Abstract
Background/objectives
Despite best practice guidelines, feeding methods after colorectal surgery vary due to the difficulties translating evidence into practice. The aim was to determine the effectiveness of diets delivered into the gastrointestinal tract (GIT) on gut motility following colorectal surgery.
Subjects/methods
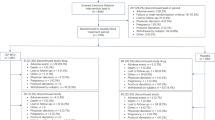
EMBASE, MEDLINE, CINAHL, Web of Science and PubMed were systematically searched. Randomised controlled trials investigating effectiveness of a diet on gut motility after colorectal surgeries were included. Outcomes included postoperative ileus, length of stay, mortality, nausea and vomiting.
Results
A total of 756 potential studies were identified; of these, 10 trials reporting on 1237 unique patients were included. There is evidence that early feeding reduces time (days) to first flatus (mean difference (MD):−0.64; 95% CI:−0.84 to −0.44) and bowel movements (MD:−0.64; 95% CI:−1.01 to −0.26), when compared to traditional postoperative fasting. Introducing solids versus the progression of fluids to solids had no effect on time (days) to first flatus (MD:0.13; 95% CI:−1.99 to 1.74) or bowel movement (MD:0.20; 95% CI:−0.50 to 0.98). Complete nutrition compared to hypocaloric nutrition had no effect on time to first flatus (MD:−0.60; 95% CI:−1.66 to 0.46) or bowel movement (MD:−0.20; 95% CI:−1.59 to 1.19), whereas coffee and diet compared to water and diet significantly decreased time (days) to first bowel movement (MD:−0.60; 95% CI:−0.97 to −0.19) but had no effect on time to first flatus (MD:−0.20; 95% CI:−0.57 to 0.09).
Conclusions
Any form of early postoperative diet provided into the GIT early after colorectal surgery is likely to stimulate gut motility, resulting in earlier return of bowel function and shorter length of stay.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev 2006; Cd004080. https://doi.org/10.1002/14651858.CD004080.pub2.
Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009;13:569–75.
Lewis SJ, Egger M, Sylvester PA, Thomas S. Early enteral feeding versus “nil by mouth” after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. Brit Med J. 2001;323:773–6.
Osland E, Yunus RM, Khan S, Memon MA. Early versus traditional postoperative feeding in patients undergoing resectional gastrointestinal surgery: a meta-analysis. JPEN J Parent Enter Nutr. 2011;35:473–87. https://doi.org/10.1177/0148607110385698. 2
Zhuang CL, Ye XZ, Zhang CJ, Dong QT, Chen BC, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225–32. https://doi.org/10.1159/000353136.
Bernardes LFM, Diogo A. Early enteral feeding after upper digestive tract surgeries and clinical assessment of post-operative ileus. Biosci J. 2008;24:100–7.
Flores-Funes D, Campillo-Soto A, Pellicer-Franco E, Aguayo-Albasini JL. The use of coffee, chewing-gum and gastrograffin in the management of postoperative ileus: a review of current evidence. Cirugia Esp. 2016;94:495–501. https://doi.org/10.1016/j.ciresp.2016.05.020.
Kasparek MS, Mueller MH, Glatzle J, Enck P, Becker HD, Zittel TT, et al. Postoperative colonic motility increases after early food intake in patients undergoing colorectal surgery. Surgery. 2004;136:1019–27. https://doi.org/10.1016/j.surg.2004.03.011.
Gianotti L, Nespoli L, Panelli M, Nespoli A. Early oral feeding after colorectal resection is safe and feasible also outside a fast track programme. Surg Infect. 2011;12:A11. https://doi.org/10.1089/sur.2011.9918.
Russ A, Stein S, Crawshaw B, Champagne B. Improved postoperative outcomes with a modified GI diet after laparoscopic colorectal resection. Dis Colon Rectum. 2014;57:e318–e319.
Funder JA, Tolstrup R, Jepsen BN, Iversen LH. Postoperative paralytic ileus remains a problem following surgery for advanced pelvic cancers. J Surg Res. 2017;218:167–73.
Story SK, Chamberlain RS. A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig Surg. 2009;26:265–75. https://doi.org/10.1159/000227765.
Murphy MM, Tevis SE, Kennedy GD. Independent risk factors for prolonged postoperative ileus development. J Surg Res. 2016;201:279–85. https://doi.org/10.1016/j.jss.2015.10.047.
Chapman SJ, Thorpe G, Vallance AE, Harji DP, Lee MJ, Fearnhead NS, et al. Systematic review of definitions and outcome measures for return of bowel function after gastrointestinal surgery. Bjs Open. 2019;3:1–10. https://doi.org/10.1002/bjs5.102.
van Bree SH, Bemelman WA, Hollmann MW, Zwinderman AH, Matteoli G, El Temna S, et al. Identification of clinical outcome measures for recovery of gastrointestinal motility in postoperative ileus. Ann Surg. 2014;259:708–14. https://doi.org/10.1097/SLA.0b013e318293ee55.
Chapman SJ, Pericleous A, Downey C, Jayne DG. Postoperative ileus following major colorectal surgery. Br J Surg. 2018;105:797–810. https://doi.org/10.1002/bjs.10781.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 Updated March 2011. The Cochrane Collaboration. Bristol: UK; 2011. http://handbook.cochrane.org.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (Lond, Engl). 2010;8:336–41. https://doi.org/10.1016/j.ijsu.2010.02.007.
Bosio RM, Pigazzi A. Emerging and evolving technology in colon and rectal surgery. Clin Colon Rectal Surg. 2015;28:152–7.
Kim YJ. The future medical science and colorectal surgeons. Ann Coloproctology. 2017;33:207–9.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr (Edinb, Scotl). 2017;36:49–64. https://doi.org/10.1016/j.clnu.2016.09.004.
Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I et al. A Revised Tool for Assessing Risk of Bias in Randomized Trials. In: Chandler J, McKenzie J, Boutron I, Welch V, editors. Cochrane Methods. Cochrane Database of Systematic Reviews. Briston: UK; 2016.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. Brit Med J. 2004;328:1490.
Borenstein M, Hedges L, Higgins J, & Rothstein H. Comprehensive meta-analysis. 3rd edn. Englewood: Biostat; 2013.
da Fonseca LM, da Luz MMP, Lacerda A, Correia M, da Silva RG. A simplified rehabilitation program for patients undergoing elective colonic surgery-randomized controlled clinical trial. Int J Colorectal Dis. 2011;26:609–16. https://doi.org/10.1007/s00384-010-1089-0.
Dag A, Colak T, Turkmenoglu O, Gundogdu R, Aydin S. A randomized controlled trial evaluating early versus traditional oral feeding after colorectal surgery. Clin (Sao Paulo, Braz). 2011;66:2001–5.
El Nakeeb A, Fikry A, El Metwally T, Fouda E, Youssef M, Ghazy H, et al. Early oral feeding in patients undergoing elective colonic anastomosis. Int J Surg. 2009;7:206–9. https://doi.org/10.1016/j.ijsu.2009.03.003.
Feo CV, Romanini B, Sortini D, Ragazzi R, Zamboni P, Pansini GC, et al. Early oral feeding after colorectal resection: a randomized controlled study. ANZ J Surg. 2004;74:298–301. https://doi.org/10.1111/j.1445-1433.2004.02985.x.
Zhou T, Wu XT, Zhou YJ, Huang X, Fan W, Li YC. Early removing gastrointestinal decompression and early oral feeding improve patients’ rehabilitation after. World J Gastroenterol. 2006;12:2459–63. https://doi.org/10.3748/wjg.v12.i15.2459.
Han-Geurts IJ, Hop WC, Kok NF, Lim A, Brouwer KJ, Jeekel J. Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. Br J Surg. 2007;94:555–61. https://doi.org/10.1002/bjs.5753.
Lau C, Phillips E, Bresee C, Fleshner P. Early use of low residue diet is superior to clear liquid diet after elective colorectal surgery a randomized controlled trial. Ann Surg. 2014;260:641–9. https://doi.org/10.1097/sla.0000000000000929.
Soop M, Carlson GL, Hopkinson J, Clarke S, Thorell A, Nygren J, et al. Randomized clinical trial of the effects of immediate enteral nutrition on metabolic responses to major colorectal surgery in an enhanced recovery protocol. Br J Surg. 2004;91:1138–45. https://doi.org/10.1002/bjs.4642. e-pub ahead of print 2004/09/28.
Muller SA, Rahbari NN, Schneider F, Warschkow R, Simon T, von Frankenberg M, et al. Randomized clinical trial on the effect of coffee on postoperative ileus following elective colectomy. Br J Surg. 2012;99:1530–8. https://doi.org/10.1002/bjs.8885.
Boelens PG, FFBM Heesakkers, MDP Luyer, KWY VanBarneveld, IHJT DeHingh, GAP Nieuwenhuijzen, et al. Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg. 2014;259:649–55. https://doi.org/10.1097/SLA.0000000000000288.
Kruse C, Muller SA, Warschkow R, Luthi C, Brunner W, Marti L, et al. Does caffeine reduce postoperative bowel paralysis after elective laparoscopic colectomy? (CaCo trial): study protocol for a randomized controlled trial. Trials. 2016;17:186. https://doi.org/10.1186/s13063-016-1297-1.
Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, et al. ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr. 2006;25:224–44.
Carroll JS, Quijada MA. Redirecting traditional professional values to support safety: changing organisational culture in health care. Qual Saf Health Care. 2004;13(Suppl 2):ii16–21. https://doi.org/10.1136/qhc.13.suppl_2.ii16.
Scott T, Mannion R, Davies HT, Marshall MN. Implementing culture change in health care: theory and practice. Int J Qual Health Care: J Int Soc Qual Health Care. 2003;15:111–8.
Bauer JJ, Gelernt IM, Salky BA, Kreel I. Is routine postoperative nasogastric decompression really necessary? Ann Surg. 1985;201:233–6.
Johnson Casto C, Krammer J, Drake J. Postoperative feeding: a clinical review. Obstet Gynecol Surv. 2000;55:571–3. e-pub ahead of print 2000/09/07.
Silk DB, Gow NM. Postoperative starvation after gastrointestinal surgery. Early feeding is beneficial. Brit Med J. 2001;323:761–2.
Kahokehr A, Sammour T, Zargar-Shoshtari K, Thompson L, Hill AG. Implementation of ERAS and how to overcome the barriers. Int J Surg (Lond, Engl). 2009;7:16–9. https://doi.org/10.1016/j.ijsu.2008.11.004.
Martin D, Roulin D, Grass F, Addor V, Ljungqvist O, Demartines N, et al. A multicentre qualitative study assessing implementation of an Enhanced Recovery After Surgery program. Clin Nutr (Edinb, Scotl). 2018;37(6 Pt A):2172–7. https://doi.org/10.1016/j.clnu.2017.10.017.
Braga M, Gianotti L, Gentilini O, Liotta S, Di Carlo V. Feeding the gut early after digestive surgery: results of a nine-year experience. Clin Nutr (Edinb, Scotl). 2002;21:59–65. https://doi.org/10.1054/clnu.2001.0504. e-pub ahead of print 2002/03/09.
Austin KK, Young JM, Solomon MJ. Quality of life of survivors after pelvic exenteration for rectal cancer. Dis colon rectum. 2010;53:1121–6. https://doi.org/10.1007/DCR.0b013e3181e10c46.
Jakobsson J, Idvall E, Kumlien C Patient characteristics and surgery-related factors associated with patient-reported recovery at 1 and 6 months after colorectal cancer surgery. Eur J Cancer Care. 2017;26:1–11. https://doi.org/10.1111/ecc.12715.
Bekker R, Koole G, Roubos D. Flexible bed allocations for hospital wards. Health Care Manag Sci. 2017;20:453–66.
Buttigieg SC, Abela L, Pace A. Variables affecting hospital length of stay: a scoping review. J health Organ Manag. 2018;32:463–93. https://doi.org/10.1108/jhom-10-2017-0275.
Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102:1884–98. https://doi.org/10.1213/01.ane.0000219597.16143.4d.
Hamilton E, Ravikumar R, Bartlett D, Hepburn E, Hwang M-J, Mirza N, et al. Dexamethasone reduces emesis after major gastrointestinal surgery (DREAMS). Trials. 2013;14:249. https://doi.org/10.1186/1745-6215-14-249.
Liu L, Xie YH, Zhang W, Chai XQ. Effect of transversus abdominis plane block on postoperative pain after colorectal surgery: a meta-analysis of randomized controlled trials. Med Princ Pract. 2018;27:158–65.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design of the study. SH and SC completed the review protocol, the search strategy, screening of potentially eligible studies and extracting and analysing data. SH and DS conducted the meta-regression analysis and created the ‘Summary of Findings’ tables. All authors analysed and interpreted the results. SH was a major contributor of drafting the manuscript and all other authors were involved in revising it critically for important intellectual content. All authors provided final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Search Strategy
Search Strategy
EMBASE and MEDLINE via Ovid | 1. (‘colorectal surgery’/exp OR ‘colorectal surgery’ OR ‘rectum’/exp OR ‘rect*’ OR ‘rect* surgery’).mp. |
2. (‘gastrointestinal motility’/exp OR ‘gastrointestinal motility’ OR ‘recovery of function’/exp or ‘recovery of function’ OR ‘enhanced recovery’ OR ‘fast track’).mp. | |
3. (‘ileus’/exp OR ‘ileus’ OR ‘postoperative ileus’).mp. | |
Web of Knowledge via Web of Science | 1. TOPIC: ‘colorectal surgery’ OR TITLE: ‘colorectal surgery’ OR TOPIC: ‘rect*’ OR TITLE: ‘rect*’ OR TOPIC: ‘rect* surgery’ OR TITLE: ‘rect* surgery’ |
2. TOPIC: ‘gastrointestinal motility’ OR TITLE: ‘gastrointestinal motility’ OR TOPIC: ‘recovery of function’ OR TITLE: ‘recovery of function’ OR TOPIC: ‘enhanced recovery’ OR TITLE: ‘enhanced recovery’ OR TOPIC: ‘fast track* OR TITLE: ‘fast track*’ | |
3. TOPIC: ‘ileus’ OR TITLE: ‘ileus’ OR TOPIC: ‘postoperative ileus’ OR TITLE: ‘postoperative ileus’ | |
Cinahl via Ebsco | 1. ‘colorectal surgery’ OR (MH ‘rectum’) OR ‘rect*’ OR ‘rect* surgery’ |
2. (MH ‘gastrointestinal motility;) OR ‘gastrointestinal motility’ OR ‘recovery of function’ OR ‘enhanced recovery’ OR ‘fast track*’ | |
3. ‘ileus’ OR ‘postoperative ileus’ | |
1. ‘colorectal surgery’[MeSH] OR ‘colorectal surgery’[tiab] OR ‘rectum’[MeSH] OR ‘rect*’ OR ‘rect* surgery’ | |
2. ‘gastrointestinal motility’[MeSH] OR ‘gastrointestinal motility’ OR ‘recovery of function’[MeSH] OR ‘recovery of function’ OR ‘enhanced recovery’ OR ‘fast track’ | |
3. ‘ileus’[MeSH] OR ‘ileus’ OR ‘postoperative ileus’ |
Rights and permissions
About this article
Cite this article
Hogan, S., Steffens, D., Rangan, A. et al. The effect of diets delivered into the gastrointestinal tract on gut motility after colorectal surgery—a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr 73, 1331–1342 (2019). https://doi.org/10.1038/s41430-019-0474-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0474-1
This article is cited by
-
Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons
Surgical Endoscopy (2023)
-
Short-term outcome of diverting loop ileostomy reversals performed by residents: a retrospective cohort prognostic factor study
International Journal of Colorectal Disease (2023)
-
Factors associated with diet failure after colon cancer surgery
Surgical Endoscopy (2022)
-
State-of-the-art colorectal disease: postoperative ileus
International Journal of Colorectal Disease (2021)