Abstract
Background/objectives
Major causes of hip fractures are osteoporosis and falls, both of which are determined by nutrition. Information on the nutritional status of patients admitted to hospital with a hip fracture is lacking. In this study, we assessed determinants and adverse outcomes associated with malnutrition and malnourishment.
Methods
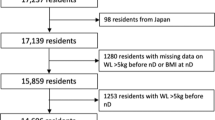
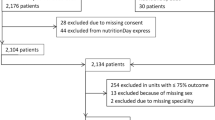
Nutritional status, assessed using the Malnutrition Universal Screening Tool protocol, was compared to age and residency prior to admission, and outcomes during hospital stay and at discharge.
Results
A total of 1239 patients admitted with a hip fracture (349 men, 890 women), aged 60–100 years. Compared with well-nourished individuals, the prevalences of malnutrition risk or malnourishment were higher in older age groups and those from residential or nursing care. Those with risk of malnutrition or malnourishment stayed in hospital longer by 3.0 days (95% confidence interval (CI), 1.5–4.5 days; p < 0.001) and 3.1 days (95% CI, 0.7–5.5 days; p = 0.011), respectively. Compared with the well-nourished group, malnourished individuals had increased: (1) risk for failure to mobilise within 1 day of surgery (rates = 17.9 versus 27.0%; odds ratio (OR) = 1.6 (95% CI, 1.0–2.7), p = 0.045); (2) pressure ulcers (rates = 1.0% versus 5.0%; OR = 5.5 (95% CI, 1.8–17.1), p = 0.006); (3) in-patient mortality (rates = 4.5% versus 10.1%; OR = 2.3 (95% CI, 1.1–4.8) p = 0.033) and (4) discharge to residential/nursing care: rates = 4.3% versus 11.1%; OR = 2.8 (95% CI, 1.2–6.6), p = 0.022.
Conclusions
Inadequate nutrition is common in patients admitted to hospital with a hip fracture, which in turn predisposes them to a number of complications. More research on nutritional support should be directed to this group to prevent or minimise hip fractures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458–60.
Rapp K, Büchele G, Dreinhöfer K, Bücking B, Becker C, Benzinger P. Epidemiology of hip fractures. Z Gerontol Geriatr. 2019;52:10–6.
Hagen G, Magnussen J, Tell G, Omsland T. Estimating the future burden of hip fractures in Norway. A NOREPOS study. Bone. 2020;131:115156.
Greenspan SL, Myers ER, Kiel DP, Parker RA, Hayes WC, Resnick NM. Fall direction, bone mineral density, and function: risk factors for hip fracture in frail nursing home elderly. Am J Med. 1998;104:539–45.
Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000;48:883–93.
Cannarella R, Barbagallo F, Condorelli RA, Aversa A, La Vignera S, Calogero AE. Osteoporosis from an endocrine perspective: the role of hormonal changes in the elderly. J Clin Med. 2019;8:1564.
Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57:492–8.
Lord SR, Ward JA, Williams P, Anstey KJ. An epidemiological study of falls in older community‐dwelling women: the Randwick falls and fractures study. Aust J Public Health. 1993;17:240–5.
Buchner DM, Larson EB. Falls and fractures in patients with Alzheimer-type dementia. JAMA. 1987;257:1492–5.
Tromp AM, Smit JH, Deeg DJ, Bouter LM, Lips PT. Predictors for falls and fractures in the Longitudinal Aging Study Amsterdam. J Bone Min Res. 1998;13:1932–9.
Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15:22–6.
Pigłowska M, Kostka J, Kostka T. Association between respiratory tract infections and incidence of falls in nursing home residents. Pol Arch Med Wewn. 2013;123:371–7.
Verlaan S, Ligthart-Melis GC, Wijers SL, Cederholm T, Maier AB, de van der Schueren MA. High prevalence of physical frailty among community-dwelling malnourished older adults–a systematic review and meta-analysis. J Am Med Dir Assoc. 2017;18:374–82.
Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, et al. Nutritional status and nutritional treatment are related to outcomes and mortality in older adults with hip fracture. Nutrients 2018;10:555.
Koren-Hakim T, Weiss A, Hershkovitz A, Otzrateni I, Grosman B, Frishman S, et al. The relationship between nutritional status of hip fracture operated elderly patients and their functioning, comorbidity and outcome. Clin Nutr. 2012;31:917–21.
Goisser S, Schrader E, Singler K, Bertsch T, Gefeller O, Biber R, et al. Malnutrition according to mini nutritional assessment is associated with severe functional impairment in geriatric patients before and up to 6 months after hip fracture. J Am Med Dir Assoc. 2015;16:661–7.
Lisk R, Uddin M, Parbhoo A, Yeong K, Fluck D, Sharma P, et al. Predictive model of length of stay in hospital among older patients. Aging Clin Exp Res. 2019;31:993–9.
Lisk R, Yeong K, Enwere P, Jenkinson J, Robin J, Irvin-Sellers M, et al. Associations of 4AT with mobility, length of stay and mortality in hospital and discharge destination among patients admitted with hip fractures. Age Ageing. 2020;49:411–7.
Royal College of Physicians. National Hip Fracture Database annual report 2017. London: RCP; 2017. http://www.nhfd.co.uk/. Accessed 1 Feb 2019.
Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database National report 2013. Prepared on behalf of the Clinical Effectiveness and Evaluation Unit at the Royal College of Physicians. https://www.nhfd.co.uk/20/hipfractureR.nsf/945b5efcb3f9117580257ebb0069c820/566c6709d04a865780257bdb00591cda/$FILE/onlineNHFDreport.pdf.
Kondrup JE, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
National Institute for Health and Care Excellence Hip fracture in adults. Manchester: NICE; 2012. NICE quality standard No 16.
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14–7.
Kiesswetter E, Pohlhausen S, Uhlig K, Diekmann R, Lesser S, Heseker H, et al. Malnutrition is related to functional impairment in older adults receiving home care. J Nutr Health Aging. 2013;17:345–50.
Söderström L, Rosenblad A, Adolfsson ET, Bergkvist L. Malnutrition is associated with increased mortality in older adults regardless of the cause of death. Br J Nutr. 2017;117:532–40.
Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:1734–8.
Chavarro-Carvajal D, Reyes-Ortiz C, Samper-Ternent R, Arciniegas AJ, Gutierrez CC. Nutritional assessment and factors associated to malnutrition in older adults: a cross-sectional study in Bogotá, Colombia. J Aging Health. 2015;27:304–19.
Neumann SA, Miller MD, Daniels L, Crotty M. Nutritional status and clinical outcomes of older patients in rehabilitation. J Hum Nutr Diet. 2005;18:129–36.
Galivanche AR, Kebaish KJ, Adrados M, Ottesen TD, Varthi AG, Rubin LE, et al. Postoperative pressure ulcers after geriatric hip fracture surgery are predicted by defined preoperative comorbidities and postoperative complications. J Am Acad Orthop Surg. 2020;28:342–51.
Lindholm C, Sterner E, Romanelli M, Pina E, Torra y Bou J, Hietanen H, et al. Hip fracture and pressure ulcers—the Pan‐European Pressure Ulcer Study—intrinsic and extrinsic risk factors. Int Wound J. 2008;5:315–28.
Jones A, Pope J, Anguah KO, Erickson D. Mini Nutritional Assessment Score as a potential predictor of pressure ulcers in elderly nursing home patients with dementia. Top Clin Nutr. 2020;35:42–9.
Hedström M, Ljungqvist O, Cederholm T. Metabolism and catabolism in hip fracture patients nutritional and anabolic intervention—a review. Acta Orthopaedica. 2006;77:741–7.
Bell JJ, Bauer JD, Capra S, Pulle RC. Multidisciplinary, multi-modal nutritional care in acute hip fracture inpatients—results of a pragmatic intervention. Clin Nutr. 2014;33:1101–7.
Li HJ, Cheng HS, Liang J, Wu CC, Shyu YI. Functional recovery of older people with hip fracture: does malnutrition make a difference? J Adv Nurs. 2013;69:1691–703.
Gunnarsson AK, Lönn K, Gunningberg L. Does nutritional intervention for patients with hip fractures reduce postoperative complications and improve rehabilitation? J Clin Nurs. 2009;18:1325–33.
Houwing RH, Rozendaal M, Wouters-Wesseling W, Beulens JW, Buskens E, Haalboom JR. A randomised, double-blind assessment of the effect of nutritional supplementation on the prevention of pressure ulcers in hip-fracture patients. Clin Nutr. 2003;22:401–5.
Espaulella J, Guyer H, Diaz-Escriu F, Mellado-Navas JA, Castells MO, Pladevall MA. Nutritional supplementation of elderly hip fracture patients. A randomized, double-blind, placebo-controlled trial. Age Ageing. 2000;29:425–31.
Bruce D, Laurance I, McGuiness M, Ridley M, Goldswain P. Nutritional supplements after hip fracture: poor compliance limits effectiveness. Clin Nutr. 2003;22:497–500.
Lawson RM, Doshi MK, Ingoe LE, Colligan JM, Barton JR, Cobden I. Compliance of orthopaedic patients with postoperative oral nutritional supplementation. Clin Nutr. 2000;19:171–5.
Philipson TJ, Snider JT, Lakdawalla DN, Stryckman B, Goldman DP. Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care. 2013;19:121–8.
Barr J, Hecht M, Flavin KE, Khorana A, Gould MK. Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest. 2004;125:1446–57.
Han TS, Lean ME, Fluck D, Affley B, Gulli G, Patel T, et al. Impact of delay in early swallow screening on pneumonia, length of stay in hospital, disability and mortality in acute stroke patients. Eur J Clin Nutr. 2018;72:1548–54.
McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ. 1994;308:945–8.
Koren-Hakim T, Weiss A, Hershkovitz A, Otzrateni I, Anbar R, Nevo RF, et al. Comparing the adequacy of the MNA-SF, NRS-2002 and MUST nutritional tools in assessing malnutrition in hip fracture operated elderly patients. Clin Nutr. 2016;35:1053–8.
Acknowledgements
We are grateful to all patients who participated in this NHFD Audit Programme and hospital staff who provided clinical care and support to patients throughout their hospital stay.
Author information
Authors and Affiliations
Contributions
TSH reviewed the topic related literature and conceived the original idea. KY and RL performed the study coordination and data collection. TSH wrote the first draft, analysed, interpreted the data and revised the paper. CHF and DF edited the paper. All authors checked, interpreted the results and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Han, T.S., Yeong, K., Lisk, R. et al. Prevalence and consequences of malnutrition and malnourishment in older individuals admitted to hospital with a hip fracture. Eur J Clin Nutr 75, 645–652 (2021). https://doi.org/10.1038/s41430-020-00774-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00774-5
This article is cited by
-
Changes in Characteristics and Outcomes of Patients Undergoing Surgery for Hip Fractures Following the Initiation of Orthogeriatric Service: Temporal Trend Analysis
Calcified Tissue International (2022)
-
Influence of Nutritional Status on a Family-Centered Care Intervention for Older Adults with Cognitive Impairment following Hip-Fracture Surgery: Secondary Data Analysis of a Randomized Controlled Trial
The Journal of nutrition, health and aging (2022)
-
Clinical outcomes in patients admitted to hospital with cervical spine fractures or with hip fractures
Internal and Emergency Medicine (2021)