by the dietary pattern of adults of Sierra Leone. The Global Nutrition Report 2018 showed that the consumption of food groups by Sierra Leonean adults is below the minimum theoretical risk of calcium, fruits, milk, nuts and seeds, omega 3, meat, trans fat, vegetables, and whole grain [37].
We found wealth, residence, education and age are strong determinants for both underweight and overweight, which are already well-known with findings from studies in both LMICs [22] and high-income countries [38]. Our analysis indicates important wealth-related gaps in both the prevalence of underweight and overweight in women. Similar to our study, a recent study also highlighted the increasing gaps in underweight and overweight across wealth and projected the highest underweight among poorest and overweight among richest in South and Southeast Asian countries [22]. It is anticipated that while no subgroup of women is likely to eradicate malnutrition in 2030, many countries are likely to have even wider gaps than that they are currently facing in the prevalence of underweight and overweight across sociodemographic equity dimensions.
Combating malnutrition is not a one-way task to apply. A multidisciplinary approach, including changing dietary patterns and lifestyle behaviours, is essential to strengthening national policies. In many high-income countries, the general features of overweight and obesity policies targeting children and adolescents are a reluctance to use taxes and industry regulations to change eating and drinking behaviours [39, 40]. To combat overweight/obesity, many middle-income countries are currently adopting policies to impose taxes on high energy-dense foods and strengthening industry regulations to reduce consumption of such foods and drinks [41]. Also, attempts must be made to make healthy foods such as grains, fruits, and vegetables available and affordable for many people by fixing prices, providing subsidies, cash transfers to vulnerable populations (conditionally on a need basis), and allocating food vouchers for the marginalized populations. The affordability of healthy foods may work in two ways. First, it may allow economically underserved groups to increase the consumption of healthy foods that reduce underweight. Second, it will reduce overweight among the richest if consumed by. Failure to provide affordable healthy foods may create wider inequality in malnutrition [42, 43] and might limit unhealthy food consumption policies. Introducing or scaling-up of maternal nutrition education can reduce malnutrition in women by improving their engagement in physical activity, eating fruits and vegetables [44].
The unique survey methodology and measurement allow this study for cross-country comparison of estimates. However, fewer data points with heterogeneity in survey years create wider CrI for the projected estimates for some countries (e.g., Kazakhstan). However, wider CrI can be narrowed down for countries (e.g., Bangladesh) having data from multiple time points. Also, realistic probability estimates are possible to calculate with wider CrI. Another limitation of this study is the use of BMI measurement to assess the nutritional status of reproductive women irrespective of adolescents 15–19 years of age. Also given the different population in diverse settings has different body compositions, the traditional BMI and its cut-off may not represent undernutrition and overnutrition [45]. Finally, the projected estimates may suffer from the lower provision and utilization of health services due to the current COVID-19 pandemic [46].
Overall, underweight is declining but the dramatic increase of overweight will supersede this decline. None of the 55 LMICs is likely to eradicate malnutrition in women by 2030. Effective strategies and nutrition interventions need to be instituted to minimize the nutritional disparities across subpopulations. The global goal of eradicating all forms of malnutrition should be grounded in a close collaborative approach through integrating policies and agencies to offer context and population-specific interventions. Without these, the paradox of DBM will continue in LMICs.
References
World Health Organization (WHO). The double burden of malnutrition- Policy brief. 2016. https://apps.who.int/iris/handle/10665/255413.
Han Z, Mulla S, Beyene J, Liao G, McDonald SD. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. 2011;40:65–101.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
Modjadji P, Madiba S. Childhood undernutrition and its predictors in a rural health and demographic surveillance system site in South Africa. Int J Environ Res Public Health. 2019;16. https://doi.org/10.3390/ijerph16173021.
Park D, Lee JH, Han S. Underweight: another risk factor for cardiovascular disease? Med (United States). 2017; 96. https://doi.org/10.1097/MD.0000000000008769.
Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE. 2013;8. https://doi.org/10.1371/journal.pone.0065174.
Ni Mhurchu C, Rodgers A, Pan WH, Gu DF, Woodward M, Parag V, et al. Body mass index and cardiovascular disease in the Asia-Pacific Region: an overview of 33 cohorts involving 310 000 participants. Int J Epidemiol. 2004;33:751–8.
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-Mass Index and Mortality among 1.46 Million White Adults. N Engl J Med. 2010;363:2211–9.
Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between Body-Mass Index and Risk of Death in More Than 1 Million Asians. N Engl J Med. 2011;364:719–29.
Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–95.
MacMahon S, Baigent C, Duffy S, Rodgers A, Tominaga S, Chambless L, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383:970–83.
Ezzati M, Lopez AD, Rodgers A. Hoorn S Vander, Murray CJL, Group CRAC. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60.
WHO. Global Health Risks: mortality and burden of disease attributable to selected major risks. 2009. http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf.
Mamun AA, Finlay JE. Shifting of undernutrition to overnutrition and its determinants among women of reproductive ages in the 36 low to medium income countries. Obes Res Clin Pr. 2015;9:75–86.
Popkin BM. The nutrition transition in the developing world. Dev Policy Rev. 2003;21:581–97.
Popkin BM. The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1:5–21.
Popkin BM. Nutrition Transition and the Global Diabetes Epidemic. Curr Diab Rep. 2015;15. https://doi.org/10.1007/s11892-015-0631-4.
World Health Organization. Global action plan for the prevention and control of non communicable diseases 2013–20. World Health Organization: 2013. https://apps.who.int/iris/handle/10665/94384.
Kontis V, Mathers CD, Rehm J, Stevens GA, Shield KD, Bonita R, et al. Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modelling study. Lancet. 2014;384:427–37.
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. 2015. https://sdgs.un.org/2030agenda.
Biswas T, Townsend N, Magalhaes RJS, Islam MS, Hasan MM, Mamun AA. Current progress and future directions in the double burden of malnutrition among women in South and Southeast Asian countries. Curr Dev Nutr. 2019;3:1–8.
Varghese JS, Stein AD. Malnutrition among women and children in India: limited evidence of clustering of underweight, anemia, overweight, and stunting within individuals and households at both state and district levels. Am J Clin Nutr. 2019;109:1207–15.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395:65–74.
Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395:75–88.
Nugent R, Levin C, Hale J, Hutchinson B. Economic effects of the double burden of malnutrition. Lancet. 2020;395:156–64.
Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395:142–55.
Rutstein SO, Rojas G. Guide to DHS Statistics. Demographic and Health Surveys, ORC Macro. Calverton, Maryland: 2006. https://dhsprogram.com/pubs/pdf/DHSG1/Guide_to_DHS_Statistics_29Oct2012_DHSG1.pdf.
World Health Organization. Nutrition landacape information system: country profile indicators: 2010 https://doi.org/10.1159/000362780.Interpretation.
Rutstein SO, Johnson K. DHS Comparative Reports No. 6 The DHS Wealth Index. Calverton, Maryland, USA: ORC Macro: 2004. https://dhsprogram.com/pubs/pdf/CR6/CR6.pdf
Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:1–16.
Mendez MA, Monteiro CA, Popkin BM. Overweight exceedes underweight among women in most developing countries. Am Soc Clin Nutr. 2009;2005:714–21.
Subramanian S, Smith GD. Patterns, distribution, and determinants of under- and overnutrition: a population-based study of women in India. Am J Clin Nutr. 2006;84:633–40.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Hassan NE, Wahba S, El-Alameey IR, El-Masry SA, Abushady MM, Abdel Hameed ER, et al. Dietary behaviour pattern and physical activity in overweight and obese Egyptian mothers: relationships with their children’s body mass index. Maced J Med Sci. 2016;4:353–8.
Hassan NE, El-Masry SA, Elshebini SM, Al-Tohamy M, Ahmed NH, Rasheed EA, et al. Comparison of three protocols: dietary therapy and physical activity, acupuncture, or laser acupuncture in management of obese females. Open Access Maced J Med Sci. 2014;2:191–7.
Report GN Global Nutrition Report: Sierra Leone Nutrition Profile. https://globalnutritionreport.org/resources/nutrition-profiles/africa/western-africa/sierra-leone/.
Sidik S, Rampal L. The prevalence and factors associated with obesity among adult women in Selangor, Malaysia. Asia Pac Fam Med. 2009;8:2.
Kraak VI, Vandevijvere S, Sacks G, Brinsden H, Hawkes C, Barquera S, et al. Progress achieved in restricting the marketing of high-fat, sugary and salty food and beverage products to children. Bull World Health Organ. 2016;94:540–8.
Hawkes C, Harris JL. An analysis of the content of food industry pledges on marketing to children. Public Health Nutr. 2011;14:1403–14.
Popkin BM. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr Rev. 2017;75:73–82.
Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73:643–60.
Powell LM, Chriqui JF, Khan T, Wada R, Chaloupka FJ. Assessing the potential effectiveness of food and beverage taxes and subsidies for improving public health: a systematic review of prices, demand and body weight outcomes. Obes Rev. 2013;14:110–28.
Mahmudiono T, Al Mamun A, Nindya TS, Andrias DR, Megatsari H, Rosenkranz RR. The effectiveness of nutrition education for overweight/obese mother with stunted children (NEO-MOM) in reducing the double burden of malnutrition. Nutrients. 2018;10:1–16.
Jayawardena R, Hills AP. Body composition derived Body Mass Index and Waist Circumference cut-offs for Sri Lankan adults. Obes Med. 2020; vol 18, Article ID 100214.
Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Heal. 2020;8:e901–e908.
Acknowledgements
This research is supported partially by the Australian Government through the Australian Research Council’s Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025). We thank the Demographic and Health Survey program for providing access to the data sets. We gratefully acknowledge the commitment of the Australian Government and the University of Queensland, Brisbane, QLD, Australia, to their research efforts. To undertake the PhD degree, MMH is supported by the “Research Training Program” scholarship jointly funded by the Commonwealth Government of Australia and the University of Queensland, Brisbane, QLD, Australia.
Author information
Authors and Affiliations
Contributions
MMH conceptualized the study and performed data acquisition, data analysis, interpretation of the findings, and drafting the paper. SA, RJSM, and AAM helped in conceptualizing the study and provided guidance. YF and TB helped to interpret the results and contributed to drafting the paper. SA, RJSM, and AAM critically reviewed the analysis and final version of the paper. All authors made a thorough review of the final draft and approved it for submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hasan, M.M., Ahmed, S., Soares Magalhaes, R.J. et al. Double burden of malnutrition among women of reproductive age in 55 low- and middle-income countries: progress achieved and opportunities for meeting the global target. Eur J Clin Nutr 76, 277–287 (2022). https://doi.org/10.1038/s41430-021-00945-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00945-y
This article is cited by
-
Double burden of malnutrition and its associated factors among women in low and middle income countries: findings from 52 nationally representative data
BMC Public Health (2023)
-
Wealth related inequality in women and children malnutrition in the state of Chhattisgarh and Tamil Nadu
BMC Nutrition (2022)
-
Development and Validation of a Questionnaire to Assess the Risk Factors, Facilitators, and Barriers to Postpartum Weight Management
The Journal of Obstetrics and Gynecology of India (2022)