Abstract
Background/objectives
Increased age is strongly associated with anorexia and protein-energy wasting (PEW) in maintenance hemodialysis (MHD) population. We hypothesized that the association of obestatin, a recently discovered anorexigenic gut hormone, with appetite and nutritional status differs by age groups.
Subjects/methods
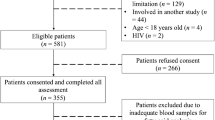
We performed a cross-sectional study on 261MHD patients. Obestatin, acyl-ghrelin, markers of inflammation (CRP, IL-6, TNF-α) and nutrition (self-reported appetite, dietary intake, biochemical nutritional parameters, and body composition) were measured.
Results
Obestatin was associated with appetite in multivariate analyses even after controlling for such confounders as lean body mass (LBM), IL-6 and acyl-ghrelin in patients younger than 71 years. For each ng/ml increase in obestatin levels, the odds for diminished appetite was 0.75 (95% CI: 0.59–0.96). However, these associations were not observed in patients 71 years and older. Multivariable logistic regression models (including appetite) also showed increasing odds for PEW (defined by ESPEN consensus-based criteria for the diagnosis of malnutrition) across increasing serum obestatin levels (OR: 1.51, 95% CI: 1.05–2.18) in patients 71 years and older. However, after lean body mass (LBM) was added to this model, the association between obestatin and malnutrition was abolished (OR: 1.26, 95% CI: 0.83–1.91).
Conclusions
The association between serum obestatin, appetite and PEW differs depending on age in MHD patients. A positive link with appetite exists in patients younger than 71 years, whereas this relationship disappears by the age of 71. In older MHD patients, obestatin is associated with PEW through mechanisms related to LBM, but not to appetite.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bossola M, Tazza L, Giungi S, Luciani G. Anorexia in hemodialysis patients: an update. Kidney Int. 2006;70:417–22.
Zhang JV, Ren PG, Avsian-Kretchmer O, Luo CW, Rauch R, Klein C, et al. Obestatin, a peptide encoded by the ghrelin gene, opposes ghrelin’s effects on food intake. Science. 2005;310:996–9.
Borges N, Moraes C, Barros AF, Carraro-Eduardo JC, Fouque D, Mafra D. Acyl-ghrelin and obestatin plasma levels in different stages of chronic kidney disease. J Ren Nutr. 2014;24:100–4.
Xing YX, Yang L, Kuang HY, Gao XY, Liu HL. Function of obestatin in the digestive system. Nutrition. 2017;34:21–8.
Depoortere I, Thijs T, Moechars D, De Smet B, Ver Donck L, Peeters TL. Effect of peripheral obestatin on food intake and gastric emptying in ghrelin-knockout mice. Br J Pharmacol. 2008;153:1550–7.
Zizzari P, Longchamps R, Epelbaum J, Bluet-Pajot MT. Obestatin partially affects ghrelin stimulation of food intake and growth hormone secretion in rodents. Endocrinology. 2007;148:1648–53.
Beasley JM, Ange BA, Anderson CA, Miller ER 3rd, Erlinger TP, Holbrook JT, et al. Associations between macronutrient intake and self-reported appetite and fasting levels of appetite hormones: results from the Optimal Macronutrient Intake Trial to Prevent Heart Disease. Am J Epidemiol. 2009;169:893–900.
Mafra D, Guebre-Egziabher F, Cleaud C, Arkouche W, Mialon A, Drai J, et al. Obestatin and ghrelin interplay in hemodialysis patients. Nutrition. 2010;26:1100–4.
Lacquaniti A, Bolignano D, Donato V, Chirico V, Romeo A, Loddo S, et al. Obestatin: a new element for mineral metabolism and inflammation in patients on hemodialysis. Kidney Blood Press Res. 2011;34:104–10.
Beberashvili I, Sinuani I, Azar A, Kadoshi H, Shapiro G, Feldman L, et al. Low serum concentration of obestatin as a predictor of mortality in maintenance hemodialysis patients. Biomed Res Int. 2013;2013:796586.
Lippl F, Erdmann J, Lichter N, Tholl S, Wagenpfeil S, Adam O, et al. Relation of plasma obestatin levels to bmi, gender, age and insulin. Horm Metab Res. 2008;40:806–12.
Beasley JM, Ange BA, Anderson CA, Miller Iii ER, Holbrook JT, Appel LJ. Characteristics associated with fasting appetite hormones (obestatin, ghrelin, and leptin). Obes (Silver Spring). 2009;17:349–54.
Wolfson M. Nutrition in elderly dialysis patients. Semin Dial. 2002;15:113–5.
Johansson L. Nutrition in older adults on peritoneal dialysis. Perit Dial Int. 2015;35:655–8.
Burrowes JD, Cockram DB, Dwyer JT, Larive B, Paranandi L, Bergen C, et al. Cross-sectional relationship between dietary protein and energy intake, nutritional status, functional status, and comorbidity in older versus younger hemodialysis patients. J Ren Nutr. 2002;12:87–95.
Ohkawa S, Odamaki M, Ikegaya N, Hibi I, Miyaji K, Kumagai H. Association of age with muscle mass, fat mass and fat distribution in non-diabetic haemodialysis patients. Nephrol Dial Transplant. 2005;20:945–51.
Beberashvili I, Sinuani I, Azar A, Shapiro G, Feldman L, Stav K, et al. Serum uric acid as a clinically useful nutritional marker and predictor of outcome in maintenance hemodialysis patients. Nutrition. 2015;31:138–47.
Fouque D, Vennegoor M, ter Wee P, Wanner C, Basci A, Canaud B. et al. EBPG guideline on nutrition. Nephrol Dial Transplant. 2007;22:ii45–87.
Depner TA, Daugirdas JT. Equations for normalized protein catabolic rate based on two-point modeling of hemodialysis urea kinetics. J Am Soc Nephrol. 1996;7:780–5.
Rambod M, Bross R, Zitterkoph J, Benner D, Pithia J, Colman S, et al. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. Am J Kidney Dis. 2009;53:298–309.
Beberashvili I, Azar A, Sinuani I, Kadoshi H, Shapiro G, Feldman L, et al. Comparison analysis of nutritional scores for serial monitoring of nutritional status in hemodialysis patients. Clin J Am Soc Nephrol. 2013;8:443–51.
Yamada K, Furuya R, Takita T, Maruyama Y, Yamaguchi Y, Ohkawa S, et al. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr. 2008;87:106–13.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - An ESPEN consensus statement. Clin Nutr. 2015;34:335–40.
Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010;77:141–51.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, et al. ESPEN. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23:1430–53.
Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C. Single prediction equation for bioelectrical impedance analysis in adults aged 20--94 years. Nutrition. 2001;17:248–53.
Hassouna R, Zizzari P, Tolle V. The ghrelin/obestatin balance in the physiological and pathological control of growth hormone secretion, body composition and food intake. J Neuroendocrinol. 2010;22:793–804.
Bossola M, Muscaritoli M, Valenza V, Panocchia N, Tazza L, Cascino A, et al. Anorexia and serum leptin levels in hemodialysis patients. Nephron Clin Pract. 2004;97:c76–82.
Wright M, Woodrow G, O’Brien S, King N, Dye L, Blundell J, et al. Disturbed appetite patterns and nutrient intake in peritoneal dialysis patients. Perit Dial Int. 2003;23:550–6.
Chang CC, Chen HL, Hung CH, Hwang KL, Lin CY. Single meal food intake characteristics reliably predict nutrition status and body composition in patients undergoing continuous peritoneal dialysis. Nephrol (Carlton). 2007;12:337–41.
Germain N, Galusca B, Grouselle D, Frere D, Billard S, Epelbaum J, et al. Ghrelin and obestatin circadian levels differentiate bingeing-purging from restrictive anorexia nervosa. J Clin Endocrinol Metab. 2010;95:3057–62.
Caliskan Y, Yelken B, Gorgulu N, Ozkok A, Yazici H, Telci A, et al. Comparison of markers of appetite and inflammation between hemodialysis patients with and without failed renal transplants. J Ren Nutr. 2012;22:258–67.
Ashby DR, Ford HE, Wynne KJ, Wren AM, Murphy KG, Busbridge M, et al. Sustained appetite improvement in malnourished dialysis patients by daily ghrelin treatment. Kidney Int. 2009;76:199–206.
Hung AM, Ikizler TA. Factors determining insulin resistance in chronic hemodialysis patients. Contrib Nephrol. 2011;171:127–34.
Germain N, Galusca B, Grouselle D, Frere D, Tolle V, Zizzari P, et al. Ghrelin/obestatin ratio in two populations with low body weight: constitutional thinness and anorexia nervosa. Psychoneuroendocrinology. 2009;34:413–9.
Guo ZF, Zheng X, Qin YW, Hu JQ, Chen SP, Zhang Z. Circulating preprandial ghrelin to obestatin ratio is increased in human obesity. J Clin Endocrinol Metab. 2007;92:1875–80.
Mafra D, Guebre-Egziabher F, Fouque D. Endocrine role of stomach in appetite regulation in chronic kidney disease: about ghrelin and obestatin. J Ren Nutr. 2010;20:68–73.
Wright MJ, Woodrow G, O’Brien S, King NA, Dye L, Blundell JE, et al. A novel technique to demonstrate disturbed appetite profiles in haemodialysis patients. Nephrol Dial Transplant. 2001;16:1424–9.
Fassett RG1, Robertson IK, Geraghty DP, Ball MJ, Coombes JS. Dietary intake of patients with chronic kidney disease entering the LORD trial: adjusting for underreporting. J Ren Nutr. 2007;17:235–42.
Biasioli S, Foroni R, Petrosino L, Cavallini L, Zambello A, Cavalcanti G, et al. Effect of aging on the body composition of dialyzed subjects. Comparison with normal subjects. ASAIO J. 1993;39:M596–601.
Nolph KD, Moore HL, Prowant B, Meyer M, Twardowski ZJ, Khanna R, et al. Age and indices of adequacy and nutrition in CAPD patients. Adv Perit Dial. 1993;9:87–91.
Harper EJ. Changing perspectives on aging and energy requirements: aging and energy intakes in humans, dogs and cats. J Nutr. 1998;128:2623S–6S.
Roberts SB, Fuss P, Heyman MB, Young VR. Influence of age on energy requirements. Am J Clin Nutr. 1995;62:1053S–8S.
Eftekhari MH, Ranjbar-Zahedani M, Basiratnia M, Rezaianzadeh A, Faghih S. Comparison of appetite-regulating hormones and body composition in pediatric patients in predialysis stage of chronic kidney disease and healthy control group. Iran J Med Sci. 2015;40:27–33.
Zamrazilová H, Hainer V, Sedlácková D, Papezová H, Kunesová M, et al. Plasma obestatin levels in normal weight, obese and anorectic women. Physiol Res. 2008;57:S49–55.
Mora M, Granada ML, Palomera E, Serra-Prat M, Puig-Domingo M, Mataró Ageing Study Group.. Obestatin is associated to muscle strength, functional capacity and cognitive status in old women. Age (Dordr). 2013;35:2515–23.
Wang YW, Lin TY, Peng CH, Huang JL, Hung SC. Factors Associated with Decreased Lean Tissue Index in Patients with Chronic Kidney Disease. Nutrients. 2017;9:5.
Pupim LB, Heimbürger O, Qureshi AR, Ikizler TA, Stenvinkel P. Accelerated lean body mass loss in incident chronic dialysis patients with diabetes mellitus. Kidney Int. 2005;68:2368–74.
Kim JK, Choi SR, Choi MJ, Kim SG, Lee YK, et al. Prevalence of and factors associated with sarcopenia in elderly patients with end-stage renal disease. Clin Nutr. 2014;33:64–8.
Feng DD, Yang SK, Loudes C, Simon A, Al-Sarraf T, Culler M, et al. Ghrelin and obestatin modulate growth hormone-releasing hormone release and synaptic inputs onto growth hormone-releasing hormone neurons. Eur J Neurosci. 2011;34:732–44.
Fuoco D, Kilgour RD, Vigano A. A hypothesis for a possible synergy between ghrelin and exercise in patients with cachexia: Biochemical and physiological bases. Med Hypotheses. 2015;85:927–33.
Anderwald-Stadler M, Krebs M, Promintzer M, Mandl M, Bischof MG, Nowotny P, et al. Plasma obestatin is lower at fasting and not suppressed by insulin in insulin-resistant humans. Am J Physiol Endocrinol Metab. 2007;293:E1393–8.
Hung AM, Ikizler TA. Factors determining insulin resistance in chronic hemodialysis patients. Contrib Nephrol. 2011;171:127–34.
Huda MS, Durham BH, Wong SP, Deepak D, Kerrigan D, McCulloch P, et al. Plasma obestatin levels are lower in obese and post-gastrectomy subjects, but do not change in response to a meal. Int J Obes (Lond). 2008;32:129–35.
Acknowledgements
The authors appreciate the language editing of Dr. Mechael Kanovsky, which has greatly improved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Katkov, A., Sinuani, I., Azar, A. et al. Age modifies the association between serum obestatin, appetite and nutritional status in maintenance hemodialysis patients. Eur J Clin Nutr 72, 1007–1018 (2018). https://doi.org/10.1038/s41430-018-0087-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-018-0087-0