Abstract
Objective
Few studies have evaluated the total energy expenditure (TEE) of children with disabilities using the doubly labeled water (DLW) method; however, none have compared it by disability type. Furthermore, no large-scale studies have focused on the severity of motor disability (MD). We aimed to compare TEE in children with disabilities by disability type.
Methods
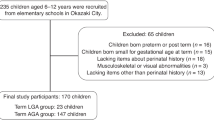
In a cross-sectional study design, TEE was measured using the DLW method, anthropometry, and weighted food records. The following comparisons were made: (1) TEEs among four disability types and (2) TEEs of three subgroups classified by MD based on the Gross Motor Function Classification System (GMFCS).
Results
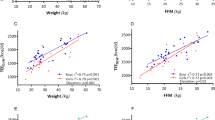
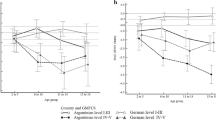
In total, 256 children (138 boys; ages 6–15 years) were studied. The comparison between the four disability types for boys in all age categories revealed that TEE (kJ/d) was lowest in MD, followed by intellectual disability (ID), visual disability, and hearing disability (HD), in that order. TEE/fat-free mass (FFM) (kJ/FFMkg/d) was also lowest in MD and highest in HD. TEE (kJ/d) and TEE/FFM (kJ/FFMkg/d) were also lowest in MD and highest in HD in girls. For both boys and girls, TEE (kJ/d) and TEE/FFM (kJ/FFMkg/d) were higher in the MD subtype GMFCS I–II than in GMFCS III–IV and GMFCS V.
Conclusions
TEE differed, depending on the disability type, and was the lowest in MD and highest in HD for both boys and girls. Analysis by GMFCS classification revealed that greater severity of motor dysfunction resulted in lower TEE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Schoeller DA. Energy expenditure from doubly labeled water: some fundamental considerations in humans. Am J Clin Nutr 1983;38:999–1005. https://doi.org/10.1093/ajcn/38.6.999
Schoeller DA, Ravussin E, Schutz Y, Acheson KJ, Baertschi P, Jequier E. Energy expenditure by doubly labeled water: validation in humans and proposed calculation. Am J Physiol 1986;250:R823–830. https://doi.org/10.1152/ajpregu.1986.250.5.R823
Speakman JR. The history and theory of the doubly labeled water technique. Am J Clin Nutr. 1998;68:932S–938S. https://doi.org/10.1093/ajcn/68.4.932S
Schoeller DA. Recent advances from application of doubly labeled water to measurement of human energy expenditure. J Nutr. 1999;129:1765–8. https://doi.org/10.1093/jn/129.10.1765
Tabata I, Ebine N, Kawashima Y, Ishikawa-Takata K, Tanaka S, Higuchi M, et al. Dietary reference intakes for Japanese 2010: energy. J Nutr Sci Vitaminol 2013;59:S26–S35. https://doi.org/10.3177/jnsv.59.S26
Brooks GA, Butte NF, Rand WM, Flatt JP, Caballero B. Chronicle of the Institute of Medicine physical activity recommendation: how a physical activity recommendation came to be among dietary recommendations. Am J Clin Nutr 2004;79:921S–30S. https://doi.org/10.1093/ajcn/79.5.921S
Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington DC: National Academies Press; 2005) p. 107–264
Kuperminc MN, Stevenson RD. Growth and nutrition disorders in children with cerebral palsy. Dev Disabil Res Rev. 2008;14:137–46.
Burrows T, Goldman S, Rollo M. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labelled water. Eur J Clin Nutr. 2019. https://doi.org/10.1016/j.jada.2010.07.008
Walker JL, Ardouin S, Burrows T. The validity of dietary assessment methods to accurately measure energy intake in children and adolescents who are overweight or obese: a systematic review. Eur J Clin Nutr. 2018;72:185–97. https://doi.org/10.1038/s41430-017-0029-2
Sardinha LB, Júdice PB. Usefulness of motion sensors to estimate energy expenditure in children and adults: a narrative review of studies using DLW. Eur J Clin Nutr 2017;71:331–9. https://doi.org/10.1038/ejcn.2017.2
Bandini LG, Schoeller DA, Fukagawa NK, Wykes LJ, Dietz WH. Body composition and energy expenditure in adolescents with cerebral palsy or myelodysplasia. Pediatr Res. 1991;29:70–77. https://doi.org/10.1203/00006450-199101000-00014
Polfuss M, Sawin KJ, Papanek PE, Bandini L. Total energy expenditure and body composition of children with developmental disabilities. Disabil Health J. 2018;11:442–6. https://doi.org/10.1016/j.dhjo.2017.12.009
Walker JL, Bell KL, Boyd RN, Davies PS. Validation of a modified three-day weighed food record for measuring energy intake in preschool-aged children with cerebral palsy. Clin Nutr. 2013;32:426–31. https://doi.org/10.1016/j.clnu.2012.09.005
Walker JL, Bell KL, Boyd RN, Davies PS. Energy requirements in preschool-age children with cerebral palsy. Am J Clin Nutr. 2012;96:1309–15. https://doi.org/10.3945/ajcn.112.043430
Rieken R, van Goudoever JB, Schierbeek H, Willemsen SP, Calis EA, Tibboel D, et al. Measuring body composition and energy expenditure in children with severe neurologic impairment and intellectual disability. Am J Clin Nutr 2011;94:759–66. https://doi.org/10.3945/ajcn.110.003798
Bell KL, Davies PS. Energy expenditure and physical activity of ambulatory children with cerebral palsy and of typically developing children. Am J Clin Nutr. 2010;92:313–9. https://doi.org/10.3945/ajcn.2010.29388
Stallings VA, Zemel BS, Davies JC, Cronk CE, Charney EB. Energy expenditure of children and adolescents with severe disabilities: a cerebral palsy model. Am J Clin Nutr 1996;64:627–34. https://doi.org/10.1093/ajcn/64.4.627
Sullivan PB, Alder N, Bachlet AM, Grant H. Gastrostomy feeding in cerebral palsy: too much of a good thing? Dev Med Child Neurol 2006;48:877–82. https://doi.org/10.1017/S0012162206001927
Luke A, Roizen NJ, Sutton M, Schoeller DA. Energy expenditure in children with Down syndrome: correcting metabolic rate for movement. J Pediatr 1994;125:829–38. https://doi.org/10.1016/S0022-3476(06)80193-9
International Atomic Energy Agency. Assessment of body composition and total energy expenditure in humans using stable isotope techniques. Vienna, Austria: International Atomic Energy Agency; 2009
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x
Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. 2008;50:744–50. https://doi.org/10.1111/j.1469-8749.2008.03089.x
Ministry of Education, Culture, Sports, Science and Technology. Annual Report of School Health Statistics Research. Tokyo, Japan: Ministry of Education, Culture, Sports, Science and Technology; 2010
Roberts SB, Dietz W, Sharp T, Dallal GE, Hill JO. Multiple laboratory comparison of the doubly labeled water technique. Obes Res. 1995;3:3–13. https://doi.org/10.1002/j.1550-8528.1995.tb00002.x
Speakman JR Assumptions in the single model of Lifson and co-workers. In: Doubly Labelled Water. Theory and Practice. London: Chapman & Hall; 1997. p.115–133
Lohman TG. Estimating body composition in children and the elderly. In: Advances in body composition assessment. Illinois: Human Kinetics Publishers; 1992. p. 65–77
Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. https://doi.org/10.1113/jphysiol.1949.sp004363
Black AE, Prentice AM, Coward WA. Use of food quotients to predict respiratory quotients for the doubly-labelled water method of measuring energy expenditure. Hum Nutr Clin Nutr. 1986;40:381–91
Calis EA, Veugelers R, Rieken R, Tibboel D, Evenhuis HM, Penning C. Energy intake does not correlate with nutritional state in children with severe generalized cerebral palsy and intellectual disability. Clin Nutr. 2010;29:617–21. https://doi.org/10.1016/j.clnu.2010.02.006
Wang J, Gao Y, Kwok HHM, Huang WYJ, Li S, Li L. Children with intellectual disability are vulnerable to overweight and obesity: a cross-sectional study among Chinese children. Child Obes. 2018;14:316–26. https://doi.org/10.1089/chi.2018.0015
Must A, Curtin C, Hubbard K, Sikich L, Bedford J, Bandini L. Obesity prevention for children with developmental disabilities. Curr Obes Rep. 2014;3:156–70. https://doi.org/10.1007/s13679-014-0098-7
Murray J, Ryan-Krause P. Obesity in children with Down syndrome: background and recommendations for management. Pediatr Nurs. 2010;36:314–9
Minister of Health, Labour and Welfare. Dietary reference intakes for Japanese (2015). II Energy and Nutrients. Table 4 The basal metabolism reference values for the reference bodyweight (BW). Tokyo, Japan 2015:45. https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000208955.pdf
Suzuki M, Saitoh S, Tasaki Y, Shimomura Y, Makishima R, Hosoya N. Nutritional status and daily physical activity of handicapped students in Tokyo metropolitan schools for deaf, blind, mentally retarded, and physically handicapped individuals. Am J Clin Nutr. 1991;54:1101–11. https://doi.org/10.1093/ajcn/54.6.1101
Ministry of Education, Culture, Sports, Science and Technology. School feeding standards for kindergarten and high schools of special support schools. 2009. Ministry of Education, Culture, Sports, Science and Technology Notification No. 63. https://www.mext.go.jp/content/1407743_003.pdf
Meyns P, Van Gestel L, Bar-On L, Goudriaan M, Wambacq H, Aertbelien E, et al. Children with spastic cerebral Palsy experience difficulties adjusting their gait pattern to weight added to the waist, while typically developing children do not. Front Hum Neurosci. 2016;10:657 https://doi.org/10.3389/fnhum.2016.00657
Xiao D, Qu Y, Huang L, Wang Y, Li X, Mu D Association between maternal overweight or obesity and cerebral palsy in children: A meta-analysis. PLoS ONE 2018; 13. https://doi.org/10.1371/journal.pone.0205733
Acknowledgements
We wish to thank the participating children, parents, principal, and staff members of each school who provided help in conducting this research.
Funding
This study was supported by a grant from the Ministry of Education, Culture, Sports, Science and Technology in Japan (to HO). The funders played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
HO designed and conducted the research, analyzed the data, and also wrote the paper. TN designed the research, analyzed the data, and wrote the paper. KIT designed the research, conducted research, and wrote the paper. NI analyzed the data. YK conducted the research. ST designed the research. All authors contributed to data interpretation and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ohwada, H., Nakayama, T., Ishikawa-Takata, K. et al. Total energy expenditure among children with motor, intellectual, visual, and hearing disabilities: a doubly labeled water method. Eur J Clin Nutr 75, 1607–1617 (2021). https://doi.org/10.1038/s41430-021-00885-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00885-7