Abstract
Background/objectives
Milk contributes with saturated fat, but randomized controlled trials (RCT) on the effects of dairy on the risk of type 2 diabetes (T2D) where dairy is given as whole foods are scarce. The objective of our study was to investigate the long-term effects of semi-skimmed milk on insulin sensitivity and further to compare milk with sugar-sweetened soft drinks (SSSD).
Subjects/methods
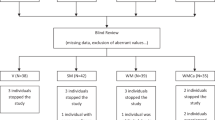
A secondary analysis of a 6-month RCT with 60 overweight and obese subjects randomly assigned to 1 L/d of either milk (1.5 g fat/100 mL), SSSD, non-calorie soft drink (NCSD), or water was conducted. Insulin sensitivity was evaluated by oral glucose tolerance test (OGTT) and plasma free fatty acids. Second, fasting blood lipids, blood pressure, and concentration of plasminogen activator inhibitor-1 were assessed.
Results
There were no differences between milk, SSSD, NCSD, and water on insulin sensitivity assessed by OGTT (Matsuda Index, fasting, and area under the curve glucose, insulin and homeostasis model assessment values). SSSD increased total cholesterol compared to NCSD (P = 0.007), and triacylglycerol compared to NCSD and water (P = 0.045 and 0.045, respectively). None of the other parameters differed significantly between the groups.
Conclusions
In conclusion, there were no differences in effect between intake of milk, SSSD, NCSD, and water (1 L/d) for 6-month on risk markers of T2D in overweight and obese adults. As a secondary analysis, these results need confirmation in future studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Change history
22 November 2019
Since publication the authors noticed an error in Tables 2, 3, and 4 of the original article, where the pre-intervention values were presented by mean and SD instead of mean and SE as described in the table text. The correct tables are reproduced below where SD’s are replaced by SE’s.
References
WHO. WHO Global report on Diabetes. World Health Organization. 2016. Internet: Available from: http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf (accessed 26 September 2017).
Qin L-Q, Xu J-Y, Han S-F, Zhang Z-L, Zhao Y-Y, Szeto IMY. Dairy consumption and risk of cardiovascular disease: an updated meta-analysis of prospective cohort studies. Asia Pac J Clin Nutr. 2015;24:90–100.
Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93:158–71.
Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr. 2013;98:1066–83.
Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr. 2016;103:1111–24.
Chen M, Sun Q, Giovannucci E, Mozaffarian D, Manson JE, Willett WC, et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med. 2014;12:211–15.
Fonolla J, Lopez-Huertas E, Machado FJ, Molina D, Alvarez I, Marmol E, et al. Milk enriched with ‘healthy fatty acids’ improves cardiovascular risk markers and nutritional status in human volunteers. Nutrition. 2009;25:408–14.
Drouin-Chartier JP, Gagnon J, Labonte ME, Desroches S, Charest A, Grenier G, et al. Impact of milk consumption on cardiometabolic risk in postmenopausal women with abdominal obesity. Nutr J. 2015;14:12.
Soerensen KV, Thorning TK, Astrup A, Kristensen M, Lorenzen JK. Effect of dairy calcium from cheese and milk on fecal fat excretion, blood lipids, and appetite in young men. Am J Clin Nutr. 2014;99:984–91.
Barr SI, McCarron DA, Heaney RP, Dawson-Hughes B, Berga SL, Stern JS, et al. Effects of increased consumption of fluid milk on energy and nutrient intake, body weight, and cardiovascular risk factors in healthy older adults. J Am Diet Assoc. 2000;100:810–17.
Greenwood DC, Threapleton DE, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. Association between sugar-sweetened and artificially sweetened soft drinks and type 2 diabetes: systematic review and dose-response meta-analysis of prospective studies. Br J Nutr. 2014;112:725–34.
Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33:2477–83.
Rogers PJ, Hogenkamp PS, de Graaf C, Higgs S, Lluch A, Ness AR, et al. Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int J Obes. 2016;40:381–94.
Maersk M, Belza A, Stodkilde-Jorgensen H, Ringgaard S, Chabanova E, Thomsen H, et al. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr. 2012;95:283–89.
Bruun JM, Maersk M, Belza A, Astrup A, Richelsen B. Consumption of sucrose-sweetened soft drinks increases plasma levels of uric acid in overweight and obese subjects: a 6-month randomised controlled trial. Eur J Clin Nutr. 2015;69:949–53.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Kaplan W. Background Paper 6.4 Diabetes. Priority Medicines for Europe and the World. ‘A Public Health Approach to Innovation’. World health Organization. 2013. Internet: Available from: http://www.who.int/medicines/areas/priority_medicines/BP6_4DM.pdf(accessed 26 Sseptember 2017).
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–19.
Maki KC, Nieman KM, Schild AL, Kaden VN, Lawless AL, Kelley KM, et al. Sugar-sweetened product consumption alters glucose homeostasis compared with dairy product consumption in men and women at risk of type 2 diabetes mellitus. J Nutr. 2015;145:459–66.
Bergholdt HK, Nordestgaard BG, Ellervik C. Milk intake is not associated with low risk of diabetes or overweight-obesity: a Mendelian randomization study in 97,811 Danish individuals. Am J Clin Nutr. 2015;102:487–96.
Malik VS. Sugar sweetened beverages and cardiometabolic health. Curr Opin Cardiol. 2017;32:572–79. 1
Xi B, Huang Y, Reilly KH, Li S, Zheng R, Barrio-Lopez MT, et al. Sugar-sweetened beverages and risk of hypertension and CVD: a dose-response meta-analysis. Br J Nutr. 2015;113:709–17.
Richelsen B. Sugar-sweetened beverages and cardio-metabolic disease risks. Curr Opin Clin Nutr Metab Care. 2013;16:478–84.
Te Morenga LA, Howatson AJ, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr. 2014;100:65–79.
Benatar JR, Sidhu K, Stewart RAH. Effects of high and low fat dairy food on cardio-metabolic risk factors: a meta-analysis of randomized studies. PLoS ONE. 2013;8:e76480.
Crichton GE, Howe PRC, Buckley JD, Coates AM, Murphy KJ. Dairy consumption and cardiometabolic health: outcomes of a 12-month crossover trial. Nutr Metab. 2012;9:19.
Acknowledgements
We thank Christian Ritz for support with the statistical analyses. We gratefully acknowledge the work of Maria Maersk and Anita Belza, who conducted the intervention and helped planning the study. The authors’ responsibilities were following—S.E.: performed the statistical analysis, wrote the manuscript with primary responsibility for final content; J.M.B.: responsible for the analysis of PAI-1 and FFA; T.T. and A.R.: initiated the current analyses and supplied valuable knowledge and scientific consultation during the process; A.A. and B.R.: took part in the funding and design; all authors: read and approved the final manuscript. A.A. has received research grants from Arla Foods, Denmark; The Danish Dairy Research Foundation; Global Dairy Platform, USA; and the Danish Agriculture and Food Foundation. T.T. has received research grants from Arla Foods, Denmark; The Danish Dairy Research Foundation; and the Dairy Institute, Rosemont, IL. A.R. has received research funding from the Dairy Research Industry, Rosemont, IL, and The Danish Agriculture and Food Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Disclaimer
The sponsors had no influence on the execution of the study, the manuscripts, or its conclusions.
Additional information
No reprints available
The trial is registered at: www.clinicaltrial.gov (NCT00777647)
Rights and permissions
About this article
Cite this article
Engel, S., Tholstrup, T., Bruun, J.M. et al. Effect of high milk and sugar-sweetened and non-caloric soft drink intake on insulin sensitivity after 6 months in overweight and obese adults: a randomized controlled trial. Eur J Clin Nutr 72, 358–366 (2018). https://doi.org/10.1038/s41430-017-0006-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-017-0006-9
This article is cited by
-
WHO guideline on the use of non-sugar sweeteners: a need for reconsideration
European Journal of Clinical Nutrition (2023)
-
Low-fat dairy consumption improves intestinal immune function more than high-fat dairy in a diet-induced swine model of insulin resistance
European Journal of Nutrition (2023)
-
Sugar and low/no-calorie-sweetened beverage consumption and associations with body weight and waist circumference changes in five European cohort studies: the SWEET project
European Journal of Nutrition (2023)
-
The effects of low-calorie sweeteners on energy intake and body weight: a systematic review and meta-analyses of sustained intervention studies
International Journal of Obesity (2021)
-
Association of artificially sweetened and sugar-sweetened soft drinks with β-cell function, insulin sensitivity, and type 2 diabetes: the Maastricht Study
European Journal of Nutrition (2020)