Abstract
Background:
Studies associate sleeping and eating late in the day with poor dietary quality and higher obesity risk but differences in sleep duration confound this association. We aimed to determine whether sleep and meal timing, independent of sleep duration, influenced food intake in healthy adults.
Methods:
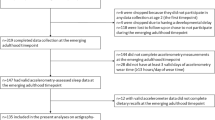
This was a controlled, 2 × 2 inpatient crossover study with normal (0000-0800 h) or late (0330-1130 h) sleep and normal (1, 5, 11, and 12.5 h after awakening) or late (4.5, 8.5, 14.5, and 16 h after awakening) meals. Food intake was controlled while blood samples were obtained for determination of appetite-regulating hormones on days 3-4. Self-selected food intake was assessed on day 5. Data were analyzed using linear mixed model analysis with sleep, meal, and sleep x meal interaction as dependent variables.
Results:
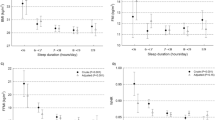
Five participants completed all phases (mean age 25.1 ± [SD] 3.9 y, body mass index 29.2 ± 2.7 kg/m2). There was a significant sleep x meal interaction on energy intake (P = 0.035) and trends on fat and sodium intakes (P < 0.10). Overnight ghrelin concentrations were higher under normal sleep and meal conditions relative to late (P < 0.005) but lower when both were combined (P < 0.001). Overnight leptin concentrations were higher under normal meal conditions (P = 0.012). There was a significant sleep x meal interaction on ghrelin (P = 0.032) and glucagon-like peptide 1 (P = 0.041) concentrations, but not leptin (P = 0.83), in response to a test meal.
Conclusions:
Our results suggest that alignment of sleep and meals may influence food choice and energy balance. Additional research is necessary to expand and confirm our findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Di Lorenzo L, De Pergola G, Zocchetti C, L’Abbate N, Basso A, Pannacciulli N, et al. Effect of shift work on body mass index: results of a study performed in 319 glucose-tolerant men working in a Southern Italian industry. Int J Obes Relat Metab Disord. 2003;27:1353–8. https://doi.org/10.1038/sj.ijo.0802419
van Drongelen A, Boot CR, Merkus SL, Smid T, van der Beek AJ. The effects of shift work on body weight change - a systematic review of longitudinal studies. Scandinavian journal of work, environment & health. 2011;37:263–75. https://doi.org/10.5271/sjweh.3143
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43. https://doi.org/10.1016/j.cub.2012.03.038
Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). 2011;19:1374–81. e-pub ahead of print 2011/04/30; doi: oby2011100 [pii] 10.1038/oby.2011.100
St-Onge M-P, Roberts A, Chen J, Kelleman M, O’Keeffe M, Jones P. Short sleep duration increases energy intakes but does not change expenditure in normal weight individuals. The American journal of clinical nutrition. 2011;94:410–6. e-pub ahead of print2011 Jun29.
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. The American journal of clinical nutrition. 2009;89:126–33.
Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake and meal timing in healthy adults. Sleep. 2013;36:981–90.
Markwald RR, Melanson EL, Smith MR, Higgins J, Perreault L, Eckel RH, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:5695–5700. https://doi.org/10.1073/pnas.1216951110
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring). 2009;17:2100–2. e-pub ahead of print 2009/09/05; doi: oby2009264 [pii]10.1038/oby.2009.264
Bray MS, Ratcliffe WF, Grenett MH, Brewer RA, Gamble KL, Young ME. Quantitative analysis of light-phase restricted feeding reveals metabolic dyssynchrony in mice. International journal of obesity. 2012. https://doi.org/10.1038/ijo.2012.137. e-pub ahead of print 2012/08/22
Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, Haim A, et al. Light at night increases body mass by shifting the time of food intake. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:18664–9. e-pub ahead of print 2010/10/13; doi: 1008734107 [pii] 10.1073/pnas.1008734107
Cain SW, Filtness AJ, Phillips CL, Anderson C. Enhanced preference for high-fat foods following a simulated night shift. Scandinavian journal of work, environment & health. 2015;41:288–93. https://doi.org/10.5271/sjweh.3486
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. The American journal of clinical nutrition. 1990;51:241–7. e-pub ahead of print1990/02/01
Kissileff HR, Wentzlaff TH, Guss JL, Walsh BT, Devlin MJ, Thornton JC. A direct measure of satiety disturbance in patients with bulimia nervosa. Physiology & behavior. 1996;60:1077–85. e-pub ahead of print1996/10/01
Dzaja A, Dalal MA, Himmerich H, Uhr M, Pollmacher T, Schuld A. Sleep enhances nocturnal plasma ghrelin levels in healthy subjects. American journal of physiology. Endocrinology and metabolism. 2004;286:E963–967. https://doi.org/10.1152/ajpendo.00527.2003
Natalucci G, Riedl S, Gleiss A, Zidek T, Frisch H. Spontaneous 24-h ghrelin secretion pattern in fasting subjects: maintenance of a meal-related pattern. Eur J Endocrinol. 2005;152:845–50. https://doi.org/10.1530/eje.1.01919
Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:4453–8. e-pub ahead of print 2009/03/04; 0808180106 [pii] 10.1073/pnas.0808180106
Thomas EA, Higgins J, Bessesen DH, McNair B, Cornier MA. Usual breakfast eating habits affect response to breakfast skipping in overweight women. Obesity (Silver Spring). 2015;23:750–9. https://doi.org/10.1002/oby.21049
St-Onge MP, O’Keeffe M, Roberts AL, RoyChoudhury A, Laferrere B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35:1503–10. https://doi.org/10.5665/sleep.2198. e-pub ahead of print 2012/11/02
Reid KJ, Baron KG, Zee PC. Meal timing influences daily caloric intake in healthy adults. Nutr Res. 2014;34:930–5. https://doi.org/10.1016/j.nutres.2014.09.010
Author Contributions
MPSO designed the study, analyzed and interpreted data, and wrote the manuscript. She takes full responsibility for the data contained in this report. TP and KK conducted the study, analyzed data, and contributed to writing the manuscript. BL provided medical supervision for the study, assisted with data interpretation and manuscript preparation. AR performed statistical analysis of the data and assisted with data interpretation and manuscript preparation.
Funding
This study was funded by the National Institutes of Health grants R56HL0119945 (MPSO) and DK26687, and also in part by Columbia University’s CTSA grant UL1 TR000040 from NCATS/NIH. This article is published as part of a supplement sponsored by the Mediterranean Diet Foundation and the Diputació de Barcelona.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M-PS-O received grant support from the National Institutes of Health. ARC owns stock in Alphabet Inc and received grant support National Institutes of Health and National Science Foundation.
Rights and permissions
About this article
Cite this article
St-Onge, MP., Pizinger, T., Kovtun, K. et al. Sleep and meal timing influence food intake and its hormonal regulation in healthy adults with overweight/obesity. Eur J Clin Nutr 72 (Suppl 1), 76–82 (2019). https://doi.org/10.1038/s41430-018-0312-x
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0312-x
This article is cited by
-
The Impact of Meal Timing on Risk of Weight Gain and Development of Obesity: a Review of the Current Evidence and Opportunities for Dietary Intervention
Current Diabetes Reports (2022)
-
Integration of Time-Based Recommendations with Current Pediatric Health Behavior Guidelines: Implications for Obesity Prevention and Treatment in Youth
Current Obesity Reports (2022)
-
Culturally-consistent diet among individuals of Mexican descent at the US-Mexico border is associated with sleep duration and snoring
BMC Nutrition (2021)
-
The Challenge of Maintaining Metabolic Health During a Global Pandemic
Sports Medicine (2020)