Abstract
Background
Malnutrition is prevalent that can impair multiple clinical outcomes in oncology populations. This study aimed to develop and utilize a tool to optimize the early identification of malnutrition in patients with cancer.
Methods
We performed an observational cohort study including 3998 patients with cancer at two teaching hospitals in China. Hierarchical clustering was performed to classify the patients into well-nourished or malnourished clusters based on 17 features reflecting the phenotypic and etiologic dimensions of malnutrition. Associations between the identified clusters and patient characteristics were analyzed. A nomogram for predicting the malnutrition probability was constructed and independent validation was performed to explore its clinical significance.
Results
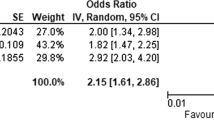
The cluster analysis identified a well-nourished cluster (n = 2736, 68.4%) and a malnourished cluster (n = 1262, 31.6%) in the study population, which showed significant agreement with the Patient-Generated Subjective Global Assessment and the Global Leadership Initiative on Malnutrition criteria (both P < 0.001). The malnourished cluster was negatively associated with the nutritional status, physical status, quality of life, short-term outcomes and was an independent risk factor for survival (HR = 1.38, 95%CI = 1.22–1.55, P < 0.001). Sex, gastrointestinal symptoms, weight loss percentages (within and beyond 6 months), calf circumference, and body mass index were incorporated to develop the nomogram, which showed high performance to predict malnutrition (AUC = 0.972, 95%CI = 0.960–0.983). The decision curve analysis and independent external validation further demonstrated the effectiveness and clinical usefulness of the tool.
Conclusions
Nutritional features-based clustering analysis is a feasible approach to define malnutrition. The derived nomogram shows effectiveness for the early identification of malnutrition in patients with cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available to protect patient confidentiality but are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32.
Canonici A, Browne AL, Ibrahim MFK, Fanning KP, Roche S, Conlon NT, et al. Combined targeting EGFR and SRC as a potential novel therapeutic approach for the treatment of triple negative breast cancer. Ther Adv Med Oncol. 2020;12:1758835919897546.
Yoshii Y, Tashima H, Iwao Y, Yoshida E, Wakizaka H, Akamatsu G, et al. Immuno-OpenPET: a novel approach for early diagnosis and image-guided surgery for small resectable pancreatic cancer. Sci Rep. 2020;10:4143.
Bagcchi S. Lung cancer survival only increases by a small amount despite recent treatment advances. Lancet Respir Med. 2017;5:169.
Almasaudi AS, McSorley ST, Dolan RD, Edwards CA, McMillan DC. The relation between Malnutrition Universal Screening Tool (MUST), computed tomography-derived body composition, systemic inflammation, and clinical outcomes in patients undergoing surgery for colorectal cancer. Am J Clin Nutr. 2019;110:1327–34.
Vangelov B, Venchiarutti RL, Smee RI. Critical Weight Loss in Patients With Oropharynx Cancer During Radiotherapy (+/- Chemotherapy). Nutr Cancer. 2017;69:1211–8.
Sanchez-Lara K, Ugalde-Morales E, Motola-Kuba D, Green D. Gastrointestinal symptoms and weight loss in cancer patients receiving chemotherapy. Br J Nutr. 2013;109:894–7.
Preiser JC, Schneider SM. ESPEN disease-specific guideline framework. Clin Nutr. 2011;30:549–52.
Morita Y, Sakaguchi T, Kitajima R, Furuhashi S, Kiuchi R, Takeda M, et al. Body weight loss after surgery affects the continuity of adjuvant chemotherapy for pancreatic cancer. BMC Cancer. 2019;19:416.
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A. Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections—results from a National Quality Registry. Clin Nutr. 2020;39:1593–99.
Gupta D, Lis CG, Granick J, Grutsch JF, Vashi PG, Lammersfeld CA. Malnutrition was associated with poor quality of life in colorectal cancer: a retrospective analysis. J Clin Epidemiol. 2006;59:704–9.
Pressoir M, Desne S, Berchery D, Rossignol G, Poiree B, Meslier M, et al. Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer. 2010;102:966–71.
Yin L, Lin X, Li N, Zhang M, He X, Liu J, et al. Evaluation of the global leadership initiative on malnutrition criteria using different muscle mass indices for diagnosing malnutrition and predicting survival in lung cancer patients. JPEN J Parenter Enteral Nutr. 2020; https://doi.org/10.1002/jpen.1873 (Online ahead of print).
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11–48.
Torricelli P, Antonelli F, Ferorelli P, Borromeo I, Shevchenko A, Lenzi S, et al. Oral nutritional supplement prevents weight loss and reduces side effects in patients in advanced lung cancer chemotherapy. Amino Acids. 2020;52:445–51.
Langius JA, Zandbergen MC, Eerenstein SE, van Tulder MW, Leemans CR, Kramer MH, et al. Effect of nutritional interventions on nutritional status, quality of life and mortality in patients with head and neck cancer receiving (chemo)radiotherapy: a systematic review. Clin Nutr. 2013;32:671–8.
de Pinho NB, Martucci RB, Rodrigues VD, D’Almeida CA, Thuler LCS, Saunders C, et al. High prevalence of malnutrition and nutrition impact symptoms in older patients with cancer: Results of a Brazilian multicenter study. Cancer. 2020;126:156–64.
Alvaro Sanz E, Garrido Siles M, Rey Fernandez L, Villatoro Roldan R, Rueda Dominguez A, Abiles J. Nutritional risk and malnutrition rates at diagnosis of cancer in patients treated in outpatient settings: early intervention protocol. Nutrition. 2019;57:148–53.
Li YF, Nie RC, Wu T, Li SM, Chen S, Wang W, et al. Prognostic value of the nutritional risk screening 2002 scale in metastatic gastric cancer: a large-scale cohort study. J Cancer. 2019;10:112–9.
Gioulbasanis I, Baracos VE, Giannousi Z, Xyrafas A, Martin L, Georgoulias V, et al. Baseline nutritional evaluation in metastatic lung cancer patients: Mini Nutritional Assessment versus weight loss history. Ann Oncol. 2011;22:835–41.
Hettiarachchi J, Madubhashini P, Miller M. Agreement between the malnutrition universal screening tool and the patient-generated subjective global assessment for cancer outpatients receiving chemotherapy: a cross-sectional study. Nutr Cancer. 2018;70:1275–82.
Martin L, Watanabe S, Fainsinger R, Lau F, Ghosh S, Quan H, et al. Prognostic factors in patients with advanced cancer: use of the patient-generated subjective global assessment in survival prediction. J Clin Oncol. 2010;28:4376–83.
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9.
Cederholm T, Jensen GL. To create a consensus on malnutrition diagnostic criteria: aA report from the Global Leadership Initiative on Malnutrition (GLIM) meeting at the ESPEN Congress 2016. Clin Nutr. 2017;36:7–10.
Loh KW, Vriens MR, Gerritsen A, Borel Rinkes IH, van Hillegersberg R, Schippers C, et al. Unintentional weight loss is the most important indicator of malnutrition among surgical cancer patients. Neth J Med. 2012;70:365–9.
Sanchez-Rodriguez D, Marco E, Ronquillo-Moreno N, Maciel-Bravo L, Gonzales-Carhuancho A, Duran X, et al. ASPEN-AND-ESPEN: A postacute-care comparison of the basic definition of malnutrition from the American Society of Parenteral and Enteral Nutrition and Academy of Nutrition and Dietetics with the European Society for Clinical Nutrition and Metabolism definition. Clin Nutr. 2019;38:297–302.
Baltazar GA, Pate AJ, Panigrahi B, LaBoy S, Prosniak R, Mody A, et al. Malnutrition as measured by albumin and prealbumin on admission is associated with poor outcomes after severe traumatic brain injury. Am Surg. 2015;81:E61–3.
Ryan AM, Power DG, Daly L, Cushen SJ, Ni Bhuachalla E, Prado CM. Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc. 2016;75:199–211.
Xu H, Song C, Wang C, Fu Z, Guo Z, Lin Y, et al. Investigation on nutrition status and clinical outcome of patients with common cancers in Chinese patients: a multicenter prospective study protocol. Int J Clin Trials. 2020;7:94–102.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational, et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Murri R, Scoppettuolo G, Damiano F, Ammassari A, Fantoni M, Antinori A. Karnofsky performance status and assessment of global health status. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13:294–5.
Wan C, Meng Q, Yang Z, Tu X, Feng C, Tang X, et al. Validation of the simplified Chinese version of EORTC QLQ-C30 from the measurements of five types of inpatients with cancer. Ann Oncol. 2008;19:2053–60.
Ottery FD. Rethinking nutritional support of the cancer patient: the new field of nutritional oncology. Semin Oncol. 1994;21:770–8.
Martin L, Gioulbasanis I, Senesse P, Baracos VE. Cancer-associated malnutrition and CT-defined sarcopenia and myosteatosis are endemic in overweight and obese patients. JPEN J Parenter Enter Nutr. 2020;44:227–38.
Kwon YJ, Kim HS, Jung DH, Kim JK. Cluster analysis of nutritional factors associated with low muscle mass index in middle-aged and older adults. Clin Nutr. 2020;39:3369–76.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36:49–64.
De Groot LM, Lee G, Ackerie A, van der Meij BS. Malnutrition screening and assessment in the cancer care ambulatory setting: mortality predictability and validity of the patient-generated subjective global assessment short form (PG-SGA SF) and the GLIM criteria.Nutrients. 2020;12:2287.
Kim S, Kim M, Lee Y, Kim B, Yoon TY, Won CW. Calf circumference as a simple screening marker for diagnosing sarcopenia in older Korean adults: the Korean frailty and aging cohort study (KFACS). J Korean Med Sci. 2018;33:e151.
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15:969–76.
Hisanaga T, Shinjo T, Imai K, Katayama K, Kaneishi K, Honma H, et al. Clinical guidelines for management of gastrointestinal symptoms in cancer patients: the Japanese society of palliative medicine recommendations. J Palliat Med. 2019;22:986–97.
Rangwala F, Zafar SY, Abernethy AP. Gastrointestinal symptoms in cancer patients with advanced disease: new methodologies, insights, and a proposed approach. Curr Opin Support Palliat Care. 2012;6:69–76.
Funding
This work was supported by the National Natural Science Foundation of China (81673167), the National Key Research and Development Program (2017YFC1309200), and the Chongqing Technology Innovation and Application Demonstration Project for Social Livelihood (cstc2018jscx-msybX0094).
Author information
Authors and Affiliations
Contributions
Conceptualization and study design: HXX, HPS, JWC, and LYY. investigation: LYY and HXX. Statistical analysis: LYY. Data interpretation: JL, XL, NL, JG, YF, LZ, MLS, HMZ, XC, CW, LD, WL, ZMF, CHS, and ZQG. Paper preparation: LYY. All authors have read and approved the final paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yin, L., Liu, J., Lin, X. et al. Nutritional features-based clustering analysis as a feasible approach for early identification of malnutrition in patients with cancer. Eur J Clin Nutr 75, 1291–1301 (2021). https://doi.org/10.1038/s41430-020-00844-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00844-8
This article is cited by
-
PWSC: a novel clustering method based on polynomial weight-adjusted sparse clustering for sparse biomedical data and its application in cancer subtyping
BMC Bioinformatics (2023)
-
Several anthropometric measurements and cancer mortality: predictor screening, threshold determination, and joint analysis in a multicenter cohort of 12138 adults
European Journal of Clinical Nutrition (2022)