ABSTRACT
Background
Carnitine deficiency is common in patients on hemodialysis. However, the efficacy of L-carnitine supplementation for improving lean body mass (LBM) and physical function has not yet been evaluated.
Methods
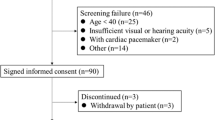
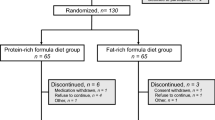
In this multicenter, prospective, parallel, randomized, controlled trial, 91 patients on hemodialysis who developed carnitine deficiency were randomly assigned to receive injections of 1,000 mg L-carnitine 3 times per week after each hemodialysis session (L-carnitine group) or no injections (control group) with monitoring for 12 months.
Results
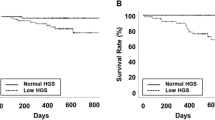
The data for 84 of the 91 patients were available for analysis (L-carnitine group, n = 42; control group, n = 42). Dry weight and body mass index did not significantly change in the l-carnitine group, but significantly decreased in the control group. Arm muscle area (AMA) did not change significantly in the L-carnitine group but decreased significantly in the control group; the difference in mean AMA between the groups was 6.22% (95% confidence interval [CI] 1.90–10.5; P = 0.037). Hand grip strength did not change significantly in the L-carnitine group, but decreased significantly in the control group. The difference in change in hand grip strength between the groups was 4.27% (95% CI 0.42–8.12; P = 0.030). Furthermore, LBM did not change significantly in the l-carnitine group but decreased significantly in the control group; the difference in mean LBM between the groups was 2.92 % (95% CI 1.28–4.61; P = 0.0007).
Conclusions
l-carnitine supplementation is useful in patients who develop carnitine deficiency on hemodialysis because it maintains physical function and LBM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Evans AM, Faull RJ, Nation RL, Prasad S, Elias T, Reuter SE, et al. Impact of hemodialysis on endogenous plasma and muscle carnitine levels in patients with end-stage renal disease. Kidney Int. 2004;66:1527–34.
Higuchi T, Abe M, Yamazaki T, Okawa E, Ando H, Hotta S, et al. Levocarnitine improves cardiac function in hemodialysis patients with left ventricular hypertrophy: a randomized controlled trial. Am J Kidney Dis. 2016;67:260–70.
Schreiber B. Levocarnitine and dialysis: a review. Nutr Clin Pract. 2005;20:218–43.
Matera M, Bellinghieri G, Costantino G, Santoro D, Calvani M, Savica V. History of L-carnitine: implications for renal disease. J Ren Nutr. 2003;13:2–14.
Cruz-Jentoft AJ, Landi F, Topinková E, Michel JP. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010;13:1–7.
Muscaritoli M, Anker SD, Argilés J, Aversa Z, Bauer JM, Biolo G, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010;29:154–9.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc. 2011;12:249–56.
Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K, et al. International Society of Renal Nutrition and Metabolism. Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84:1096–107.
Kim JC, Kalantar-Zadeh K, Kopple JD. Frailty and protein-energy wasting in elderly patients with end stage kidney disease. J Am Soc Nephrol. 2013;24:337–51.
Carrero JJ, Stenvinkel P, Cuppari L, Ikizler TA, Kalantar-Zadeh K, Kaysen G, et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J Ren Nutr. 2013;23:77–90.
Johansen KL, Chertow GM, Ng AV, Mulligan K, Carey S, Schoenfeld PY, et al. Physical activity levels in patients on hemodialysis and healthy sedentary controls. Kidney Int. 2000;57:2564–70.
Stack AG, Martin DR. Association of patient autonomy with increased transplantation and survival among new dialysis patients in the United States. Am J Kidney Dis. 2005;45:730–42.
Bishop CW. Reference values for arm muscle area, arm fat area, subscapular skinfold thickness, and sum of skinfold thicknesses for American adults. J Parenter Enter Nutr. 1984;8:515–22.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Badrasawi M, Shahar S, Zahara AM, Nor Fadilah R, Singh DK. Efficacy of L-carnitine supplementation on frailty status and its biomarkers, nutritional status, and physical and cognitive function among prefrail older adults: a double-blind, randomized, placebo-controlled clinical trial. Clin Interv Aging. 2016;11:1675–86.
Evans M, Guthrie N, Pezzullo J, Sanli T, Fielding RA, Bellamine A. Efficacy of a novel formulation of L-Carnitine, creatine, and leucine on lean body mass and functional muscle strength in healthy older adults: a randomized, double-blind placebo-controlled study. Nutr Metab (Lond). 2017;14:7.
Malaguarnera M, Cammalleri L, Gargante MP, Vacante M, Colonna V, Motta M. L-Carnitine treatment reduces severity of physical and mental fatigue and increases cognitive functions in centenarians: a randomized and controlled clinical trial. Am J Clin Nutr. 2007;86:1738–44.
Malaguarnera M, Gargante MP, Cristaldi E, Colonna V, Messano M, Koverech A, et al. Acetyl L-carnitine (ALC) treatment in elderly patients with fatigue. Arch Gerontol Geriatr. 2008;46:181–90.
Hoppel C. The role of carnitine in normal and altered fatty acid metabolism. Am J Kidney Dis. 2003;41(Suppl 4):S4–12.
Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2001;38:1251–63.
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73:391–8.
Abe M, Kalantar-Zadeh K. Haemodialysis-induced hypoglycaemia and glycaemic disarrays. Nat Rev Nephrol. 2015;11:302–13.
Johansen KL. The frail dialysis population: a growing burden for the dialysis community. Blood Purif. 2015;40:288–92.
Johansen KL, Chertow GM, Jin C, Kutner NG. Significance of frailty among dialysis patients. J Am Soc Nephrol. 2007;18:2960–7.
Bellinghieri G, Santoro D, Calvani M, Savica V. Role of carnitine in modulating acute-phase protein synthesis in hemodialysis patients. J Ren Nutr. 2005;15:13–7.
Kopple JD, Zhu X, Lew NL, Lowrie EG. Body weight-for-height relationships predict mortality in maintenance hemodialysis patients. Kidney Int. 1999;56:1136–48.
Stenvinkel P, Heimbürger O, Lindholm B, Kaysen GA, Bergström J. Are there two types of malnutrition in chronic renal failure? Evidence for relationship between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. 2000;15:953–60.
Kalantar-Zadeh K, Block G, McAllister CJ, Humphreys MH, Kopple JD. Appetite and inflammation, nutrition, anemia, and clinical outcome in hemodialysis patients. Am J Clin Nutr. 2004;80:299–307.
Bistrian BR, Schwartz J, Istfan NW. Cytokines, muscle proteolysis, and the catabolic response to infection and inflammation. Proc Soc Exp Biol Med. 1992;200:220–3.
Duranay M, Akay H, Yilmaz FM, Senes M, Tekeli N, Yücel D. Effects of L-carnitine infusions on inflammatory and nutritional markers in haemodialysis patients. Nephrol Dial Transplant. 2006;21:3211–4.
Suchitra MM, Ashalatha VL, Sailaja E, Rao AM, Reddy VS, Bitla AR, et al. The effect of L-carnitine supplementation on lipid parameters, inflammatory and nutritional markers in maintenance hemodialysis patients. Saudi J Kidney Dis Transpl. 2011;22:1155–9.
Shakeri A, Tabibi H, Hedayati M. Effects of L-carnitine supplement on serum inflammatory cytokines, C-reactive protein, lipoprotein (a), and oxidative stress in hemodialysis patients with Lp (a) hyperlipoproteinemia. Hemodial Int. 2010;14:498–504.
Siew ED, Ikizler TA. Insulin resistance and protein energy metabolism in patients with advanced chronic kidney disease. Semin Dial. 2010;23:378–82.
Eidemak I, Feldt-Rasmussen B, Kanstrup IL, Nielsen SL, Schmitz O, Strandgaard S. Insulin resistance and hyperinsulinemia in mild to moderate progressive chronic renal failure and its association with aerobic work capacity. Diabetologia. 1995;38:565–72.
Mak RHK. Correction of anemia by erythropoietin reverses insulin resistance and hyperinsulinemia in uremia. Am J Physiol. 1996;270:F839–94.
Abe M, Okada K, Soma M, Matsumoto K. Relationship between insulin resistance and erythropoietin responsiveness in hemodialysis patients. Clin Nephrol. 2011;75:49–58.
Rasmussen BB, Holmbäck UC, Volpi E, Morio-Liondore B, Paddon-Jones D, Wolfe RR. Malonyl coenzyme A and the regulation of functional carnitine palmitoyltransferase-1 activity and fat oxidation in human skeletal muscle. J Clin Invest. 2002;110:1687–93.
Günal AI, Celiker H, Dönder E, Günal SY. The effect of L-carnitine on insulin resistance in hemodialysed patients with chronic renal failure. J Nephrol. 1999;12:38–40.
Savica V, Calvani M, Benatti P, Santoro D, Monardo P, Peluso G, et al. Carnitine system in uremic patients: molecular and clinical aspects. Semin Nephrol. 2004;24:464–8.
Schreiber B. Levocarnitine and dialysis: a review. Nutr Clin Pract. 2005;20:218–43.
Ferrannini E, Buzzigoli G, Bevilacqua S, Boni C, Del Chiaro D, Oleggini M, et al. Interaction of carnitine with insulin-stimulated glucose metabolism in humans. Am J Physiol. 1988;255:E946–952.
Capaldo B, Napoli R, Di Bonito P, Albano G, Saccà L. Carnitine improves peripheral glucose disposal in non-insulin-dependent diabetic patients. Diabetes Res Clin Pract. 1991;14:191–5.
Author contributions
Research concept and study design: TH, TM, NM. Acquisition of data: CN, HT, MK, KU, RT, TF, TY, EO. Data analysis and interpretation: TM, NM. Statistical analysis: TH, MA. Supervision or mentorship: HA, FK. Each author contributed significant intellectual content during drafting or revision of the manuscript and takes accountability for the overall work by ensuring appropriate investigation and resolution of questions pertaining to the accuracy or integrity of any aspect of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MA has received honoraria from Otsuka Pharmaceutical Co., Ltd. The other authors declare that they have no conflict of interest.
Additional information
These authors contributed equally: Takashi Maruyama, Noriaki Maruyama
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Maruyama, T., Maruyama, N., Higuchi, T. et al. Efficacy of L-carnitine supplementation for improving lean body mass and physical function in patients on hemodialysis: a randomized controlled trial. Eur J Clin Nutr 73, 293–301 (2019). https://doi.org/10.1038/s41430-018-0348-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0348-y
This article is cited by
-
Was ist L-Carnitin, und sollten wir es bei CKD supplementieren?
Die Nephrologie (2024)
-
Mitigating the pro-oxidant state and melanogenesis of Retinitis pigmentosa: by counteracting mitochondrial dysfunction
Cellular and Molecular Life Sciences (2021)