Abstract
Background/objectives
To estimate the risks of term-small for gestational age (SGA), preterm-appropriate for gestational age (AGA), and preterm SGA associated with maternal height and body mass index (BMI) and to calculate the population attributable fractions (PAF) of term SGA, preterm AGA, and preterm SGA associated with maternal short stature.
Subjects/methods
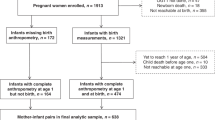
A population-based cohort of 13,230 women with pre-pregnancy height and weight followed from 2012 to 2016 in Sylhet, Bangladesh. We analyzed data of 2655 singleton live born infants. The babies born <37 weeks of gestation were considered preterm and weight <10th percentile of Intergrowth sex-specific gestational age were considered SGA. Risk factors for term SGA, preterm AGA, and preterm SGA were examined using multinomial logistic regression that estimated relative risk ratios (RRR) and 95% confidence intervals (CI).
Results
Maternal short stature <145 cm was significantly associated with term SGA (RRR 1.88, 95% CI 1.37, 2.58; p < 0.001), preterm AGA (RRR 1.45, 95% CI 1.02, 2.05; p < 0.05), and preterm SGA (RRR 14.40, 95% CI 1.82, 113.85; p < 0.05). Maternal underweight status (BMI < 18.5 kg/m2) was significant predictor of term SGA (RRR 1.32, 95% CI 1.10, 1.59; p < 0.01), and preterm AGA (RRR 1.39, 95% CI 1.12, 1.71; p < 0.01). PAF for maternal short stature were 23.2, 7.3, and 73.9% for term SGA, preterm AGA, and preterm SGA, respectively.
Conclusions
To address the problem of undernutrition, Bangladesh needs to strengthen implementation of its multi-sectoral nutrition program comprising nutrition specific and sensitive interventions. Implementation of the program with high coverage and quality would improve maternal nutrition and perinatal outcomes including preterm births and SGA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
UNICEF, WHO. Low Birth Weight: Country. New York: Regional and Global Estimates; 2004. http://www.unicef.org/publications/index_24840.
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller A-B, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–72.
Schlaudecker EP, Munoz FM, Bardaji A, Boghossian NS, Khalil A, Mousa H, et al. Small for gestational age: Case definition & guidelines for data collection, analysis, and presentation of maternal immunisation safety data. Vaccine. 2017;35:6518–28.
Lee AC, Kozuki N, Cousens S, Stevens GA, Blencowe H, Silveira MF, et al. Estimates of burden and consequences of infants born small for gestational age in low and middle income countries with INTERGROWTH-21(st) standard: analysis of CHERG datasets. BMJ. 2017;358:j3677.
Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, Blencowe H, et al. Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–25.
Kozuki N, Katz J, Lee AC, Vogel JP, Silveira MF, Sania A, et al. Short maternal stature increases risk of small-for-gestational-age and preterm births in low- and middle-income countries: individual participant data meta-analysis and population attributable fraction. J Nutr. 2015;145:2542–50.
Kozuki N, Lee AC, Silveira MF, Sania A, Vogel JP, Adair L, et al. The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health. 2013;13(Suppl 3):S2.
Kozuki N, Katz J, LeClerq SC, Khatry SK, West KP Jr., Christian P. Risk factors and neonatal/infant mortality risk of small-for-gestational-age and preterm birth in rural Nepal. J Matern Fetal Neonatal Med. 2015;28:1019–25.
McCowan L, Horgan RP. Risk factors for small for gestational age infants. Best Pract Res Clin Obstet Gynaecol. 2009;23:779–93.
Simas TA, Waring ME, Liao X, Garrison A, Sullivan GM, Howard AE, et al. Prepregnancy weight, gestational weight gain, and risk of growth affected neonates. J Women Health. 2012;21:410–7.
Leng J, Hay J, Liu G, Zhang J, Wang J, Liu H, et al. Small-for-gestational age and its association with maternal blood glucose, body mass index and stature: a perinatal cohort study among Chinese women. BMJ Open. 2016;6:e010984.
Li X, Sundquist K, Sundquist J. Risks of small-for-gestational-age births in immigrants: a nationwide epidemiological study in Sweden. Scand J Public Health. 2012;40:634–40.
Xie C, Epstein LH, Eiden RD, Shenassa ED, Li X, Liao Y, et al. Stunting at 5 Years Among SGA Newborns. Pediatrics. 2016;137:e20152636.
Hayward I, Malcoe LH, Cleathero LA, Janssen PA, Lanphear BP, Hayes MV, et al. Investigating maternal risk factors as potential targets of intervention to reduce socioeconomic inequality in small for gestational age: a population-based study. BMC Public Health. 2012;12:333.
Derraik JG, Lundgren M, Cutfield WS, Ahlsson F. Maternal height and preterm birth: a study on 192,432 Swedish women. PLoS ONE. 2016;11:e0154304.
Vinturache A, McKeating A, Daly N, Sheehan S. M T. Maternal body mass index and the prevalence of spontaneous and elective preterm deliveries in an Irish obstetric population: a retrospective cohort study. BMJ Open. 2017;15:10.
National Institute of Population Research and Training (NIPORT), Ministry of Health and Family Welfare, Mitra and Associates (MA) Bangladesh demographic and health survey 2014. RockVille, Maryland: The DHS program, ICF International; 2016..
Lee ACC, Quaiyum MA, Mullany LC, Mitra DK, Labrique A, Ahmed P, et al. Screening and treatment of maternal genitourinary tract infections in early pregnancy to prevent preterm birth in rural Sylhet, Bangladesh: a cluster randomized trial. BMC Pregnancy and Childbirth. 2015;15:1–14.
Baqui AH, Rosen HE, Lee AC, Applegate JA, El Arifeen S, Rahman SM, et al. Preterm birth and neonatal mortality in a rural Bangladeshi cohort: implications for health programs. J Perinatol. 2013;33:977–81.
Khanam Rasheda, Baqui Abdullah H, Syed MamunIbneMoin, Harrison Meagan, Begum Nazma, Quaiyum Abdul, et al. Can facility delivery reduce the risk of intrapartum complications related perinatal mortality: findings from a cohort study. J Glob Health. 2017;8:010408.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Centers for Disease Control. NHANES 2011–2012 Examination data 2014. http://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Examination&CycleBeginYear=2011 (2014) Accessed on 31 January 2018.
Muhihi A, Sudfeld CR, Smith ER, Noor RA, Mshamu S, Briegleb C, et al. Risk factors for small-for-gestational-age and preterm births among 19,269 Tanzanian newborns. BMC Pregnancy Childbirth. 2016;16:110.
Ozaltin E, Hill K, Subramanian SV. Association of maternal stature with offspring mortality, underweight, and stunting in low- to middle-income countries. JAMA. 2010;303:1507–16.
Kramer MS, McLean FH, Eason EL, Usher RH. Maternal nutrition and spontaneous preterm birth. Am J Epidemiol. 1992;136:574–83.
Schaible UE, Kaufmann SH. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4:e115.
Fowden AL, Forhead AJ, Coan PM, Burton GJ. The placenta and intrauterine programming. J Neuroendocrinol. 2008;20:439–50.
Timasheva Y, Putku M, Kivi R, Kozich V, Mannik J, Laan M. Developmental programming of growth: genetic variant in GH2 gene encoding placental growth hormone contributes to adult height determination. Placenta. 2013;34:995–1001.
Rodriguez G, Ventura P, Samper MP, Moreno L, Sarria A, Perez-Gonzalez JM. Changes in body composition during the initial hours of life in breast-fed healthy term newborns. Biol Neonate. 2000;77:12–6.
Gernand AD, Paul RR, Ullah B, Taher MA, Witter FR, Wu L, et al. A home calendar and recall method of last menstrual period for estimating gestational age in rural Bangladesh: a validation study. J Health Popul Nutr. 2016;35:34.
Osmani SR, Ahmed A, Ahmed T, Hossain N, Huq S, A. S. Strategic Review of Food Security and Nutrition in Bangladesh. Executive Summary. Rome, Italy: World Food Programme; 2016.
Mitra SN, Ahmed A1-Sabir, Anne R, Cross, Jamil. K Bangladesh Demographic and Health Survey, 1996-1997. Dhaka and Calverton, Maryland: National Institute of Population Research and Training (NIPORT), Mitra and Associates, and Macro International Inc.; 1997.
National Institute of Population Research and Training (NIPORT), Mitra and Associates (MA), ICF International Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and Calverton, Maryland, USA: NIPORT, Mitra and Associates, and ICF International.; 2013.
Nisbett N, Davis P, Yosef S, Akhtar N. Bangladesh’s story of change in nutrition: Strong improvements in basic and underlying determinants with an unfinished agenda for direct community level support. Glob Food Secur. 2017;13:21–9.
Unicef. Learning from nutrition programme evaluations: a thematic evaluation synthesis report. https://www.unicef.org/evaluation/files/Final_learning_from_nutrition_17_07_2014.pdf (2014) Accessed on 11 May 2018.
Majumder MAA. World health statistics 2011: how does Bangladesh compare with other south-east Asian countries. South East Asia. J Public Health. 2013;1:4–11.
Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77.
Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR, et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet. 2008;371:1936–44.
Acknowledgements
We acknowledge the contribution of the study women and the dedication of Projahnmo field team. Projahnmo is a research partnership of Johns Hopkins University, the Bangladesh Ministry of Health and Family Welfare and other Bangladeshi institutions including ICDDR,B, and Shimantik.
Author contributions
RK and AHB conceived and designed the analysis. AHB, ACL, DKM, SDG, AQ, LCM were involved in project implementation and conduct of study procedures. SDG developed and maintained the database with LCM. MR conducted data cleaning and analyses with RK. RK drafted the first version of the manuscript. All authors read, provided technical input and approved the final manuscript.
Funding
The study was funded by grants from the NICHD (R01 HD066156-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Khanam, R., Lee, A.C., Mitra, D.K. et al. Maternal short stature and under-weight status are independent risk factors for preterm birth and small for gestational age in rural Bangladesh. Eur J Clin Nutr 73, 733–742 (2019). https://doi.org/10.1038/s41430-018-0237-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0237-4
This article is cited by
-
Etiological subgroups of term small-for-gestational-age and childhood health outcomes
Pediatric Research (2023)
-
Risk Factors of Preterm Birth in Okinawa Prefecture, the Southernmost Island Prefecture of Japan
Maternal and Child Health Journal (2023)
-
Pregnancy, delivery, and neonatal outcomes among women living with Down syndrome: a matched cohort study, utilizing a population database
Archives of Gynecology and Obstetrics (2023)
-
The Effect of Structural Gender Inequality Revealed in Small for Gestational Age
Global Social Welfare (2022)
-
Novel sex-specific influence of parental factors on small-for-gestational-age newborns
Scientific Reports (2020)