Abstract
Background/Objectives
The aim of the present study was to investigate the relationship between tea drinking and gallstones, specifically to evaluate the amount and time of tea consumption by gender.
Subjects/Methods
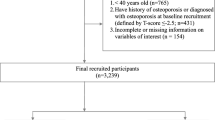
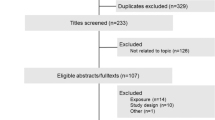
A total of 14,555 eligible adults receiving health examinations were included. The participants were divided into three subgroups with tea consumption of none, <240/day and ≥240 ml/day. We defined 120 ml for each traditional Chinese teapot as a “cup,” and the variable “cup-year” was obtained by multiplying the cups per day by the years of tea consumption. Based on the findings of abdominal ultrasound examination, gallstones was defined by the presence of movable or gravity-dependent intraluminal hyperechoic foci that attenuated ultrasound transmission.
Results
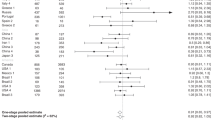
Among the participants, 1040 (7.1%) had gallstones. In multivariate analysis, the inverse relationship between tea drinking habit and gallstones was significant (OR = 0.807; 95% CI = 0.685−0.951, p = 0.010). Daily consumption of 1−240 ml (OR = 0.741; 95% CI = 0.584−0.941, p = 0.014), but not ≥240 ml, was associated with reduced risk of gallstones. In addition, the 1−19 cup-year group had significantly lower associated risk of gallstones (OR = 0.677; 95% CI = 0.534−0.857, p = 0.001), while the ≥19 cup-year group did not. By gender, subjects with tea consumption of 1−19 cup-year exhibited a low associated risk of gallstones in both males (OR = 0.678; 95% CI = 0.504−0.913, p = 0.010) and females (OR = 0.671; 95% CI = 0.453−0.994, p = 0.047), while subjects with ≥19 cup-years did not.
Conclusions
Appropriate tea drinking if less than 240 ml/day or 19 cup-years was associated with a decreased risk of gallstones in both genders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gall bladder disease in the United States. Gastroenterology. 1999;117:632–9.
Chen CH, Huang MH, Yang JC, Nien CK, Etheredge GD,Yang CC, et al. Prevalence and risk factors of gallstone disease in an adult population of Taiwan: an epidemiological survey. J Gastroenterol Hepatol. 2006;21:1737–43. https://doi.org/10.1111/j.1440-1746.2006.04381.x.
Liu CM, Tung TH, Chou P, Chen VT, Hsu CT, Chien WS, et al. Clinical correlation of gallstone disease in a Chinese population in Taiwan: experience at Cheng Hsin General Hospital. World J Gastroenterol. 2006;12:1281–6.
Lai SW, Liao KF, Lai HC, Chou CY, Cheng KC, Lai YM. The prevalence of gall bladder stones is higher among patients with chronic kidney disease in Taiwan. Medicine (Baltimore). 2009;88:46–51. https://doi.org/10.1097/MD.0b013e318194183f.
Naeem M, Rahimnajjad NA, Rahimnajjad MK, Khurshid M, Ahmed QJ, Shahid SM, et al. Assessment of characteristics of patients with cholelithiasis from economically deprived rural Karachi, Pakistan. BMC Res Notes. 2012;5:334 https://doi.org/10.1186/1756-0500-5-334.
Lai SW, Ng KC. Risk factors for gallstone disease in a hospital-based study. South Med J. 2002;95:1419–23.
Misciagna G, Centonze S, Leoci C, Guerra V, Cisternino AM, Ceo R, et al. Diet, physical activity, and gallstones—a population-based, case-control study in southern Italy. Am J Clin Nutr. 1999;69:120–6.
Misciagna G, Leoci C, Guerra V, Chiloiro M, Elba S, Petruzzi J, et al. Epidemiology of cholelithiasis in southern Italy. Part II: risk factors. Eur J Gastroenterol Hepatol. 1996;8:585–93.
Ishizuk H, Eguchi H, Oda T, Ogawa S, Nakagawa K, Honjo S, et al. Relation of coffee, green tea, and caffeine intake to gallstone disease in middle-aged Japanese men. Eur J Epidemiol. 2003;18:401–5.
Chandran AP, Sivarajan RR, Srinivas M, Srinivasan V, Venkataraman J. Risk factors for choledocholithiasis in a south Indian population: a case-control study. Indian J Gastroenterol. 2013;32:381–5. https://doi.org/10.1007/s12664-013-0354-x.
Zhang XH, Andreotti G, Gao YT, Deng J, Liu E, Rashid A, et al. Tea drinking and the risk of biliary tract cancers and biliary stones: a population-based case-control study in Shanghai, China. Int J Cancer. 2006;118:3089–94. https://doi.org/10.1002/ijc.21748.
Chandran AP, Sivarajan R, Srinivasan V, Srinivas M, Jayanthi V. Risk profile for gallstone disease in southern Indian population: is there anything new?. Indian J Gastroenterol. 2014;33:254–7. https://doi.org/10.1007/s12664-014-0453-3.
Yang YC, Lu FH, Wu JS, Wu CH, Chang CJ. The protective effect of habitual tea consumption on hypertension. Arch Intern Med. 2004;164:1534–40. https://doi.org/10.1001/archinte.164.14.1534.
Pan WH, Lee MS, Chuang SY, Lin YC, Fu ML. Obesity pandemic, correlated factors and guidelines to define, screen and manage obesity in Taiwan. Obes Rev. 2008;9(Suppl 1):22–31. https://doi.org/10.1111/j.1467-789X.2007.00434.x.
Organization WH International Association for the Study of Obesity, International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications; 2000.
Saverymuttu SH, Joseph AE, Maxwell JD. Ultrasound scanning in the detection of hepatic fibrosis and steatosis. Br Med J (Clin Res Ed). 1986;292:13–5.
Zhang YP, Li WQ, Sun YL, Zhu RT, Wang WJ. Systematic review with meta-analysis: coffee consumption and the risk of gallstone disease. Aliment Pharmacol Ther. 2015;42:637–48. https://doi.org/10.1111/apt.13328.
Nordenvall C, Oskarsson V, Wolk A. Inverse association between coffee consumption and risk of cholecystectomy in women but not in men. Clin Gastroenterol Hepatol. 2015;13:1096–102 e1091. https://doi.org/10.1016/j.cgh.2014.09.029.
Leitzmann MF, Stampfer MJ, Willett WC, Spiegelman D, Colditz GA, Giovannucci EL. Coffee intake is associated with lower risk of symptomatic gallstone disease in women. Gastroenterology. 2002;123:1823–30. https://doi.org/10.1053/gast.2002.37054.
Douglas BR, Jansen JB, Tham RT, Lamers CB. Coffee stimulation of cholecystokinin release and gallbladder contraction in humans. Am J Clin Nutr. 1990;52:553–6.
Conter RL, Roslyn JJ, Porter-Fink V, DenBesten L. Gallbladder absorption increases during early cholesterol gallstone formation. Am J Surg. 1986;151:184–91.
Shan D, Fang Y, Ye Y, Liu J. EGCG reducing the susceptibility to cholesterol gallstone formation through the regulation of inflammation. Biomed Pharmacother. 2008;62:677–83. https://doi.org/10.1016/j.biopha.2007.12.008.
Chung JH, Kim S, Lee SJ, Chung JO, Oh YJ, Shim SM. Green tea formulations with vitamin C and xylitol on enhanced intestinal transport of green tea catechins. J Food Sci. 2013;78:C685–90. http://doi.org/https://doi.org/10.1111/1750-3841.12112.
Peters CM, Green RJ, Janle EM, Ferruzzi MG. Formulation with ascorbic acid and sucrose modulates catechin bioavailability from green tea. Food Res Int. 2010;43:95–102. https://doi.org/10.1016/j.foodres.2009.08.016.
Simon JA, Hudes ES. Serum ascorbic acid and gallbladder disease prevalence among US adults: the Third National Health and Nutrition Examination Survey (NHANES III). Arch Intern Med. 2000;160:931–6.
Koch W, Kukula-Koch W, Glowniak K. Catechin composition and antioxidant activity of black teas in relation to brewing time. J AOAC Int. 2017;100:1694–9. https://doi.org/10.5740/jaoacint.17-0235.
Labbé D, Tremblay A, Bazinet L. Effect of brewing temperature and duration on green tea catechin solubilization: basis for production of EGC and EGCG-enriched fractions. Sep Purif Technol. 2006;49:1–9. https://doi.org/10.1016/j.seppur.2005.07.038.
Bunsawat K, White DW, Kappus RM, Baynard T. Caffeine delays autonomic recovery following acute exercise. Eur J Prev Cardiol. 2015;22:1473–9. https://doi.org/10.1177/2047487314554867.
Rai G, Baghel V, Rai T, Vyas M. Gall bladder dysfunction in chronic diabetics (type 2): an ultrasonography based prospective study. Int J Res Med Sci. 2016;4:390–97.
Chey WY, Chang T. Neural hormonal regulation of exocrine pancreatic secretion. Pancreatology. 2001;1:320–35.
Weerawatanakorn M, Hung W-L, Pan M-H, Li S, Li D, Wan X, et al. Chemistry and health beneficial effects of oolong tea and theasinensins. Food Sci Human Wellness. 2015;4:133–46. https://doi.org/10.1016/j.fshw.2015.10.002.
Ho KJ, Lin XZ, Yu SC, Chen JS, Wu CZ. Cholelithiasis in Taiwan. Gallstone characteristics, surgical incidence, bile lipid composition, and role of beta-glucuronidase. Dig Dis Sci. 1995;40:1963–73.
Tsai WL, Lai KH, Lin CK, Chan HH, Lo CC, Hsu PI, et al. Composition of common bile duct stones in Chinese patients during and after endoscopic sphincterotomy. World J Gastroenterol. 2005;11:4246–9.
Chen JY, Hsu CT, Liu JH, Tung TH. Clinical predictors of incident gallstone disease in a Chinese population in Taipei, Taiwan. BMC Gastroenterol. 2014;14:83 https://doi.org/10.1186/1471-230X-14-83.
Chen CY, Lu CL, Huang YS, Tam TN, Chao Y, Chang FY, et al. Age is one of the risk factors in developing gallstone disease in Taiwan. Age Ageing. 1998;27:437–41.
Acalovschi M, Buzas C, Radu C, Grigorescu M. Hepatitis C virus infection is a risk factor for gallstone disease: a prospective hospital-based study of patients with chronic viral C hepatitis. J Viral Hepat. 2009;16:860–6. https://doi.org/10.1111/j.1365-2893.2009.01141.x.
Zhang FM, Chen LH, Chen HT, Shan GD, Hu FL, Yang M, et al. Hepatitis C virus infection is positively associated with gallstones in liver cirrhosis. Digestion. 2016;93:221–8. https://doi.org/10.1159/000444252.
Wijarnpreecha K, Thongprayoon C, Panjawatanan P, Manatsathit W, Ungprasert P. Hepatitis B virus infection and risk of gallstones: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2016;28:1437–42. https://doi.org/10.1097/meg.0000000000000754.
Li CH, Yang YC, Wu JS, Huang YH, Lee CT, Lu FH, et al. Increased tea consumption is associated with decreased arterial stiffness in a Chinese population. PLoS ONE. 2014;9:e86022 https://doi.org/10.1371/journal.pone.0086022.
Acknowledgements
We thank the clinical staff of the health examination center in National Cheng Kung University Hospital. We are grateful to Chung-Yi Li for providing the statistical consulting services from the Biostatistics Consulting Center, Clinical Medicine Research Center, National Cheng Kung University Hospital.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Su, FL., Li, CH., Chang, YF. et al. Moderate, but not heavy, tea drinking decreased the associated risk of gallstones in a Taiwanese population. Eur J Clin Nutr 73, 401–407 (2019). https://doi.org/10.1038/s41430-018-0265-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0265-0