Abstract
Objectives
To investigate the possible associations of muscle and visceral fat mass with the prognosis of patients hospitalized with acute pancreatitis.
Methods
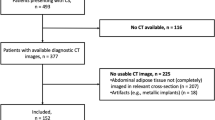
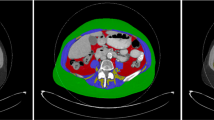
Body composition analysis (Sliceomatic, TomoVision, Montreal, Canada) was performed on CT images at the L3 level in patients admitted with acute pancreatitis during 2008–2014. Regression analysis was used to examine associations of body composition with 1-year mortality and 1-year readmission rates.
Results
A total of 158 patients were included (mean age 63.7 ± 17.4 years, 91 (57.6%) were male). Fat was the most abundant tissue (408 ± 180 cm2 surface area). None of the prognostic factors examined were associated with 1-year mortality. Values below compared to above the medians for muscle mass and visceral fat were associated with higher mean 1-year readmissions: 1.7 versus 1.0, p = 0.02 and 1.6 versus 1.1, p = 0.09, respectively. Logistic regression analysis showed an association of high visceral fat with reduced 1-year readmission (OR 0.995, 95% CI 0.991–1.000, p = 0.03). Linear regression analysis showed an inverse correlation of visceral fat mass with the number of 1-year readmissions (HR −0.004, 95% CI −0.008–000, p = 0.070).
Conclusions
Higher amounts of visceral fat and muscle mass were positively associated with lower recurrent hospitalizations in patients admitted with acute pancreatitis. These results support the importance of nutritional rehabilitation in patients after admission due to acute pancreatitis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–87.
Gapp J, Hall AG, Walters RW, Jahann D, Kassim T, Reddymasu S. Trends and outcomes of hospitalizations related to acute pancreatitis: epidemiology from 2001 to 2014 in the United States. Pancreas. 2019;48:548–54.
Brindise E, Elkhatib I, Kuruvilla A, Silva R. Temporal trends in incidence and outcomes of acute pancreatitis in hospitalized patients in the United States from 2002 to 2013. Pancreas. 2019;48:169–75.
Garg SK, Campbell JP, Anugwom C, Wadhwa V, Singh R, Gupta N, et al. Incidence and predictors of readmissions in acute pancreatitis: a nationwide analysis. Pancreas. 2018;47:46–54.
Mok SR, Mohan S, Elfant AB, Judge TA. The acute physiology and chronic health evaluation iv, a new scoring system for predicting mortality and complications of severe acute pancreatitis. Pancreas. 2015;44:1314–9.
Basit H, Ruan GJ, Mukherjee S Ranson Criteria. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019–2019.
Al-Qahtani HH, Alam MKH, Waheed M. Comparison of harmless acute pancreatitis score with ranson’s score in predicting the severity of acute pancreatitis. J Coll Phys Sug Pak. 2017;27:75–79.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
MacDonald AJ, Greig CA, Baracos V. The advantages and limitations of cross-sectional body composition analysis. Curr Opin Support Palliat Care. 2011;5:342–9.
Hajibandeh S, Hajibandeh S, Jarvis R, Bhogal T, Dalmia S Meta-analysis of the effect of sarcopenia in predicting postoperative mortality in emergency and elective abdominal surgery. Surgeon. 2018. pii: S1479-666X(18)30119-7.
Hamidi M, Ho C, Zeeshan M, O’Keeffe T, Hamza A, Kulvatunyou N, et al. Can sarcopenia quantified by computed tomography scan predict adverse outcomes in emergency general surgery? J Surg Res. 2019;235:141–7.
Leibovitz E, Ben-David N, Shibanov L, Elias S, Shimonov M. Visceral adiposity but not subcutaneous fat associated with improved outcome of patients with acute cholecystitis. J Surg Res. 2018;225:15–20.
Hall TC, Stephenson JS, Jones MJ, Ngu WS, Horsfield MA, Rajesh A, et al. Is abdominal fat distribution measured by axial CT imaging an indicator of complications and mortality in acute pancreatitis. J Gastroint Surg. 2015;19:2126–31.
Sadr-Azodi O, Orsini N, Andrén-Sandberg Å, Wolk A. Abdominal and total adiposity and the risk of acute pancreatitis: a population-based prospective cohort study. Am J Gastroenterol. 2013;108:133–9.
Natu A, Stevens T, Kang L, Yasinow S, Mansoor E, Lopez R, et al. visceral adiposity predicts severity of acute pancreatitis. Pancreas. 2017;46:776–81.
Wells JCK. Using body composition assessment to evaluate the double burden of malnutrition. Ann Nutr Metab. 2019;75:103–8.
Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31:345–50.
Somekawa S, Mine T, Ono K, Hayashi N, Obuchi S, Yoshida H, et al. Relationship between sensory perception and frailty in a community-dwelling elderly population. J Nutr Health Aging. 2017;21:710–4.
Gentile S, Lacroix O, Durand AC, Cretel E, Alazia M, Sambuc R, et al. Malnutrition: a highly predictive risk factor of short-term mortality in elderly presenting to the emergency department. J Nutr Health Aging. 2013;17:290–4.
Moran RA, García-Rayado G, de la Iglesia-García D, Martínez-Moneo E, Fort-Martorell E, Lauret-Braña E, et al. Influence of age, body mass index and comorbidity on major outcomes in acute pancreatitis, a prospective nation-wide multicentre study. United Eur Gastroenterol J. 2018;6:1508–18.
Choi JS, Yi SW, Park JW, Lee S, Jeong SH, Yi JJ, et al. Body mass index and the risk of acute pancreatitis by etiology: a prospective analysis of Korean National Screening Cohort. J Gastroenterol Hepatol. 2019;34:603–11.
Wells JCK. The capacity-load model of non-communicable disease risk: understanding the effects of child malnutrition, ethnicity and the social determinants of health. Eur J Clin Nutr. 2018;72:688–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shimonov, M., Abtomonova, Z., Groutz, A. et al. Associations between body composition and prognosis of patients admitted because of acute pancreatitis: a retrospective study. Eur J Clin Nutr 75, 817–822 (2021). https://doi.org/10.1038/s41430-020-00789-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00789-y
This article is cited by
-
Automatic quantitative evaluation of normal pancreas based on deep learning in a Chinese adult population
Abdominal Radiology (2022)