Abstract
Background/Objectives
Adequate dietary intake for type 2 diabetes mellitus (T2DM) patients is central in preventing or delaying onset of diabetes related complications. This study used dietary serving scores (DSS) to determine the adequacy of dietary intake and associated factors among patients with T2DM in Kampala.
Subjects/Methods
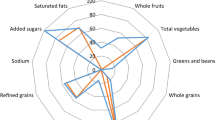
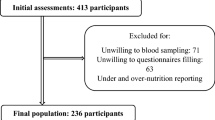
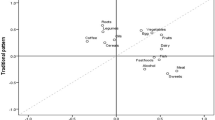
A facility based cross-sectional study among adult T2DM patients attending diabetes clinics attached to health care facilities in Kampala was conducted. Semi structured demographic and 7-day Food Frequency Questionnaires (FFQ) were used to collect data on sociodemographic characteristics, environmental factors and dietary intake respectively. Dietary intake was computed using Dietary Serving Scores (DSS) and was grouped into two: “adequate dietary intake (DSS of 78 and above)” and “inadequate dietary intake (DSS below 78)”. Multiple linear regression was used to assess correlates of dietary intake.
Results
Out of the 400 participants, only 49 (12.25%; 95% CI: 9.04, 15.46) were classified as having adequate dietary intake. After adjusting for potential confounders, unmarried individuals (β = −2.367; p = 0.024) and those who are salaried (β = −3.162; p = 0.012) or self-employed (β = −4.214; p = 0.001) had significantly lower mean DSS compared to their respective counterparts. T2DM patients who attended Nsambya hospital diabetes clinic had significantly higher mean DSS (β = 3.698; p = 0.022) compared to those who receive treatment in Lubaga hospital.
Conclusions
The prevalence of adequate dietary intake among patients with T2DM attending health facilities in Kampala is very low. More efforts are needed to educate patients on better dietary choices aligned with disease management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Datasets generated and analysed during the study are not publicly available due to terms of participant consent but are available in anonymised form from the corresponding author on reasonable request.
References
Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, et al. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–30.
Roglic G. WHO Global report on diabetes: a summary. Int J Noncommun Dis. 2016;1:3.
M.O.H. National NCDs risk survey. Uganda: Ministry of Health; 2014.
Serrano-Gil M, Jacob S. Engaging and empowering patients to manage their type 2 diabetes, Part I: a knowledge, attitude, and practice gap? Adv Ther. 2010;27:321–33.
Kibirige D, Atuhe D, Sebunya R, Mwebaze R. Suboptimal glycaemic and blood pressure control and screening for diabetic complications in adult ambulatory diabetic patients in Uganda: a retrospective study from a developing country. J Diabetes Metab Disord. 2014;13:40.
ADA. American Diabetes Association, food pyramid for patients with diabetes. American Diabetes Association; 2014.
IDF. Diabetes in Africa. International Diabetes Federation; 2015.
Tiew KF, Chan YM, Lye MS, Loke SC. Factors associated with dietary diversity score among individuals with type 2 diabetes mellitus. J Health Popul Nutr. 2014;32:665–76.
Ganiyu AB, Mabuza LH, Malete NH, Govender I, Ogunbanjo GA. Non-adherence to diet and exercise recommendations amongst patients with type 2 diabetes mellitus attending Extension II Clinic in Botswana: original research. Afr J Prim Health Care Fam Med. 2013;5:1–6.
Firouzi S, Barakatun-Nisak MY, Azmi KN. Nutritional status, glycemic control and its associated risk factors among a sample of type 2 diabetic individuals, a pilot study. J Res Med Sci. 2015;20:40.
García-Pérez L-E, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4:175–94.
WHO. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. World Health Organization: Geneva; 2006.
Kish L. Survey sampling. New York: John Wiley and Sons Inc.; 1965.
Kabagenyi A, Habaasa G, Rutaremwa G. Low Contraceptive Use among Young Females in Uganda: Does Birth History and Age at Birth have an Influence? Analysis of 2011 Demographic and Health Survey. J Contracept Stud. 2016;1:4.
Monteagudo C, Mariscal-Arcas M, Rivas A, Lorenzo-Tovar ML, Tur JA, Olea-Serrano F. Proposal of a mediterranean diet serving score. PLoS ONE. 2015;10:e0128594.
Rathnayake KM, Madushani P, Silva K. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res Notes. 2012;5:469.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5.
Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 2018;361:k2234.
Moubarac J-C, Parra DC, Cannon G, Monteiro CA. Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep. 2014;3:256–72.
Kennedy GL, Pedro MR, Seghieri C, Nantel G, Brouwer I. Dietary diversity score is a useful indicator of micronutrient intake in non-breast-feeding Filipino children. J Nutr. 2007;137:472–7.
Hilton CE. The importance of pretesting questionnaires: a field research example of cognitive pretesting the Exercise referral Quality of Life Scale (ER-QLS). Int J Soc Res Methodol. 2017;20:21–34.
Zhang Z. Model building strategy for logistic regression: purposeful selection. Ann Transl Med. 2016;4:9.
Matovu N, Matovu FK, Sseguya W, Tushemerirwe F. Association of dietary intake and BMI among newly diagnosed type 2 diabetes patients attending diabetic clinics in Kampala. BMC Nutr. 2017;3:21.
Cohen DA, Bhatia R. Nutrition standards for away-from-home foods in the United States. Obes Rev. 2012;13:618–29.
Antonio JP, Sarmento RA, de Almeida JC. Diet quality and glycemic control in patients with type 2 diabetes. J Acad Nutr Diet. 2019;119:652–8.
Fujii H, Iwase M, Ohkuma T, Ogata-Kaizu S, Ide H, Kikuchi Y, et al. Impact of dietary fiber intake on glycemic control, cardiovascular risk factors and chronic kidney disease in Japanese patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. Nutr J. 2013;12:159.
Brandão-Lima PN, Carvalho GBD, RKF Santos, Bdc Santos, Dias-Vasconcelos NL, Vds Rocha, et al. Intakes of zinc, potassium, calcium, and magnesium of individuals with type 2 diabetes mellitus and the relationship with glycemic control. Nutrients. 2018;10:1948.
Kyokunzire C, Matovu N. Factors associated with adherence to diabetes care recommendations among children and adolescents with type 1 diabetes: a facility-based study in two urban diabetes clinics in Uganda. Diabetes Metab Syndr Obes. 2018;11:93.
Werfalli MM, Kalula SZ, Manning K, Levitt NS. Does social support effect knowledge and diabetes self-management practices in older persons with Type 2 diabetes attending primary care clinics in Cape Town, South Africa? PLoS ONE. 2020;15:e0230173.
WDF. Optimising Care through Integrating NCD Services in Primary Care, WDF19-1721 Bagsværd: World Diabetes Foundation 2012. https://bit.ly/324gjDP.
Bahendeka S, Mutungi G, Tugumisirize F, Kamugisha A, Nyangabyaki C, Wesonga R, et al. Healthcare delivery for paediatric and adolescent diabetes in low resource settings: type 1 diabetes clinics in Uganda. Glob Public Health. 2019;14:1869–83.
Acknowledgements
We thank the staff of Mulago, Lubaga, Nsambya, Kisenyi and Naguru hospitals for their support and cooperation during the period of data collection. We further extend our appreciation to the staff of Makerere University School of Public Health for their support during the study. We would also like to extend our thanks to the study participants and research assistants for their time and cooperation during the period of data collection. Statistical support from Dr. Finian Bannon of the Centre for Public Health, Queen’s University Belfast, is highly appreciated.
Funding
This study received funding from Germany Academic Exchange service (DAAD) as a contribution towards research for SK. The funders had no role in any aspect of the study i.e. study design, data collection, data analysis and interpretation and the decision to publish or preparing and submission of the manuscript.
Author information
Authors and Affiliations
Contributions
SK, DG and RK contributed to the conceptualisation and design of the study; SK and NM designed research tools and assisted in data collection; SK and NM analysed and interpreted the data. SK and NM wrote the first draft of the manuscript. DG and RK reviewed the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval to conduct the study was sought from MakSPH Health Higher Degrees Research and Ethics Committee. Permission to collect data was sought from the five health facilities.
Informed consent
Verbal and written informed consent in the local language was obtained from the respondents and collected information was kept confidential. The investigator provided an explanation of the purpose, risks and benefits of the study to the participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kisaakye, S., Matovu, N., Guwatudde, D. et al. Using dietary serving scores to assess adequacy of dietary intake and associated factors among adult patients with type 2 diabetes in Kampala: a cross-sectional study. Eur J Clin Nutr 75, 555–563 (2021). https://doi.org/10.1038/s41430-020-00731-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00731-2