Abstract
Background/objectives
Sarcopenia is an age-related muscle disease associated with higher mortality, morbidity risk and health costs. An easy and convenient sarcopenia screening test would be hugely valuable for clinical critical care. The study aimed to assess handgrip strength (HGS) as a screening tool for sarcopenia in acute care-unit inpatients, using the EWGSOP 1 reference-standard definition.
Subjects/methods
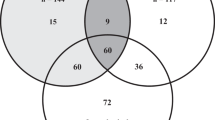
Inpatients, aged 75 years old or above, of two acute care wards—a multidisciplinary care unit (MCU) and a geriatric care unit (GCU), were included between September 2017 and June 2018 in a cross-sectional study. HGS, sarcopenia, nutritional status, functional status, number of medications and sociodemographic data were collected. The accuracy of HGS as a screening test for sarcopenia was assessed by gender using receiver operating characteristic (ROC) curves and area under the curve (AUC) in a population of older patients (n = 223; age: 85.8 yrs; BMI: 26.7 kg/m²).
Results
Screening was positive (patients confirmed with sarcopenia by the HGS test) with cut-off values of 18 kg for women and 25.5 kg for men, with ROC analysis giving a sensitivity of 92.9% in women and 78.6% in men. ROC curve analysis found also that HGS should be strictly higher than 15 kg in women and 18 kg in men to maximise AUC. Prevalence of sarcopenia according to the EWGSOP1 definition was 31.8% (95% CI: 22.1–41.6%) in the MCU and 27.8% (95% CI: 19.6–36.0%) in the GCU.
Conclusions
Acute care wards can use HGS as a valid, easy tool for early screening of sarcopenia.
Highlights
-
Handgrip strength is a valid and clinically practicable test, for screening early-onset sarcopenia during hospitalisation.
-
Handgrip strength cut-off values of 18 kg in women and 25.5 kg in men gave 92.9% and 78.6% sensitivity, respectively.
-
One-third of patients admitted to acute care wards have sarcopenia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Visser M, Schaap LA. Consequences of sarcopenia. Clin Geriatr Med. 2011;27:387–99. août
Leeper C, Lin E, Hoffman M, Fombona A, Zhou T, Kutcher M, et al. CT abbreviated assessment of sarcopenia following trauma: the CAAST measurement predicts 6-month mortality in older adult trauma patients. J Trauma Acute Care Surg. 2016;80:805–11.
Janssen I. Influence of sarcopenia on the development of physical disability: the cardiovascular health study. J Am Geriatr Soc. 2006;54:56–62.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer. 2016;57:58–67.
Nishigori T, Okabe H, Tanaka E, Tsunoda S, Hisamori S, Sakai Y. Sarcopenia as a predictor of pulmonary complications after esophagectomy for thoracic esophageal cancer. J Surg Oncol. 2016;113:678–84.
Chang S-F, Lin P-L. Systematic literature review and meta-analysis of the association of sarcopenia with mortality. Worldviews Evid-Based Nurs. 2016;13:153–62.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia and length of hospital stay. Eur J Clin Nutr. 2015;34:881–8.
Nishiguchi S, Yamada M, Shirooka H, Nozaki Y, Fukutani N, Tashiro Y, et al. Sarcopenia as a risk factor for cognitive deterioration in community-dwelling older adults: a 1-year prospective study. J Am Med Dir Assoc. 2016;17:372.e5–8.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–8.
Clynes MA, Edwards MH, Buehring B, Dennison EM, Binkley N, Cooper C. Definitions of sarcopenia: associations with previous falls and fracture in a population sample. Calcif Tissue Int. 2015;97:445–52.
Hirani V, Blyth F, Naganathan V, Le Couteur DG, Seibel MJ, Waite LM, et al. Sarcopenia is associated with incident disability, institutionalization, and mortality in community-dwelling older men: the concord health and ageing in men project. J Am Med Dir Assoc. 2015;16:607–13.
Cerri AP, Bellelli G, Mazzone A, Pittella F, Landi F, Zambon A, et al. Sarcopenia and malnutrition in acutely ill hospitalized elderly: prevalence and outcomes. Clin Nutr. 2015;34:745–51.
Vetrano DL, Landi F, Volpato S, Corsonello A, Meloni E, Bernabei R, et al. Association of sarcopenia with short- and long-term mortality in older adults admitted to acute care wards: results from the CRIME study. J Gerontol A Biol Sci Med Sci. 2014;69:1154–61.
Beaudart C, Zaaria M, Pasleau F, Reginster J-Y, Bruyère O. Health outcomes of sarcopenia: a systematic review and meta-analysis. PloS One. 2017;12:e0169548.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Ferreira S, Amaral TF. Financial impact of sarcopenia on hospitalization costs. Eur J Clin Nutr. 2016;70:1046–51.
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52:80–5.
Beaudart C, Rizzoli R, Bruyère O, Reginster J-Y, Biver E. Sarcopenia: burden and challenges for public health. Arch Public Health. 2014;72:45.
Dhillon RJS, Hasni S. Pathogenesis and management of sarcopenia. Clin Geriatr Med. 2017;33:17–26.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39:412–23.
Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(nov):748–59.
Walrand S, Gryson C, Salles J, Giraudet C, Migné C, Bonhomme C, et al. Fast-digestive protein supplement for ten days overcomes muscle anabolic resistance in healthy elderly men. Clin Nutr. 2016;35:660–8.
Boirie Y, Guillet C. Fast digestive proteins and sarcopenia of aging. Curr Opin Clin Nutr Metab Care. 2018;21:37–41.
Chanet A, Verlaan S, Salles J, Giraudet C, Patrac V, Pidou V, et al. Supplementing breakfast with a vitamin D and leucine-enriched whey protein medical nutrition drink enhances postprandial muscle protein synthesis and muscle mass in healthy older men. J Nutr. 2017;147:2262–71.
Ibrahim K, Howson FFA, Culliford DJ, Sayer AA, Roberts HC. The feasibility of assessing frailty and sarcopenia in hospitalised older people: a comparison of commonly used tools. BMC Geriatr. 2019;19:42.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8.
Laplante J, Cole M, McCusker J, Singh S, Ouimet M-A. Confusion Assessment Method. Validation of a French-language version. Perspect Infirm Rev Ordre Infirm Infirm Qué. 2005;3:12–4.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ. 2003;326:41–4.
Tichet J, Vol S, Goxe D, Salle A, Berrut G, Ritz P. Prevalence of sarcopenia in the French senior population. J Nutr Health Aging. 2008;12:202–6.
Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40:423–9.
Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56:1926–31.
Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv Plan Adm Eval. 1976;6:493–508.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56:M366–372.
Haute Autorité de Santé S des recommandations professionnelles. Stratégie de prise en charge en cas de dénutrition protéino-énergétique chez la personne âgée. Haute Autorité de Santé; 2007 avr p. 25.
Comparing the accuracy of two diagnostic tests. In: Statistical methods in diagnostic medicine [Internet]. John Wiley & Sons, Ltd; 2011 [cité 19 janv 2020]. p. 165–92. Disponible sur: https://onlinelibrary.wiley.com/doi/abs/10.1002/9780470906514.ch5.
Comparing the accuracy of two diagnostic tests. In: Statistical methods in diagnostic medicine [Internet]. John Wiley & Sons, Ltd; 2008 [cité 19 févr 2020]. p. 165–94. Disponible sur: https://onlinelibrary.wiley.com/doi/abs/10.1002/9780470317082.ch5.
Takwoingi Y, Quinn TJ. Review of Diagnostic Test Accuracy (DTA) studies in older people. Age Ageing. 2018;47:349–55.
Smoliner C, Sieber CC, Wirth R. Prevalence of sarcopenia in geriatric hospitalized patients. J Am Med Dir Assoc. 2014;15:267–72.
Rossi AP, Fantin F, Micciolo R, Bertocchi M, Bertassello P, Zanandrea V, et al. Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc. 2014;15:303.e7–12.
Zengarini E, Giacconi R, Mancinelli L, Riccardi GR, Castellani D, Vetrano DL, et al. Prognosis and interplay of cognitive impairment and sarcopenia in older adults discharged from Acute Care Hospitals. J Clin Med. 2019;8:1693.
Bianchi L, Abete P, Bellelli G, Bo M, Cherubini A, Corica F, et al. Prevalence and clinical correlates of sarcopenia, identified according to the EWGSOP definition and diagnostic algorithm, in hospitalized older people: the GLISTEN study. J Gerontol A Biol Sci Med Sci. 2017;72:1575–81.
Sipers WMWH, Meijers JMM, van Dijk RB, Halfens RJG, Schols JMGA. Impact of different diagnostic criteria on the prevalence of sarcopenia in an acute care geriatric ward. J Frailty Aging. 2014;3:222–9.
Sousa AS, Guerra RS, Fonseca I, Pichel F, Amaral TF. Sarcopenia among hospitalized patients—a cross-sectional study. Clin Nutr. 2015;34:1239–44.
Gariballa S, Alessa A. Sarcopenia: prevalence and prognostic significance in hospitalized patients. Clin Nutr. 2013;32:772–6.
Jacobsen EL, Brovold T, Bergland A, Bye A. Prevalence of factors associated with malnutrition among acute geriatric patients in Norway: a cross-sectional study. BMJ Open. 2016;6:e011512.
Papadopoulou SK, Tsintavis P, Potsaki P, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. a systematic review and meta-analysis. J Nutr Health Aging. 2020;24:83–90.
Acknowledgements
The research team thanks paramedical and medical staff of the two acute care wards.
Funding
The study was funded by Clermont-Ferrand University Hospital and two local hospitals. The study was sponsored by Nutriset and Nutricia (support from a national congress research price). These financial supports played no role in the design, execution, analysis and interpretation of the data.
Author information
Authors and Affiliations
Contributions
MB was responsible for designing the protocol, writing the protocol, conducting the clinical research, interpreting results and writing the article. GD was responsible for designing the protocol, conducting the clinical research and reading the article. AS was responsible for reading the article. SD and NF were responsible for designing the protocol and writing the article. VG was responsible for conducting the clinical research and reading the article. CGA and PB were responsible for designing the protocol, writing the protocol, extracting and analysing data, interpreting results and writing the article. JB was responsible for designing the protocol and reading the article. YB and LG were responsible for designing the protocol, interpreting results and writing the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blanquet, M., Ducher, G., Sauvage, A. et al. Handgrip strength as a valid practical tool to screen early-onset sarcopenia in acute care wards: a first evaluation. Eur J Clin Nutr 76, 56–64 (2022). https://doi.org/10.1038/s41430-021-00906-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00906-5
This article is cited by
-
Association between reduced physical performance measures and short-term consequences after major emergency abdominal surgery: a prospective cohort study
European Journal of Trauma and Emergency Surgery (2024)
-
Sarcopenia: if it looks/walks like a duck, it must be a duck
European Journal of Clinical Nutrition (2022)