Abstract
Background/Objectives
A small number of case–control studies have suggested that mitochondrial haplogroups could be associated with obesity. We examined whether obesity risk was influenced by mitochondrial haplogroup in a large North American cohort across an 8-year period. We conducted a longitudinal cohort study including individuals from the Osteoarthritis Initiative.
Subjects/Methods
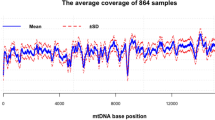
Mitochondrial haplogroups were determined by sequencing and PCR-RFLP techniques using this nomenclature: HV, JT, KU, IWX, and super HV/others. The strength of the association between mitochondrial haplogroups and incident obesity was quantified with hazard ratios (HRs), adjusted for potential confounders using a Cox’s regression analysis.
Results
Overall, 2342 non-obese Caucasian participants (56.7% women) with a mean ± SD age of 62.0 ± 9.5 years at baseline were included. During a median follow-up of 8 years, 334 individuals ( = 14.3% of baseline population) became obese. After adjusting for nine potential confounders, the haplogroups IWX carried a significant 48% higher risk of obesity (HR = 1.48; 95% CI: 1.02–2.39) compared to the HV haplotype (the most frequent type).
Conclusion
Only the presence of the IWX haplogroups appears to be linked to increased obesity risk, independent of potential baseline confounders. Future cohort studies are needed to confirm these findings and to determine potential underlying mechanisms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wang Y, Brinton RD. Triad of risk for late onset Alzheimer’s: mitochondrial haplotype, APOE genotype and chromosomal sex. Front Aging Neurosci. 2016;8:232.
Copeland WC, Longley MJ. Mitochondrial genome maintenance in health and disease. DNA Repair (Amst). 2014;19:190–8.
Wallace DC, Chalkia D. Mitochondrial DNA genetics and the heteroplasmy conundrum in evolution and disease. Cold Spring Harb Perspect Biol. 2013;5:a021220.
Picard M, Wallace DC, Burelle Y. The rise of mitochondria in medicine. Mitochondrion. 2016;30:105–16.
Mishmar D, Ruiz-Pesini E, Golik P, Macaulay V, Clark AG, Hosseini S, et al. Natural selection shaped regional mtDNA variation in humans. Proc Natl Acad Sci USA. 2003;100:171–6.
Veronese N, Stubbs B, Solmi M, Vaona A, Demurtas J, Carvalho AF, et al. Mitochondrial genetic haplogroups and depressive symptoms: A large study among people in North America. J Affect Disord. 2017;217:55–9.
Wortmann SB, Zweers-van Essen H, Rodenburg RJ, van den Heuvel LP, de Vries MC, Rasmussen-Conrad E, et al. Mitochondrial energy production correlates with the age-related BMI. Pediatr Res. 2009;65:103–8.
Yang TL, Guo Y, Shen H, Lei SF, Liu YJ, Li J, et al. Genetic association study of common mitochondrial variants on body fat mass. PLoS ONE. 2011;6:e21595.
Nardelli C, Labruna G, Liguori R, Mazzaccara C, Ferrigno M, Capobianco V, et al. Haplogroup T is an obesity risk factor: mitochondrial DNA haplotyping in a morbid obese population from southern Italy. BioMed Res Int. 2013;2013:631082.
Ebner S, Mangge H, Langhof H, Halle M, Siegrist M, Aigner E, et al. Mitochondrial Haplogroup T is associated with obesity in austrian juveniles and adults. PLoS One 2015;10:e0135622.
Grant SF, Glessner JT, Bradfield JP, Zhao J, Tirone JE, Berkowitz RI, et al. Lack of relationship between mitochondrial heteroplasmy or variation and childhood obesity. Int J Obes (Lond). 2012;36:80–3.
Rego-Perez I, Fernandez-Moreno M, Fernandez-Lopez C, Arenas J, Blanco FJ. Mitochondrial DNA haplogroups: role in the prevalence and severity of knee osteoarthritis. Arthritis Rheum. 2008;58:2387–96.
Torroni A, Huoponen K, Francalacci P, Petrozzi M, Morelli L, Scozzari R, et al. Classification of European mtDNAs from an analysis of three European populations. Genetics. 1996;144:1835–50.
Marty CB, Marie TL, Kevin CN, Syawal S, Shamkant BN, Pierre B, Douglas CW. MITOMAP: a human mitochondrial genome database—2004 update. Nucleic Acids Research. 2005;33:D611–D613.
Fernandez-Caggiano M, Barallobre-Barreiro J, Rego-Perez I, Crespo-Leiro MG, Paniagua MJ, Grille Z, et al. Mitochondrial haplogroups H and J: risk and protective factors for ischemic cardiomyopathy. PLoS ONE. 2012;7:e44128.
WHO Consultation on Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series, Geneva 1–253; 894: i–xii, 2000.
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–51.
Veronese N, Stubbs B, Noale M, Solmi M, Vaona A. demurtas J, et al. Fried potato consumption is associated with elevated mortality: an 8-year longitudinal cohort study. Am J Clin Nutr. 2017;106:162–67.
Ruiz-Pesini E, Mishmar D, Brandon M, Procaccio V, Wallace DC. Effects of purifying and adaptive selection on regional variation in human mtDNA. Science. 2004;303:223–6.
Hulgan T, Haubrich R, Riddler SA, Tebas P, Ritchie MD, McComsey GA, et al. European mitochondrial DNA haplogroups and metabolic changes during antiretroviral therapy in AIDS Clinical Trials Group Study A5142. AIDS. 2011;25:37–47.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980– 2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Herrera BM, Lindgren CM. The genetics of obesity. Curr Diab Rep. 2010;10:498–505.
Emilsson V, Thorleifsson G, Zhang B, Leonardson AS, Zink F, Zhu J, et al. Genetics of gene expression and its effect on disease. Nature. 2008;452:423–8.
Hill JO, Wyatt HR, Peters JC. Energy balance and obesity. Circulation. 2012;126:126–32.
Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–67.
Barnes AS. Obesity and sedentary lifestyles: Risk for cardiovascular disease in women. Tex Heart Inst J. 2012;39:224–7.
Caudwell P, Gibbons C, Finlayson G, Näslund E, Blundell J. Physical activity, energy intake, and obesity: The links between exercise and appetite. Curr Obes Rep. 2013;2:185–90.
Bradfield JP, Taal HR, Timpson NJ, Scherag A, Lecoeur C, Warrington NM, et al. A genome-wide association meta-analysis identifies new childhood obesity loci. Nat Genet. 2012;44:526–31.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
Hu F. Obesity epidemiology. (New York, Oxford University Press, 2008).
Pea A, Yu J, Rezaee N, et al. Targeted DNA sequencing reveals pattern of local progression in the pancreatic remnant following resection of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann Surg. 2017;266:133–141.
Yachida S, Wood LD, Suzuki M, et al. Genomic sequencing identifies ELF3 as a driver of ampullary carcinoma. Cancer Cell. 2016;29:229–240.
Saki M, Prakash A. DNA damage related crosstalk between the nucleus and mitochondria. Free Radic Biol Med. 2017;107:216–227.
Meschia JF, Ross OA. Does mitochondrial DNA have a protective role in stroke? Lancet Neurol. 2010;9:453–4.
Funding
The OAI is funded by the National Institute of Health. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. Funding sources had no role in study design, data treatment, or report writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Veronese, N., Stubbs, B., Koyanagi, A. et al. Mitochondrial genetic haplogroups and incident obesity: a longitudinal cohort study. Eur J Clin Nutr 72, 587–592 (2018). https://doi.org/10.1038/s41430-018-0097-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0097-y
This article is cited by
-
Single nucleotide polymorphism genes and mitochondrial DNA haplogroups as biomarkers for early prediction of knee osteoarthritis structural progressors: use of supervised machine learning classifiers
BMC Medicine (2022)
-
mtDNA haplogroup A enhances the effect of obesity on the risk of knee OA in a Mexican population
Scientific Reports (2022)
-
Mitochondrial haplogroup J associated with higher risk of obesity in the Qatari population
Scientific Reports (2021)