Abstract
Background
In patients with chronic intestinal failure (CIF) and long-term home parenteral nutrition (HPN), liver steatosis is a known late complication, which can progress to intestinal failure-associated liver disease (IFALD). Magnetic resonance imaging (MRI) provides a qualitative and quantitative assessment of liver steatosis. The aim of our study was to assess the prevalence of liver steatosis and find possible new factors that could be connected to liver steatosis in CIF patients on HPN therapy.
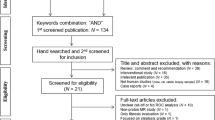
Methods
Patients diagnosed with CIF and undergoing long-term HPN therapy were enrolled in a prospective cohort study. Clinical, laboratory and body composition data were collected from their medical records between January 2017 and November 2018. Liver steatosis was diagnosed using 3 Tesla Siemens MRI scanner. The associations between various risk factors and liver steatosis were calculated using uni- and multivariate logistic regression.
Results
In our study, we included 63 adult patients with CIF on HPN therapy. The median HPN therapy duration was 70 weeks (IQR 22–203). The prevalence of liver steatosis was 28.6%. Serum cholesterol level, CRP and FFMI were statistically significantly associated with liver steatosis.
Conclusion
The results of our study indicate that CIF patients on HPN therapy experience a low risk of liver disease if they adhere to a well-controlled treatment regime. We found that MRI is an appropriate diagnostic tool for monitoring liver steatosis in patients on long-term PN. With respect to already known risk factors for liver steatosis, we did find a newly described association between FFMI and liver steatosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
EASL–EASD–EASO. Clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402. http://linkinghub.elsevier.com/retrieve/pii/S0168827815007345.
Lee SS, Park SH, Kim HJ, Kim SY, Kim M-Y, Kim DY, et al. Non-invasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations. J Hepatol. 2010;52:579–85. http://www.ncbi.nlm.nih.gov/pubmed/20185194.
Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–50. http://www.ncbi.nlm.nih.gov/pubmed/12198701.
Raptis DA, Fischer MA, Graf R, Nanz D, Weber A, Moritz W, et al. MRI: the new reference standard in quantifying hepatic steatosis? Gut. 2012;61:117–27. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21997548.
Schwenzer NF, Springer F, Schraml C, Stefan N, Machann J, Schick F. Non-invasive assessment and quantification of liver steatosis by ultrasound, computed tomography and magnetic resonance. J Hepatol. 2009;51:433–45. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0168827809003900.
Fishbein MH, Stevens WR. Rapid MRI using a modified Dixon technique: a non-invasive and effective method for detection and monitoring of fatty metamorphosis of the liver. Pediatr Radiol. 200131:806–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11692239.
Lee SS, Park SH. Radiologic evaluation of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:7392. http://www.ncbi.nlm.nih.gov/pubmed/24966609.
Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Bekker Jeppesen P, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr. 2016;35:247–307. http://www.espen.org/files/ESPEN-Guidelines/1__ESPEN_guidelines_on_chronic_intestinal_failure_in_adults.pdf.
Pironi L, Goulet O, Buchman A, Messing B, Gabe S, Candusso M, et al. Outcome on home parenteral nutrition for benign intestinal failure: a review of the literature and benchmarking with the European prospective survey of ESPEN. Clin Nutr. 2012;31:831–45. http://www.ncbi.nlm.nih.gov/pubmed/22658443.
Lal S, Pironi L, Wanten G, Arends J, Bozzetti F, Cuerda C, et al. Clinical approach to the management of Intestinal Failure Associated Liver Disease (IFALD) in adults: a position paper from the Home Artificial Nutrition and Chronic Intestinal Failure Special Interest Group of ESPEN. Clin Nutr. 2018. http://www.ncbi.nlm.nih.gov/pubmed/30017241.
Abu-Wasel B, Molinari M. Liver disease secondary to intestinal failure. Biomed Res Int. 2014;2014:968357. http://www.ncbi.nlm.nih.gov/pubmed/24551858.
Sasdelli AS, Agostini F, Pazzeschi C, Guidetti M, Lal S, Pironi L. Assessment of intestinal failure associated liver disease according to different diagnostic criteria. Clin Nutr. 2018; https://www.sciencedirect.com/science/article/pii/S0261561418301705.
Dibb M, Teubner A, Theis V, Shaffer J, Lal S. Review article: the management of long-term parenteral nutrition. Aliment Pharm Ther. 2013;37:587–603. http://doi.wiley.com/10.1111/apt.12209.
Buchman AL, Iyer K, Fryer J. Parenteral nutrition-associated liver disease and the role for isolated intestine and intestine/liver transplantation. Hepatol. 2006;43:9–19. http://doi.wiley.com/10.1002/hep.20997.
Florence Lacaille GGVCLDCHIHSKJPRS. Intestinal Failure–associated liver disease: a position paper of the espghan working group of intestinal failure and intestinal transplantation. J Pediatr Gastroenterol Nutr. 2015;60:272–83. https://insights.ovid.com/crossref?an=00005176-201502000-00026.
Kelly DA. Intestinal failure–associated liver disease: what do we know today? Gastroenterology. 2006;130:S70–7. http://www.ncbi.nlm.nih.gov/pubmed/16473076.
Pironi L, Joly F, Forbes A, Colomb V, Lyszkowska M, Baxter J, et al. Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. 2011;60:17–25. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21068130.
Couinaud C. Le foie: etudes anatomiques et chirurgicales. Paris: Mason 1957: 400–9 Goldsmith NA, Woodburne RT. The surgical anatomy pertaining to liver resection. Surg Gynecol Obs. 1957;105:310–18.
Ma X, Holalkere N-S, R AK, Mino-Kenudson M, Hahn PF, Sahani D V. Imaging-based quantification of hepatic fat: methods and clinical applications. RadioGraphics. 2009;29:1253–77. http://www.ncbi.nlm.nih.gov/pubmed/19755595.
Tang A, Desai A, Hamilton G, Wolfson T, Gamst A, Lam J, et al. Accuracy of MR Imaging–estimated proton density fat fraction for classification of dichotomized histologic steatosis grades in nonalcoholic fatty liver disease. Radiology. 2015;274:416–25. http://www.ncbi.nlm.nih.gov/pubmed/25247408.
Bohte AE, van Werven JR, Bipat S, Stoker J. The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: a meta-analysis. Eur Radiol. 2011;21:87–97. http://www.ncbi.nlm.nih.gov/pubmed/20680289.
Imajo K, Kessoku T, Honda Y, Tomeno W, Ogawa Y, Mawatari H, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016;150:626–.e7. http://www.ncbi.nlm.nih.gov/pubmed/26677985.
Lee DH. Imaging evaluation of non-alcoholic fatty liver disease: focused on quantification. Clin Mol Hepatol. 2017. http://www.ncbi.nlm.nih.gov/pubmed/28994271.
van Werven JR, Marsman HA, Nederveen AJ, Smits NJ, ten Kate FJ, van Gulik TM, et al. Assessment of hepatic steatosis in patients undergoing liver resection: comparison of US, CT, T1-weighted dual-echo MR imaging, and point-resolved 1 H MR spectroscopy. Radiology. 2010;256:159–68. http://www.ncbi.nlm.nih.gov/pubmed/20574093.
Buchman A, Naini B, Spilker B. The differentiation of intestinal-failure-associated liver disease from nonalcoholic fatty liver and nonalcoholic steatohepatitis. Semin Liver Dis. 2017;37:033–44. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0036-1597771.
Kudsk KA, Munoz-Del-Rio A, Busch RA, Kight CE, Schoeller DA. Stratification of fat-free mass index percentiles for body composition based on National Health and Nutrition Examination Survey III Bioelectric Impedance Data. JPEN J Parenter Enteral Nutr. 2017;41:249–57. http://www.ncbi.nlm.nih.gov/pubmed/26092851.
Dulloo AG, Jacquet J, Solinas G, Montani J-P, Schutz Y. Body composition phenotypes in pathways to obesity and the metabolic syndrome. Int J Obes. 2010;34(S2):S4–17. http://www.nature.com/articles/ijo2010234.
Cavicchi M, Beau P, Crenn P, Degott C, Messing B. Prevalence of liver disease and contributing factors in patients receiving home parenteral nutrition for permanent intestinal failure. Ann Intern Med 2000;132:525–32. http://www.ncbi.nlm.nih.gov/pubmed/10744588.
Acknowledgements
This study would not be possible without the help from our nursing staff. Special thanks goes to Laura Petrica and Nizra Palamar.
Author information
Authors and Affiliations
Contributions
TJ, PP and NRK. TJ contributed to the data collection, analyzed the data and drafted the manuscript. PP contributed to conception of the study, data interpretation and reviewed/edited the paper. NRK was responsible for the concept/ design of the study, and contributed to the data analysis and interpretation, and revised the paper. All authors read and approved the final paper and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jordan, T., Popovič, P. & Rotovnik Kozjek, N. Liver steatosis in adult patients on home parenteral nutrition. Eur J Clin Nutr 74, 255–260 (2020). https://doi.org/10.1038/s41430-019-0455-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0455-4
This article is cited by
-
NAFLD, MAFLD, and beyond: one or several acronyms for better comprehension and patient care
Internal and Emergency Medicine (2023)