Abstract
Background
Discrepancy between prescribed and administered enteral nutrition (EN) is a common problem during intensive care. The aim of this study was to find out the success rate and factors associated with inadequacy of enteral nutrition in a mixed general intensive care unit (ICU).
Methods
This was a retrospective single-center study of 892 patients with ICU length of stay (LOS) ≥4 days. The factors associated with adequacy of enteral nutrition on day 4 were analyzed. These included disease-specific factors, patient-related factors, severity of illness, and procedural factors.
Results
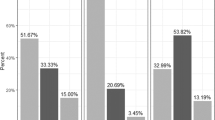
Of the 892 patients, 349 (39.1%) had an EN success rate of ≥70%, which was associated with a lower amount of prescribed enteral energy (500 kcal [500–800] vs. 800 kcal [500–1200], p < 0.001) and bolus administration of enteral nutrition (41 of 349 vs. 27 of 543, p < 0.001). Other factors impairing successful EN were severe inflammation, surgery, and GI-related admission diagnosis.
Conclusions
On the fourth day during ICU stay discrepancy between prescribed and administered enteral nutrition was associated to severe inflammation, GI-related diagnosis, and prescribing policy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Taylor BE, McClave SA, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016;44:390–438.
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP. et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr.2019;38:48–79.
Elke G, van Zanten AR, Lemieux M, McCall M, Jeejeebhoy KN, Kott M, et al. Enteral versus parenteral nutrition in critically ill patients: an updated systematic review and meta-analysis of randomized controlled trials. Crit Care. 2016;20:117. 016-1298-1.
Cahill NE, Dhaliwal R, Day AG, Jiang X, Heyland DK. Nutrition therapy in the critical care setting: what is “best achievable” practice? An international multicenter observational study. Crit Care Med. 2010;38:395–401.
Adam S, Batson S. A study of problems associated with the delivery of enteral feed in critically ill patients in five ICUs in the UK. Intensive Care Med. 1997;23:261–6.
Uozumi M, Sanui M, Komuro T, Iizuka Y, Kamio T, Koyama H, et al. Interruption of enteral nutrition in the intensive care unit: a single-center survey. J Intensive Care. 2017;5:52. 017-0245-9. eCollection 2017.
Passier RH, Davies AR, Ridley E, McClure J, Murphy D, Scheinkestel CD. Periprocedural cessation of nutrition in the intensive care unit: opportunities for improvement. Intensive Care Med. 2013;39:1221–6.
Ichimaru S. Methods of enteral nutrition administration in critically ill patients: continuous, cyclic, intermittent, and bolus feeding. Nutr Clin Pract. 2018;33:790–5.
Patel JJ, Rosenthal MD, Heyland DK. Intermittent versus continuous feeding in critically ill adults. Curr Opin Clin Nutr Metab Care. 2018;21:116–20.
Chowdhury AH, Murray K, Hoad CL, Costigan C, Marciani L, Macdonald IA, et al. Effects of bolus and continuous nasogastric feeding on gastric emptying, small bowel water content, superior mesenteric artery blood flow, and plasma hormone concentrations in healthy adults: a randomized crossover study. Ann Surg. 2016;263:450–7.
Jose IB, Leandro-Merhi VA, Aquino JLB. Target, prescription and infusion of enteral nutritional therapy of critical patients in intensive care unit. Arq Gastroenterol. 2018;55:283–9.
Gonzalez-Granda A, Schollenberger A, Haap M, Riessen R, Bischoff SC. Optimization of nutrition therapy with the use of calorimetry to determine and control energy needs in mechanically ventilated critically ill patients: the ONCA study, a randomized, prospective pilot study. J Parenter Enteral Nutr. 2019;43:481–9.
Kim SH, Park CM, Seo JM, Choi M, Lee DS, Chang DK, et al. The impact of implementation of an enteral feeding protocol on the improvement of enteral nutrition in critically ill adults. Asia Pac J Clin Nutr. 2017;26:27–35.
Capuzzo M, Volta C, Tassinati T, Moreno R, Valentin A, Guidet B, et al. Hospital mortality of adults admitted to Intensive Care Units in hospitals with and without Intermediate Care Units: a multicentre European cohort study. Crit Care. 2014;18:551. 014-0551-8.
Reignier J, Boisrame-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, et al. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet. 2018;391:133–43.
Hietanen S, Ala-Kokko T, Ohtonen P, Kakela R, Niemela S, Liisanantti JH. Treatment profile and 1-year mortality among nontraumatic intensive care unit patients with alcohol-related health problems. J Intensive Care Med. 2017:885066617740071[in press].
Author contributions
JN was responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analyzing the data, interpreting the results and updating the reference lists. TK was responsible for analyzing the data and contributed to writing the report. MV and TA provided feedback on the report. JHL was responsible for designing the review protocol and screening potentially eligible studies. He contributed to writing the report, extracting and analyzing the data, and interpreting the results.
Funding
The study was funded by grants from Oulu University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nurkkala, J., Kaakinen, T., Vakkala, M. et al. Factors associated with discrepancy between prescribed and administered enteral nutrition in general ICU. Eur J Clin Nutr 74, 248–254 (2020). https://doi.org/10.1038/s41430-019-0451-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0451-8
This article is cited by
-
Nutrition delivery after emergency laparotomy in surgical ward: a retrospective cohort study
European Journal of Trauma and Emergency Surgery (2022)
-
Causes of nutrition deficit during immediate postoperative period after free flap surgery for cancer of the head and neck
European Archives of Oto-Rhino-Laryngology (2021)