Abstract
Background/objectives
Iodine is essential for foetal neurodevelopment and growth. Requirements increase in pregnancy to support increased thyroid hormone synthesis for maternal and foetal requirements, and for foetal transfer. Iodine deficiency in pregnancy is widely reported, and obesity has been associated with sub-optimal thyroid function. We evaluated iodine status and its relation with birthweight in a secondary analysis of pregnant women with obesity from multi-ethnic inner-city settings who participated in the UK Pregnancies Better Eating and Activity trial (UPBEAT).
Subjects/methods
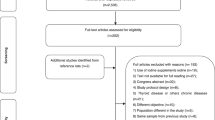
Iodine and creatinine concentrations were evaluated in spot urine samples in the second (15+0–18+6 weeks, n = 954) trimester of pregnancy. We assessed iodine status as urinary iodine concentration (UIC) and urinary iodine-to-creatinine ratio (UI/Cr) and applied WHO/UNICEF/IGN population threshold of median UIC > 150 µg/L for iodine sufficiency. Relationships between iodine status and birthweight were determined using linear and logistic regression with appropriate adjustment, including for maternal BMI and gestational age.
Results
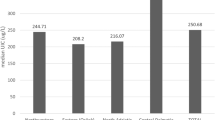
Median (IQR) UIC and UI/Cr in the second trimester of pregnancy were 147 µg/L (99–257) and 97 µg/g (59–165), respectively. An UI/Cr <150 μg/g was observed in 70% of women. Compared to women with UI/Cr >150 µg/g, there was a trend for women with UI/Cr <150 µg/g to deliver infants with a lower birthweight (β = −60.0 g; 95% CI −120.9 to −1.01, P = 0.05).
Conclusions
Iodine status of pregnant women with obesity from this cohort of UK women was suboptimal. Lower iodine status was associated with lower birthweight.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Glinoer D. The regulation of thyroid function during normal pregnancy: importance of the iodine nutrition status. Best Pr Res Clin Endocrinol Metab. 2004;18:133–52.
WHO. UNICEF & ICCIDD assessment of iodine deficiency disorders and monitoring their elimination. Geneva (Switzerland): WHO; 2007.
Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet (Lond, Engl). 2008;372:1251–62.
Hynes KL, Otahal P, Hay I, Burgess JR. Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J Clin Endocrinol Metab. 2013;98:1954–62.
Markhus MW, Dahl L, Moe V, Abel MH, Brantsæter AL, Øyen J, et al. Maternal iodine status is associated with offspring language skills in infancy and toddlerhood. Nutrients. 2018;10. https://doi.org/10.3390/nu10091270.
Robinson SM, Crozier SR, Miles EA, Gale CR, Calder PC, Cooper C, et al. Preconception maternal iodine status is positively associated with IQ but not with measures of executive function in childhood. J Nutr. 2018;148:959–66.
Bath SC, Steer CD, Golding J, Emmett P, Rayman MP. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet (Lond, Engl). 2013;382:331–7.
Robson H, Siebler T, Shalet SM, Williams GR. Interactions between GH, IGF-I, glucocorticoids, and thyroid hormones during skeletal growth. Pediatr Res. 2002;52:137–47.
Zimmermann MB. The role of iodine in human growth and development. Semin Cell Dev Biol. 2011;22:645–52.
Snart CJP, Keeble C, Taylor E, Cade JE, Stewart PM, Zimmermann M, et al. Maternal iodine status and associations with birth outcomes in three major cities in the United Kingdom. Nutrients. 2019;11:1–12.
Charoenratana C, Leelapat P, Traisrisilp K, Tongsong T. Maternal iodine insufficiency and adverse pregnancy outcomes. Matern Child Nutr. 2016;12:680–7.
Alvarez-Pedrerol M, Guxens M, Mendez M, Canet Y, Martorell R, Espada M, et al. Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. Eur J Endocrinol. 2009;160:423–9.
León G, Murcia M, Rebagliato M, Álvarez-Pedrerol M, Castilla AM, Basterrechea M, et al. Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente Cohort, Spain. Paediatr Perinat Epidemiol. 2015;29:113–22.
Torlinska B, Bath SC, Janjua A, Boelaert K, Chan S-Y. Iodine Status during Pregnancy in a Region of Mild-to-Moderate Iodine Deficiency is not Associated with Adverse Obstetric Outcomes; Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Nutrients. 2018;10:1–13.
Rydbeck F, Rahman A, Grandér M, Ekström E-C, Vahter M, Kippler M. Maternal Urinary Iodine Concentration up to 1.0 mg/L Is Positively Associated with Birth Weight, Length, and Head Circumference of Male Offspring. J Nutr. 2014;144:1438–44.
Farebrother J, Naude CE, Nicol L, Sang Z, Yang Z, Jooste PL, et al. Effects of iodized salt and iodine supplements on prenatal and postnatal growth: a systematic review. Adv Nutr. 2018;9. https://doi.org/10.1093/advances/nmy009.
Nazeri P, Shab-Bidar S, Pearce EN, Shariat M. Do maternal urinary iodine concentration or thyroid hormones within the normal range during pregnancy affect growth parameters at birth? A systematic review and meta-analysis. Nutr Rev. 2020;0:1–17.
Zimmermann MB. Methods to assess iron and iodine status. Br J Nutr. 2008;99(Suppl 3):S2–9.
Bath SC, Rayman MP. Iodine deficiency in the UK: An overlooked cause of impaired neurodevelopment? Proc Nutr Soc. 2013;72:226–35.
National Diet and Nutrition Survey. NDNS: Results from Years 7 and 8. Public Health England;2018.
Bath SC, Rayman MP. A review of the iodine status of UK pregnant women and its implications for the offspring. Environ Geochem Health. 2015;37:619–29.
Knight BA, Shields BM, He X, Pearce EN, Braverman LE, Sturley R, et al. Iodine deficiency amongst pregnant women in South-West England. Clin Endocrinol (Oxf). 2017;86:451–5.
McMullan P, Hamill L, Doolan K, Hunter A, McCance D, Patterson C, et al. Iodine deficiency among pregnant women living in Northern Ireland. Clin Endocrinol (Oxf). 2019;91:639–45.
Dahl L, Wik Markhus M, Sanchez PVR, Moe V, Smith L, Meltzer HM, et al. Iodine deficiency in a study population of norwegian pregnant women-results from the little in Norway Study (LiN). Nutrients. 2018;10:1–14.
Henjum S, Aakre I, Lilleengen AM, Garnweidner-Holme L, Borthne S, Pajalic Z, et al. Suboptimal iodine status among pregnant women in the Oslo Area, Norway. Nutrients. 2018;10:1–14.
Granfors M, Andersson M, Stinca S, Åkerud H, Skalkidou A, Poromaa IS, et al. Iodine deficiency in a study population of pregnant women in Sweden. Acta Obstet Gynecol Scand. 2015;94:1168–74.
Aguayo A, Grau G, Vela A, Aniel-Quiroga A, Espada M, Martul P, et al. Urinary iodine and thyroid function in a population of healthy pregnant women in the North of Spain. J Trace Elem Med Biol. 2013;27:302–6.
Limbert E, Prazeres S, São Pedro M, Madureira D, Miranda A, Ribeiro M, et al. Iodine intake in Portuguese pregnant women: results of a countrywide study. Eur J Endocrinol. 2010;163:631–5.
Dineva M, Rayman MP, Levie D, Guxens M, Peeters RP, Vioque J, et al. Similarities and differences of dietary and other determinants of iodine status in pregnant women from three European birth cohorts. Eur J Nutr. 2019. https://doi.org/10.1007/s00394-019-01913-w.
Devlieger R, Benhalima K, Damm P, Van Assche A, Mathieu C, Mahmood T, et al. Maternal obesity in Europe: where do we stand and how to move forward?: A scientific paper commissioned by the European Board and College of Obstetrics and Gynaecology (EBCOG). Eur J Obstet Gynecol Reprod Biol. 2016;201:203–8.
Song R, Wang B, Yao Q, Li Q, Jia X, Zhang J. The impact of obesity on thyroid autoimmunity and dysfunction: a systematic review and meta-analysis. Front Immunol. 2019;10:1–11.
Lecube A, Zafon C, Gromaz A, Fort JM, Caubet E, Baena JA, et al. Iodine deficiency is higher in morbid obesity in comparison with late after bariatric surgery and non-obese women. Obes Surg. 2015;25:85–89.
Poston L, Bell R, Croker H, Flynn AC, Godfrey KM, Goff L, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. lancet Diabetes Endocrinol. 2015;3:767–77.
Briley AL, Barr S, Badger S, Bell R, Croker H, Godfrey KM, et al. A complex intervention to improve pregnancy outcome in obese women; the UPBEAT randomised controlled trial. BMC Pregnancy Childbirth. 2014;14:74.
Flynn AC, Seed PT, Patel N, Barr S, Bell R, Briley AL, et al. Dietary patterns in obese pregnant women; Influence of a behavioral intervention of diet and physical activity in the UPBEAT randomized controlled trial. Int J Behav Nutr Phys Act. 2016;13:1–12.
Sandell EB, Kolthoff IM. Micro determination of iodine by a catalytic method. Mikrochim Acta. 1937;1:9–25.
Bartels H, Böhmer M. Eine Mikromethode zur Kreatininbestimmung [Micro-determination of creatinine]. Clin Chim Acta. 1971;32:81–5.
Middleton DRS, Watts MJ, Lark RM, Milne CJ, Polya DA. Assessing urinary flow rate, creatinine, osmolality and other hydration adjustment methods for urinary biomonitoring using NHANES arsenic, iodine, lead and cadmium data. Environ Heal A Glob Access Sci Source. 2016;15:1–13.
Bath SC, Furmidge-Owen VL, Redman CW, Rayman MP. Gestational changes in iodine status in a cohort study of pregnant women from the United Kingdom: season as an effect modifier. Am J Clin Nutr. 2015;101:1180–7.
Gallery EDM, Ross M, Gyory AZ. 24-hour urinary creatinine excretion is not altered in human pregnancy. Hypertens Pregnancy. 1996;15:257–61.
Snart C, Threapleton D, Keeble C, Taylor E, Waiblinger D, Reid S, et al. Maternal iodine status, intrauterine growth, birth outcomes and congenital anomalies in a UK birth cohort. BMC Med. 2020;18:1–11.
Vanderpump MPJ, Lazarus JH, Smyth PP, Laurberg P, Holder RL, Boelaert K, et al. Iodine status of UK schoolgirls: A cross-sectional survey. Lancet. 2011;377:2007–12.
Bath SC, Walter A, Taylor A, Wright J, Rayman MP. Iodine deficiency in pregnant women living in the South East of the UK: The influence of diet and nutritional supplements on iodine status. Br J Nutr. 2014;111:1622–31.
Kibirige MS, Hutchison S, Owen CJ, Delves HT. Prevalence of maternal dietary iodine insufficiency in the north east of England: Implications for the fetus. Arch Dis Child Fetal Neonatal Ed. 2004;89:436–9.
Pearce EN, Lazarus JH, Smyth PPA, He X, Dall’Amico D, Parkes AB, et al. Perchlorate and thiocyanate exposure and thyroid function in first-trimester pregnant women. J Clin Endocrinol Metab. 2010;95:3207–15.
The Scientific Advisory Committee. SACN statement on iodine and health. he Scientific Advisory Committee; 2014. pp. 1–44.
Vitamin supplementation in pregnancy. Drug Ther Bull. 2016;54:81–84. https://pubmed.ncbi.nlm.nih.gov/27405305/.
Dold S, Zimmermann MB, Jukic T, Kusic Z, Jia Q, Sang Z, et al. Universal salt iodization provides sufficient dietary iodine to achieve adequate iodine nutrition during the first 1000 days: a cross-sectional multicenter study. J Nutr. 2018;148:587–98.
Agarwal S, Reider C, Brooks JR, Fulgoni VL. Comparison of prevalence of inadequate nutrient intake based on body weight status of adults in the United States: An Analysis of NHANES 2001–2008. J Am Coll Nutr. 2015;34:126–34.
García OP, Long KZ, Rosado JL. Impact of micronutrient deficiencies on obesity. Nutr Rev. 2009;67:559–72.
Rifas-Shiman SL, Rich-Edwards JW, Kleinman KP, Oken E, Gillman MW. Dietary quality during pregnancy varies by maternal characteristics in Project Viva: a US cohort. J Am Diet Assoc. 2009;109:1004–11.
Tsigga M, Filis V, Hatzopoulou K, Kotzamanidis C, Grammatikopoulou MG. Healthy Eating Index during pregnancy according to pre-gravid and gravid weight status. Public Health Nutr. 2011;14:290–6.
Moran LJ, Sui Z, Cramp CS, Dodd JM. A decrease in diet quality occurs during pregnancy in overweight and obese women which is maintained post-partum. Int J Obes (Lond). 2013;37:704–11.
Bouga M, Lean MEJ, Combet E. Iodine and pregnancy-a qualitative study focusing on dietary guidance and information. Nutrients. 2018;10. https://doi.org/10.3390/nu10040408.
Northstone, K., Emmett, P. & Rogers, I. Dietary patterns in pregnancy and associations with socio-demographic and lifestyle factors. Eur J Clin Nutr. 2008;62:471–9.
Brantsæter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant norwegian women. J Nutr. 2009;139:1162–8.
Fuse Y, Shishiba Y, Irie M. Gestational changes of thyroid function and urinary iodine in thyroid antibody-negative Japanese women. Endocr J. 2013;60:1095–106.
Knudsen N, Christiansen E, Brandt-Christensen M, Nygaard B, Perrild H. Age- and sex-adjusted iodine/creatinine ratio. A new standard in epidemiological surveys? Evaluation of three different estimates of iodine excretion based on casual urine samples and comparison to 24h values. Eur J Clin Nutr. 2000;54:361–3.
Moreno-Reyes R, Glinoer D, Van Oyen H, Vandevijvere S. High prevalence of thyroid disorders in pregnant women in a mildly iodine-deficient country: a population-based study. J Clin Endocrinol Metab. 2013;98:3694–701.
Acknowledgements
JF was supported by the Medical Research Council (grant number MR/R019177/1). KVD is supported by the British Heart Foundation FS/17/71/32953. SLW, LP and ACF are supported by Tommy’s charity. LP is supported by the Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and Kings College London. KMG is supported by the UK Medical Research Council (MC_UU_12011/4), the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515-10042), NIHR Southampton 1000DaysPlus Global Nutrition Research Group (17/63/154) and NIHR Southampton Biomedical Research Centre (IS-BRC-1215-20004)), the European Union (Erasmus + Programme Early Nutrition eAcademy Southeast Asia-573651-EPP-1-2016-1-DE-EPPKA2-CBHE-JP and ImpENSA 598488-EPP-1-2018-1-DE-EPPKA2-CBHE-JP), British Heart Foundation (RG/15/17/3174) and the US National Institute On Aging of the National Institutes of Health (Award No. U24AG047867).
Author information
Authors and Affiliations
Contributions
ACF and JF conceived of the study. ACF, JF, CG and AB designed the study. KVD and ACF analysed the data. JF, KVD, SLW and ACF interpreted the data. JF, KVD and ACF wrote the manuscript. LP, JHL, KMG contributed to data interpretation and provided feedback on the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
KMG has received reimbursement for speaking at conferences sponsored by companies selling nutritional products, and is part of an academic consortium that has received research funding from Abbott Nutrition, Nestec, BenevolentAI Bio Ltd. and Danone. The other authors report no potential conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farebrother, J., Dalrymple, K.V., White, S.L. et al. Iodine status of pregnant women with obesity from inner city populations in the United Kingdom. Eur J Clin Nutr 75, 801–808 (2021). https://doi.org/10.1038/s41430-020-00796-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00796-z
This article is cited by
-
Iodine status in pregnant women and infants in Finland
European Journal of Nutrition (2022)
-
Nutritional iodine status and obesity
Thyroid Research (2021)