Abstract
Background/objectives
The use of simple screening tools to measure nutritional adequacy in a public health context in developed countries are currently lacking. We explore the relationship between food variety and nutrient intake of London school children using a simple tool with potential use for screening for inadequate diets.
Subjects/methods
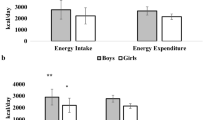
A cross-sectional survey was carried out in 2010. The survey included 2579 children aged 7−10 years in 52 primary schools in East London in the United Kingdom. The analysis included 2392 children (93% of the original sample). Food variety was assessed as the total number of listed foods recorded over 24 h using the validated Child and Diet Assessment Tool (CADET) comprising 115 listed foods divided into 16 food categories. Dietary quality was determined by the proportion of children meeting recommended intakes of individual micronutrients, namely, calcium, iron, zinc, folate, vitamin A and vitamin C.
Results
The mean number of CADET-listed foods consumed daily by children was 17.1 (95% CI: 16.8, 17.5). Children who consumed fewer than 11 foods on the collection day had particularly low nutrient intakes. Children consuming three different vegetables and two different fruits on average consumed 19–20 listed foods. It was estimated between 4 and 20% of children did not meet the recommended levels for individual micronutrients during the period of data collection.
Conclusions
A simple method using food counts to assess daily food variety may help public health nutritionists identify groups of children at risk of inadequate diets.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
World Health Organization. Obesity and overweight. Fact sheet No 311 (WHO, Geneva, 2015).
Schwingshackl L, Hoffmann G, Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115:780–800.e785. https://doi.org/10.1016/j.jand.2014.12.009.
Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC, Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–84. https://doi.org/10.1016/j.maturitas.2011.08.005.
Public Health England. National diet and nutrition survey: results from years 1-4 (combined) of the rolling programme (2008/2009-11/12). Executive summary (Public Health England, London, 2015).
Drewnowski A, Rehm CD, Socioeconomic gradient in consumption of whole fruit and 100% fruit juice among US children and adults. Nutr J. 2015;14:3. https://doi.org/10.1186/1475-2891-14-3.
Rose D. Economic determinants and dietary consequences of food insecurity in the United States. J Nutr. 1999;129:517S–520S.
Arimond M, Ruel MT. Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. J Nutr. 2004;134:2579–85.
Sharkey JR, Nalty C, Johnson CM, Dean WR, Children’s very low food security is associated with increased dietary intakes in energy, fat, and added sugar among Mexican-origin children (6-11 y) in Texas border Colonias. BMC Pediatr. 2012;12:16. https://doi.org/10.1186/1471-2431-12-16.
Mendoza JA, Drewnowski A, Cheadle A, Christakis DA. Dietary energy density is associated with selected predictors of obesity in U.S. children. J Nutr. 2006;136:1318–22.
Dinour LM, Bergen D, Yeh MC, The food insecurity-obesity paradox: a review of the literature and the role food stamps may play. J Am Diet Assoc. 2007;107:1952–61. https://doi.org/10.1016/j.jada.2007.08.006.
Alkerwi Aa, Diet quality concept. Nutr J. 2014;30:613–8. https://doi.org/10.1016/j.nut.2013.10.001.
Golley RK, Hendrie GA, McNaughton SA, Scores on the dietary guideline index for children and adolescents are associated with nutrient intake and socio-economic position but not adiposity. J Nutr. 2011;141:1340–7. https://doi.org/10.3945/jn.110.136879.
Guenther PM, Reedy J, Krebs-Smith SM, Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108:1896–901. https://doi.org/10.1016/j.jada.2008.08.016.
Marshall S, Burrows T, Collins CE, Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J Hum Nutr Diet. 2014;27:577–98. https://doi.org/10.1111/jhn.12208.
Woodruff SJ, Hanning RM, McGoldrick K, Brown KS. Healthy eating index-C is positively associated with family dinner frequency among students in grades 6-8 from Southern Ontario, Canada. Eur J Clin Nutr. 2010;64:454–60.
Kleiser C, Mensink GBM, Scheidt-Nave C, Kurth B-M, HuSKY: a healthy nutrition score based on food intake of children and adolescents in Germany. Brit J Nutr. 2009;102:610–8. https://doi.org/10.1017/S0007114509222689.
Kohlboeck G, Sausenthaler S, Standl M, Koletzko S, Bauer CP, von Berg A, et al. Food intake, diet quality and behavioral problems in children: Results from the GINI-plus/LISA-plus studies. Ann Nutr Metab. 2012;60:247–56.
Marshall S, Watson J, Burrows T, Guest M, Collins CE, The development and evaluation of the Australian child and adolescent recommended food score: a cross-sectional study. Nutr J. 2012;11:96. https://doi.org/10.1186/1475-2891-11-96.
Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2007;7:931–5. https://doi.org/10.1079/PHN2004556.
Zimmer MH, Hart LC, Manning-Courtney P, Murray DS, Bing NM, Summer S, Food variety as a predictor of nutritional status among children with autism. J Autism Dev Dis. 2012;42:549–56. https://doi.org/10.1007/s10803-011-1268-z.
Krebs-Smith SM, Smiciklas-Wright H, Guthrie HA, Krebs-Smith J. The effects of variety in food choices on dietary quality. J Am Diet Assoc. 1987;87:897–903.
Masset G, Scarborough P, Rayner M, Mishra G, Brunner EJ, Can nutrient profiling help to identify foods which diet variety should be encouraged? Results from the Whitehall II cohort. Brit J Nutr. 2015;113:1800–9. https://doi.org/10.1017/S000711451500094X.
Murphy SP, Foote JA, Wilkens LR, Basiotis PP, Carlson A, White KKL, et al. Simple measures of dietary variety are associated with improved dietary quality. J Am Diet Assoc. 2006;106:425–9. https://doi.org/10.1016/j.jada.2005.12.003.
Mark S, Lambert M, O’Loughlin J, Gray-Donald K. Household income, food insecurity and nutrition in Canadian youth. Can J Public Health. 2012;103:94–99.
Campbell AA, Akhter N, Sun K, De Pee S, Kraemer K, Moench-Pfanner R, et al. Relationship of household food insecurity to anaemia in children aged 6-59 months among families in rural Indonesia. Ann Trop Paediatr. 2011;31:321–30. https://doi.org/10.1179/1465328111Y.0000000038.
Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J Nutr. 2008;138:604–12.
Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325:1202.
Lee D-H, Anderson KE, Harnack LJ, Folsom AR, Jacobs DR,Jr., Heme iron, zinc, alcohol consumption, and colon cancer: Iowa Women’s Health Study. J Natl Cancer Inst. 2004;96:403–7. https://doi.org/10.1093/jnci/djh047.
Grantham-McGregor S, Ani C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr. 2001;131:649S–668S.
Evans CE, Mandl V, Christian MS, Cade JE. Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr. 2015;19:36–45. https://doi.org/10.1017/S1368980015000853.
Department of Health. Dietary reference values for food energy and nutrients for the United Kingdom (HMSO, London, 1991).
Christian MS, El Evans C, Conner M, Ransley JK, Cade JE, Study protocol: can a school gardening intervention improve children’s diets?. BMC Public Health. 2012;12:304. https://doi.org/10.1186/1471-2458-12-304.
Christian MS, Evans CE, Hancock N, Nykjaer C, Cade JE, Family meals can help children reach their 5 a day: a cross-sectional survey of children’s dietary intake from London primary schools. J Epidemiol Community Health. 2013;67:332–8. https://doi.org/10.1136/jech-2012-201604.
Cade JE, Frear L, Greenwood DC. Assessment of diet in young children with an emphasis on fruit and vegetable intake: using CADET--Child and Diet Evaluation Tool. Public Health Nutr. 2006;9:501–8.
Christian MS, Evans CE, Nykjaer C, Hancock N, Cade JE, Measuring diet in primary school children aged 8-11 years: validation of the Child and Diet Evaluation Tool (CADET) with an emphasis on fruit and vegetable intake. Eur J Clin Nutr. 2015;69:234–41. https://doi.org/10.1038/ejcn.2014.160.
Wrieden WL, Longbottom PJ, Adamson AJ, Ogston SA, Payne A, Haleem MA, et al. Estimation of typical food portion sizes for children of different ages in Great Britain. Brit J Nutr. 2008;99:1344–53. https://doi.org/10.1017/S0007114507868516.
Christian MS, Evans CE, Nykjaer C, Hancock N, Cade JE, Evaluation of the impact of a school gardening intervention on children’s fruit and vegetable intake: a randomised controlled trial. Int J Behav Nutr Phys Act. 2014;11:99. https://doi.org/10.1186/s12966-014-0099-7.
Department of Health. SACN dietary reference values for energy, 2012. https://www.gov.uk/government/publications/sacn-dietary-reference-values-for-energy.
Department of Health. National child measurement programme, 2009. https://www.gov.uk/government/collections/national-child-measurement-programme.
National Centre for Social Research. Health survey for England: obesity among children under 11, 2005. http://webarchive.nationalarchives.gov.uk/20130123211345/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsStatistics/DH_4109245.
Stamatakis E, Primatesta P, Chinn S, Rona R, Falascheti E. Overweight and obesity trends from 1974 to 2003 in English children: what is the role of socioeconomic factors? 4. Arch Dis Child. 2005;90:999–1004.
Jenkins G. 1.6 million children in the UK live in severe poverty: the government must do more to target areas of high deprivation, poverty and worklessness (British Politics and Policy at LSE, London, 2011).
Molcho M, Gabhainn SN, Kelly C, Friel S, Kelleher C, Food poverty and health among schoolchildren in Ireland: findings from the Health Behaviour in School-aged Children (HBSC) study. Public Health Nutr. 2007;10:364–70. https://doi.org/10.1017/S1368980007226072.
Pilgrim A, Barker M, Jackson A, Ntani G, Crozier S, Inskip H, et al. Does living in a food insecure household impact on the diets and body composition of young children? Findings from the Southampton Women’s Survey. J Epidemiol Commity Health. 2012;66:e6. https://doi.org/10.1136/jech.2010.125476.
USDA ERS. Household food security in the United States (USDA, Washington, DC, 2015).
Bhattacharya J, Currie J, Haider S, Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23:839–62. https://doi.org/10.1016/j.jhealeco.2003.12.008.
Kleinman RE, Murphy JM, Little M, Pagano M, Wehler CA, Regal K, et al. Hunger in children in the United States: potential behavioral and emotional correlates. Pediatrics. 1998;101:E3.
Lazarou C, Newby PK, Use of dietary indexes among children in developed countries. Adv Nutr. 2011;2:295–303. https://doi.org/10.3945/an.110.000166.
Acknowledgements
The authors acknowledge Claire McLoughlin and Camilla Nykjaer for their central involvement in collecting the data for this project.
Author contributions
CELE designed the research protocol and the original statistical analysis plan, secured the additional funding for the additional analysis, wrote the first manuscript and contributed to all versions of the manuscript. JH designed and carried out the analysis, wrote a report and contributed to all versions of the manuscript. JEC contributed to all versions of the manuscript. NH managed the database, made available all data in the analysis and contributed to the final version of the manuscript. MSC managed the data collection of the NIHR project and contributed to the final version of the manuscript.
Funding
This project was funded by the National Institute for Health Research Public Health Research (NIHR PHR) programme (project number 09/3001/19); visit the PHR programme website for more information.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CELE, JH, NH, MSC and JEC had financial support from the UK-based charity, Kids Company®, for the submitted work. Kids Company® had no role in the design, analysis or writing of this article. CELE, JH, NH, MSC and JEC have no other relationships with companies that might have an interest in the submitted work.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Evans, C., Hutchinson, J., Christian, M. et al. Measures of low food variety and poor dietary quality in a cross-sectional study of London school children. Eur J Clin Nutr 72, 1497–1505 (2018). https://doi.org/10.1038/s41430-017-0070-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-017-0070-1
This article is cited by
-
Dietary practices and associated factors among pregnant women in West Gojjam Zone, Northwest Ethiopia
BMC Pregnancy and Childbirth (2020)