Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is a major global health problem. The most common cause of death in these patients is due to cardiovascular disorders. The aim of this study was to examine the effects of curcumin supplementation on cardiovascular risk factors in patients with NAFLD.
Methods and materials
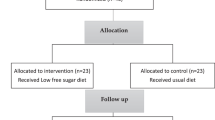
In this randomized, placebo-controlled, clinical trial, fifty two patients with NAFLD were randomly assigned to receive life style recommendations plus either 1500 mg curcumin or placebo for 12 weeks. Anthropometric indices, blood lipid profile, insulin resistance, as well as hepatic steatosis and fibrosis scores were measured at the beginning and the end of the study, and compared between and within groups.
Results
Hepatic fibrosis, serum cholesterol, glucose and alanin aminotransferase (ALT) reduced significantly only in curcumin group (p < 0.05). Anthropometric indices, blood lipid profile, insulin resistance, and hepatic steatosis decreased significantly in both groups (p < 0.05), without any significant difference between two groups.
Conclusion
Our results showed that daily intake of 1500 mg curcumin plus weight loss is not superior to weight loss alone in amelioration of cardiovascular risk factors in patients with NAFLD. Further studies with different dosages of curcumin are needed to be able to conclude about the effects of this dietary supplement on cardiovascular risk factors and NAFLD characteristics.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Faghihzadeh F, Adibi P, Rafiei R, Hekmatdoost A. Resveratrol supplementation improves inflammatory biomarkers in patients with nonalcoholic fatty liver disease. Nutr Res. 2014;34:837–43.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62:S47–S64.
Khoshbaten M, Hekmatdoost A, Ghasemi H, Entezariasl M. Prevalence of gastrointestinal symptoms and signs in northwestern Tabriz, Iran. Indian J Gastroenterol. 2004;23:168–70.
Yilmaz Y. is non‐alcoholic fatty liver disease a spectrum, or are steatosis and non‐alcoholic steatohepatitis distinct conditions? Aliment Pharmacol Ther. 2012;36:815–23.
Maithilikarpagaselvi N, Sridhar MG, Swaminathan RP, Sripradha R, Badhe B. Curcumin inhibits hyperlipidemia and hepatic fat accumulation in high-fructose-fed male Wistar rats. Pharm Biol. 2016;54:2857–63.
Morisco F, Vitaglione P, Amoruso D, Russo B, Fogliano V, Caporaso N. Foods and liver health. Mol Asp Med. 2008;29:144–50.
Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65:1038–48.
Eslamparast T, Poustchi H, Zamani F, Sharafkhah M, Malekzadeh R, Hekmatdoost A. Synbiotic supplementation in nonalcoholic fatty liver disease: a randomized, double-blind, placebo-controlled pilot study–. Am J Clin Nutr. 2014;99:535–42.
Askari F, Rashidkhani B, Hekmatdoost A. Cinnamon may have therapeutic benefits on lipid profile, liver enzymes, insulin resistance, and high-sensitivity C-reactive protein in nonalcoholic fatty liver disease patients. Nutr Res. 2014;34:143–8.
Faghihzadeh F, Adibi P, Hekmatdoost A. The effects of resveratrol supplementation on cardiovascular risk factors in patients with non-alcoholic fatty liver disease: a randomised, double-blind, placebo-controlled study. Br J Nutr. 2015;114:796–803.
Yari Z, Rahimlou M, Eslamparast T, Ebrahimi-Daryani N, Poustchi H, Hekmatdoost A. Flaxseed supplementation in non-alcoholic fatty liver disease: a pilot randomized, open labeled, controlled study. Int J Food Sci Nutr. 2016;67:461–9.
Curcumin BengmarkS. An atoxic antioxidant and natural NFκB, cyclooxygenase‐2, lipooxygenase, and inducible nitric oxide synthase inhibitor: a shield against acute and chronic diseases. J Parenter Enter Nutr. 2006;30:45–51.
Nabavi SF, Daglia M, Moghaddam AH, Habtemariam S, Nabavi SM. Curcumin and liver disease: from chemistry to medicine. Compr Rev Food Sci Food Saf. 2014;13:62–77.
Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: the Indian solid gold. Adv Exp Med Biol. 2007;595:1–75.
Rivera-Espinoza Y, Muriel P. Pharmacological actions of curcumin in liver diseases or damage. Liver Int: Off J Int Assoc Study Liver. 2009;29:1457–66.
Dattani J, Rajput D, Moid N, Highland H, George L, Desai K. Ameliorative effect of curcumin on hepatotoxicity induced by chloroquine phosphate. Environ Toxicol Pharmacol. 2010;30:103–9.
Alm-Eldeen AA, Mona MH, Shati AA, El-Mekkawy HI. Synergistic effect of black tea and curcumin in improving the hepatotoxicity induced by aflatoxin B1 in rats. Toxicol Ind Health. 2015;31:1269–80.
Coban D, Milenkovic D, Chanet A, Khallou‐Laschet J, Sabbe L, Palagani A, et al. Dietary curcumin inhibits atherosclerosis by affecting the expression of genes involved in leukocyte adhesion and transendothelial migration. Mol Nutr Food Res. 2012;56:1270–81.
Jang E-M, Choi M-S, Jung UJ, Kim M-J, Kim H-J, Jeon S-M, et al. Beneficial effects of curcumin on hyperlipidemia and insulin resistance in high-fat–fed hamsters. Metab-Clin Exp. 2008;57:1576–83.
Tang Y, Zheng S, Chen A. Curcumin eliminates leptin’s effects on hepatic stellate cell activation via interrupting leptin signaling. Endocrinology. 2009;150:3011–20.
Tang Y. Curcumin targets multiple pathways to halt hepatic stellate cell activation: updated mechanisms in vitro and in vivo. Dig Dis Sci. 2015;60:1554–64.
Rivera‐Espinoza Y, Muriel P. Pharmacological actions of curcumin in liver diseases or damage. Liver Int. 2009;29:1457–66.
Vizzutti F, Provenzano A, Galastri S, Milani S, Delogu W, Novo E, et al. Curcumin limits the fibrogenic evolution of experimental steatohepatitis. Lab Invest. 2010;90:104.
Ramirez-Tortosa MC, Ramirez-Tortosa CL, Mesa MD, Granados S, Gil Á, Quiles JL. Curcumin ameliorates rabbits’s steatohepatitis via respiratory chain, oxidative stress, and TNF-α. Free Radic Biol Med. 2009;47:924–31.
Panahi Y, Kianpour P, Mohtashami R, Jafari R, Simental-Mendía LE, Sahebkar A. Curcumin lowers serum lipids and uric acid in subjects with nonalcoholic fatty liver disease: a randomized controlled trial. J Cardiovasc Pharmacol. 2016;68:223–9.
Rahmani S, Asgary S, Askari G, Keshvari M, Hatamipour M, Feizi A, et al. Treatment of Non‐alcoholic Fatty Liver Disease with Curcumin: A Randomized Placebo‐controlled Trial. Phytother Res. 2016;30:1540–8.
Panahi Y, Kianpour P, Mohtashami R, Jafari R, Simental-Mendía LE, Sahebkar A. Efficacy and safety of phytosomal curcumin in non-alcoholic fatty liver disease: a randomized controlled trial. Drug Res (Stuttg). 2017;67:244–51.
National Heart, Lung, and Blood Institute. The Practical Guide: identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: National Institutes of Health, National Heart, Lung, and Blood Institute, NHLBI Obesity Education Initiative, North American Association for the Study of Obesity, 2000. https://www.nhlbi.nih.gov/files/docs/guidelines/prctgd_c.pdf
Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007;85:19–26.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Vanhala P, Vanhala M, Kumpusalo E, Keinanen-Kiukaanniemi S. The quantitative insulin sensitivity check index QUICKI predicts the onset of type 2 diabetes better than fasting plasma insulin in obese subjects: a 5-year follow-up study. J Clin Endocrinol Metab. 2002;87:5834–7.
Li B, Wang L, Lu Q, Da W. Liver injury attenuation by curcumin in a rat NASH model: an Nrf2 activation-mediated effect? Ir J Med Sci (1971). 2016;185:93–100.
Zhao NJ, Liao MJ, Wu JJ, Chu KX. Curcumin suppresses Notch1 signaling: Improvements in fatty liver and insulin resistance in rats. Mol Med Rep. 2018;17:819–26.
Ghaemi A, Taleban FA, Hekmatdoost A, Rafiei A, Hosseini V, Amiri Z, et al. How much weight loss is effective on nonalcoholic fatty liver disease? Hepatitis Mon. 2013;13:e15227.
Vizzutti F, Arena U, Marra F, Pinzani M. Elastography for the non-invasive assessment of liver disease: limitations and future developments. Gut. 2009;58:157–60.
Yilmaz Y, Yesil A, Gerin F, Ergelen R, Akin H, Celikel ÇA, et al. Detection of hepatic steatosis using the controlled attenuation parameter: a comparative study with liver biopsy. Scand J Gastroenterol. 2014;49:611–6.
Schiborr C, Kocher A, Behnam D, Jandasek J, Toelstede S, Frank J. The oral bioavailability of curcumin from micronized powder and liquid micelles is significantly increased in healthy humans and differs between sexes. Mol Nutr Food Res. 2014;58:516–27.
Acknowledgements
We would like to thank all participants without whom this study was impossible. The study was financially supported by a grant from Shahid Beheshti University of Medical Sciences to AH.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saadati, S., Hatami, B., Yari, Z. et al. The effects of curcumin supplementation on liver enzymes, lipid profile, glucose homeostasis, and hepatic steatosis and fibrosis in patients with non-alcoholic fatty liver disease. Eur J Clin Nutr 73, 441–449 (2019). https://doi.org/10.1038/s41430-018-0382-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0382-9
This article is cited by
-
Prepuberty is a window period for curcumin to prevent obesity in postnatal overfed rats
Pediatric Research (2024)
-
Natural compounds proposed for the management of non-alcoholic fatty liver disease
Natural Products and Bioprospecting (2024)
-
An updated meta-analysis of effects of curcumin on metabolic dysfunction-associated fatty liver disease based on available evidence from Iran and Thailand
Scientific Reports (2023)
-
Targeting HSP47 and HSP70: promising therapeutic approaches in liver fibrosis management
Journal of Translational Medicine (2022)