Abstract
Background/objectives
The purpose of our study was to explore the relation of prenatal exposure to the Chinese famine and the risk of metabolic syndrome in adulthood in consecutive generations.
Subjects/methods
A total of 960 families, including 1920 parents (F1) who were born near the time of the Great Chinese famine and 1145 of their offspring (F2), were selected from the Suihua rural area. Parental participants were defined as nonexposed (born between 1 October 1956 and 30 September 1958 or between 1 October 1962 and 30 September 1964) and famine exposed (born between 1 October 1959 and 30 September 1961). In F2, participants were divided into having no parents exposed to famine, only a mother exposed to famine, only a father exposed to famine or both parents exposed to famine. Metabolic syndrome was defined by the International Diabetes Federation criteria.
Results
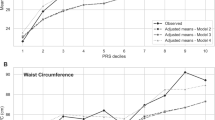
Exposure to famine during gestation was associated with an increased risk of metabolic syndrome (odds ratio: 2.79, 95% confidence interval: 2.16, 3.60) in F1 adults. However, similar association was not observed (maternal: odds ratio: 1.33, 95% confidence interval: 0.69, 2.52; paternal: odds ratio: 1.67, 95% confidence interval: 0.87, 3.21; parental: odds ratio: 1.25, 95% confidence interval: 0.68, 2.31) in F2 adults.
Conclusions
Exposure to the Chinese famine during foetal life was associated with an increased risk of metabolic syndrome in F1 participants. In F2 adults, there might be an important relationship between exposure to famine and the risk of metabolic syndrome with increasing age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Uauy R, Kain J, Corvalan C. How can the developmental origins of health and disease (DOHaD) hypothesis contribute to improving health in developing countries? Am J Clin Nutr. 2011;94:1759–64.
Gluckman PD, Hanson MA. The developmental origins of the metabolic syndrome. Trends Endocrinol Metab. 2004;15:183–7.
Wang Y, Wang X, Kong Y, Zhang JH, Zeng Q. The great Chinese famine leads to shorter and overweight females in Chongqing Chinese population after 50 years. Obesity (Silver Spring). 2010;18:588–92.
Ravelli AC, van Der Meulen JH, Osmond C, Barker DJ, Bleker OP. Obesity at the age of 50 y in men and women exposed to famine prenatally. Am J Clin Nutr. 1999;70:811–6.
Ravelli AC, van der Meulen JH, Michels RP, Osmond C, Barker DJ, Hales CN, et al. Glucose tolerance in adults after prenatal exposure to famine. Lancet. 1998;351:173–7.
de Rooij SR, Painter RC, Roseboom TJ, Phillips DI, Osmond C, Barker DJ, et al. Glucose tolerance at age 58 and the decline of glucose tolerance in comparison with age 50 in people prenatally exposed to the Dutch famine. Diabetologia. 2006;49:637–43.
Wang N, Cheng J, Han B, Li Q, Chen Y, Xia F, et al. Exposure to severe famine in the prenatal or postnatal period and the development of diabetes in adulthood: an observational study. Diabetologia. 2017;60:262–9.
Stein AD, Zybert PA, van der Pal-de Bruin K, Lumey LH. Exposure to famine during gestation, size at birth, and blood pressure at age 59 y: evidence from the Dutch Famine. Eur J Epidemiol. 2006;21:759–65.
Li Y, Jaddoe VW, Qi L, He Y, Lai J, Wang J, et al. Exposure to the Chinese famine in early life and the risk of hypertension in adulthood. J Hypertens. 2011;29:1085–92.
Lussana F, Painter RC, Ocke MC, Buller HR, Bossuyt PM, Roseboom TJ. Prenatal exposure to the Dutch famine is associated with a preference for fatty foods and a more atherogenic lipid profile. Am J Clin Nutr. 2008;88:1648–52.
Lumey LH, Stein AD, Susser E. Prenatal Famine and Adult Health. Annu Rev Public Health. 2011;32:237–62.
de Rooij SR, Painter RC, Holleman F, Bossuyt PM, Roseboom TJ. The metabolic syndrome in adults prenatally exposed to the Dutch famine. Am J Clin Nutr. 2007;86:1219–24.
Ng SF, Lin RC, Laybutt DR, Barres R, Owens JA, Morris MJ. Chronic high-fat diet in fathers programs beta-cell dysfunction in female rat offspring. Nature. 2010;467:963–6.
Carone BR, Fauquier L, Habib N, Shea JM, Hart CE, Li R, et al. Paternally induced transgenerational environmental reprogramming of metabolic gene expression in mammals. Cell. 2010;143:1084–96.
Benyshek DC, Johnston CS, Martin J. Glucose metabolism is altered in the adequately-nourished grand-offspring (F3 generation) of rats malnourished during gestation and perinatal life. Diabetologia. 2006;49:1117–9.
Mu R, Zhang X. Why does the great Chinese famine affect the male and female survivors differently? Mortality selection versus son preference. Econ Hum Biol. 2011;9:92–105.
Li Y, Jaddoe VW, Qi L, He Y, Wang D, Lai J, et al. Exposure to the Chinese famine in early life and the risk of metabolic syndrome in adulthood. Diabetes Care. 2011;34:1014–8.
Li J, Liu S, Li S, Feng R, Na L, Chu X, et al. Prenatal exposure to famine and the development of hyperglycemia and type 2 diabetes in adulthood across consecutive generations:a population-based cohort study of families in Suihua, China. Am J Clin Nutr. 2017;105:221–7.
Huang L, Xue J, He Y, Wang J, Sun C, Feng R, et al. Dietary calcium but not elemental calcium from supplements is associated with body composition and obesity in Chinese women. PLoS ONE. 2011;6:e27703.
Alberti KG, Zimmet P, Shaw J. The metabolic syndrome-a new worldwide definition. Lancet. 2005;366:1059–62.
Yu C, Wang J, Wang F, Han X, Hu H, Yuan J, et al. Victims of Chinese famine in early life have increased risk of metabolic syndrome in adulthood. Nutrition. 2018;53:20–5.
Zheng X, Wang Y, Ren W, Luo R, Zhang S, Zhang JH, et al. Risk of metabolic syndrome in adults exposed to the great Chinese famine during the fetal life and early childhood. Eur J Clin Nutr. 2012;66:231–6.
Yajnik C. Interactions of perturbations in intrauterine growth and growth during childhood on the risk of adult-onset disease. Proc Nutr Soc. 2000;59:257–65.
Hales CN, Barker DJ. The thrifty phenotype hypothesis. Br Med Bull. 2001;60:5–20.
Drake AJ, Liu L. Intergenerational transmission of programmed effects: public health consequences. Trends Endocrinol Metab. 2010;21:206–13.
Tam CH, Wang Y, Luan J, Lee HM, Luk AO, Tutino GE, et al. Maternal history of diabetes is associated with increased cardiometabolic risk in Chinese. Nutr Diabetes. 2014;4:e112.
Torrens C, Poston L, Hanson MA. Transmission of raised blood pressure and endothelial dysfunction to the F2 generation induced by maternal protein restriction in the F0, in the absence of dietary challenge in the F1 generation. Br J Nutr. 2008;100:760–6.
Pinheiro AR, Salvucci ID, Aguila MB, Mandarim-de-Lacerda CA. Protein restriction during gestation and/or lactation causes adverse transgenerational effects on biometry and glucose metabolism in F1 and F2 progenies of rats. Clin Sci (Lond). 2008;114:381–92.
Zambrano E, Martinez-Samayoa PM, Bautista CJ, Deas M, Guillen L, Rodriguez-Gonzalez GL, et al. Sex differences in transgenerational alterations of growth and metabolism in progeny (F2) of female offspring (F1) of rats fed a low protein diet during pregnancy and lactation. J Physiol. 2005;566:225–36.
Painter RC, Osmond C, Gluckman P, Hanson M, Phillips DI, Roseboom TJ. Transgenerational effects of prenatal exposure to the Dutch famine on neonatal adiposity and health in later life. BJOG. 2008;115:1243–9.
Evertts AG, Zee BM, Garcia BA. Modern approaches for investigating epigenetic signaling pathways. J Appl Physiol. 2010;109:927–33.
Tobi EW, Goeman JJ, Monajemi R, Gu H, Putter H, Zhang Y, et al. DNA methylation signatures link prenatal famine exposure to growth and metabolism. Nat Commun. 2014;5:5592.
Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw GJ, Susser ES, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci USA. 2008;105:17046–9.
Jaenisch R, Bird A. Epigenetic regulation of gene expression: how the genome integrates intrinsic and environmental signals. Nat Genet. 2003;33:245–54.
Simmons R. Epigenetics and maternal nutrition: nature v. nurture. Proc Nutr Soc. 2011;70:73–81.
Li C, Lumey LH. Exposure to the Chinese famine of 1959–61 in early life and long-term health conditions: a systematic review and meta-analysis. Int J Epidemiol. 2017;46:1157–70.
Pembrey ME, Bygren LO, Kaati G, Edvinsson S, Northstone K, Sjostrom M, et al. Sex-specific, male-line transgenerational responses in humans. Eur J Hum Genet. 2006;14:159–66.
Schulz LC. The Dutch hunger winter and the developmental origins of health and disease. PNAS. 2010;107:16757–8.
Acknowledgements
We appreciate that all staff from the Suihua Beilin CDC of Heilongjiang Province and nurses working in local hospitals positively participated in our study. Students from the Department of Nutrition and Food Hygiene supported this study by collecting and sorting data.
Funding
This research was funded and supported by the Department of Nutrition and Food Hygiene, School of Public Health, Harbin Medical University & the National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to this article. TSH conceived and designed the study. WBJ arranged a series of procedures to achieve population data. SWY analysed the data, interpreted the results and wrote and revised the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, S., Hou, W., Wu, H. et al. Prenatal exposure to the Chinese famine and the risk of metabolic syndrome in adulthood across consecutive generations. Eur J Clin Nutr 74, 1229–1236 (2020). https://doi.org/10.1038/s41430-020-0561-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0561-3
This article is cited by
-
Reply to ‘Chinese famine and metabolic syndrome: a longitudinal cohort study in Suihua China’
European Journal of Clinical Nutrition (2021)
-
Chinese famine and metabolic syndrome: a longitudinal cohort study in Suihua China
European Journal of Clinical Nutrition (2021)