Abstract
Background
Cesarean has been suggested to decrease neonatal iron stores at birth. However, few studies have differentiated the effect induced by cesarean operation from that related to medical indications.
Objectives
We aimed to estimate the association of cesarean delivery on maternal request (CDMR), a subtype of cesarean without any medical indications, with a spectrum of indicators reflecting iron stores at birth.
Methods
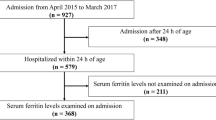
This prospective cohort study involved 288 term singleton neonates born to women without any complications by CDMR or spontaneous vaginal delivery (SVD). Measured hematological iron-related indicators in cord blood included serum ferritin (SF), hemoglobin (Hb), red blood cell (RBC), and hematocrit (Hct). Blood flow volume (BFV) of cord vein when clamping was measured to reflect placental transfusion status during birth. Quantile regression was used to assess the association between delivery mode and the iron store indicators.
Results
CDMR (n = 154) versus SVD group (n = 134) had lower conditional median cord blood SF (–34.80; 95% CI –64.70, –4.90 μg/L; P = 0.02), Hb (–10.67; 95% CI –18.87, –2.47 g/L; P = 0.01), RBC (–0.30; 95% CI –0.48, –0.12 ×1012/L; P = 0.002), and Hct (–3.06; 95% CI –6.08, –0.04 %; P = 0.047). The BFV was higher in CDMR than SVD group at the 25th centile (0.51; 95% CI 0.19, 0.82 ml/cm3; P = 0.002), median (0.49; 95% CI 0.04, 0.95 ml/cm3; P = 0.03) and the 75th centile (0.54; 95% CI 0.06, 1.03 ml/cm3; P = 0.03).
Conclusions
The cesarean operation per se likely hampered placental transfusion from mother to neonate and decreased iron stores at birth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Betran AP, Ye J, Moller AB, Zhang J, Gulmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS ONE. 2016;11:e0148343.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep. 2018;67:1–55.
Mylonas I, Friese K. Indications for and risks of elective cesarean section. Dtsch Arztebl Int. 2015;112:489–95.
Li HT, Luo S, Trasande L, Hellerstein S, Kang C, Li JX, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA. 2017;317:69–76.
Zhu YB, Li HT, Zhang YL, Li ZW, Zhang L, Liu JM. Secular trends of cesarean delivery and cesarean delivery on maternal request among primiparous women with singleton pregnancy in Southern and Northern China during 1993–2010. Zhonghua yi xue za zhi.2012;92:1734–7.
Zhou YB, Li HT, Zhu LP, Liu JM. Impact of cesarean section on placental transfusion and iron-related hematological indices in term neonates: a systematic review and meta-analysis. Placenta. 2014;35:1–8.
Kakkilaya V, Pramanik AK, Ibrahim H, Hussein S. Effect of placental transfusion on the blood volume and clinical outcome of infants born by cesarean section. Clin Perinatol. 2008;35:561–70. xi.
Shirvani F, Radfar M, Hashemieh M, Soltanzadeh MH, Khaledi H, Mogadam MA. Effect of timing of umbilical cord clamp on newborns’ iron status and its relation to delivery type. Arch Iran Med. 2010;13:420–5.
Yao AC, Hirvensalo M, Lind J. Placental transfusion-rate and uterine contraction. Lancet. 1968;1:380–3.
Yao AC, Lind J. Effect of gravity on placental transfusion. Lancet. 1969;2:505–8.
McCarthy EK, Kenny LC, Hourihane JOB, Irvine AD, Murray DM, Kiely ME. Impact of maternal, antenatal and birth-associated factors on iron stores at birth: data from a prospective maternal-infant birth cohort. Eur J Clin Nutr. 2017;71:782–7.
Hay G, Refsum H, Whitelaw A, Melbye EL, Haug E, Borch-Iohnsen B. Predictors of serum ferritin and serum soluble transferrin receptor in newborns and their associations with iron status during the first 2 y of life. Am J Clin Nutr. 2007;86:64–73.
Omori A, Manabe M, Kudo K, Tanaka K, Takahashi K, Kashiwakura I. Influence of obstetric factors on the yield of mononuclear cells, CD34+ cell count and volume of placental/umbilical cord blood. J Obstet Gynaecol Res. 2010;36:52–7.
Pafumi C, Farina M, Maggi I, Russo A, Pernicone G, Bandiera S, et al. Influence of the kind of delivery on umbilical cord blood collection. Haematologia. 2002;31:341–5.
Yamada T, Okamoto Y, Kasamatsu H, Horie Y, Yamashita N, Matsumoto K. Factors affecting the volume of umbilical cord blood collections. Acta Obstet Gynecol Scand. 2000;79:830–3.
Farrar D, Airey R, Law GR, Tuffnell D, Cattle B, Duley L. Measuring placental transfusion for term births: weighing babies with cord intact. BJOG. 2011;118:70–5.
Vain NE, Satragno DS, Gorenstein AN, Gordillo JE, Berazategui JP, Alda MG, et al. Effect of gravity on volume of placental transfusion: a multicentre, randomised, non-inferiority trial. Lancet. 2014;384:235–40.
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK. The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology. 2007;92:73–82.
Acharya G, Sitras V. Oxygen uptake of the human fetus at term. Acta Obstet Gynecol Scand. 2009;88:104–9.
Koenker R, Bassett Jr G. Robust test for heteroscedasticity based on regression quantiles. Econometrica. 1982;50:43–61.
Beyerlein A. Quantile regression-opportunities and challenges from a user’s perspective. Am J Epidemiol. 2014;180:330–1.
Institute of Medicine and National Research Council. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: The National Academies Press; 2009. http://iom.nationalacademies.org/en/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx.
Scholl TO. Iron status during pregnancy: setting the stage for mother and infant. Am J Clin Nutr. 2005;81:1218s–22s.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. http://www.who.int/vmnis/indicators/haemoglobin/en/.
Shao J, Lou J, Rao R, Georgieff MK, Kaciroti N, Felt BT, et al. Maternal serum ferritin concentration is positively associated with newborn iron stores in women with low ferritin status in late pregnancy. J Nutr. 2012;142:2004–9.
Chang YH, Yang SH, Wang TF, Lin TY, Yang KL, Chen SH. Complete blood count reference values of cord blood in Taiwan and the influence of gender and delivery route on them. Pediatr Neonatol. 2011;52:155–60.
Wu JH, Chou HC, Chen PC, Jeng SF, Chen CY, Tsao PN, et al. Impact of delivery mode and gestational age on haematological parameters in Taiwanese preterm infants. J Paediatr Child Health. 2009;45:332–6.
Roburn M. Relation of onset of respiration to placental transfusion. Lancet. 1965;1:651.
Lubetzky R, Ben-Shachar S, Mimouni FB, Dollberg S. Mode of delivery and neonatal hematocrit. Am J Perinatol. 2000;17:163–5.
Yektaei-Karin E, Moshfegh A, Lundahl J, Berggren V, Hansson LO, Marchini G. The stress of birth enhances in vitro spontaneous and IL-8-induced neutrophil chemotaxis in the human newborn. Pediatr Allergy Immunol. 2007;18:643–51.
Delaney KM, Guillet R, Fleming RE, Ru Y, Pressman EK, Vermeylen F, et al. Umbilical cord serum ferritin concentration is inversely associated with umbilical cord hemoglobin in neonates born to adolescents carrying singletons and women carrying multiples. J Nutr. 2019;149:406–15.
Lingman G, Marsal K. Fetal central blood circulation in the third trimester of normal pregnancy-a longitudinal study. I. Aortic and umbilical blood flow. Early Hum Dev. 1986;13:137–50.
Lees C, Albaiges G, Deane C, Parra M, Nicolaides KH. Assessment of umbilical arterial and venous flow using color Doppler. Ultrasound Obstet Gynecol. 1999;14:250–5.
Acknowledgements
We would like to give special thanks to all the staff and participants of the study.
Funding
This work is supported by National Key Research and Development Program of China [2016YFC1000401 and 2016YFC1000406-1], National Natural Science Foundation of China [81801542 and 81701538].
Author information
Authors and Affiliations
Contributions
JL conceived the study and supervised the study. YZ, HL and JL designed the study. YZ, HL, AL and JL conducted the study. ZL analyzed data. ZL and YZ wrote the manuscript. HL, AL, RLP and JL critically reviewed and revised the manuscript. JL had primary responsibility for final content. All the authors have reviewed and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics
The Institutional Review Board of Peking University approved this study. The written informed consent was obtained from all participant mothers.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41430_2021_874_MOESM3_ESM.docx
Table S2 Maternal and neonatal characteristics of participants with and without available data of cord blood Hb, RBC, and Hct.
41430_2021_874_MOESM4_ESM.docx
Table S3 Maternal and neonatal characteristics of participants without available data of cord blood Hb, RBC, and Hct according to delivery mode.
41430_2021_874_MOESM6_ESM.docx
Table S5 Adjusted quantile regression estimations (95% CI) of cord blood iron-related outcomes for CDMR compared with SVD, stratified by maternal SF.
Rights and permissions
About this article
Cite this article
Liao, Z., Zhou, Y., Liu, A. et al. Association of cesarean delivery on maternal request with neonatal iron stores at birth. Eur J Clin Nutr 75, 1637–1644 (2021). https://doi.org/10.1038/s41430-021-00874-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00874-w