Abstract
The in vitro activity of IMB-XMA0038, a novel inhibitor targeting Mycobacterial tuberculosis (Mtb) aspartate semialdehyde dehydrogenase, was evaluated. Minimum inhibitory concentrations (MICs) of IMB-XMA0038 were against 20 Mtb isolates, including H37Rv (ATCC 27294), ten clinical pan-sensitive isolates, and nine clinical multidrug-resistant (MDR) isolates. In addition, minimum bactericidal concentrations (MBCs) were also determined against the H37Rv and 6 MDR isolates (the background information is same as above in order). A model was generated to evaluate IMB-XMA0038 activity against dormant Mtb. The post-antibiotic effect (PAE), an important indicator of antimicrobial drug dosing schedules to obtain efficacy, was determined based on time required for regrowth of Mtb to 50% of the OD600max value after treatment with various concentrations of IMB-XMA0038 and INH. In addition, interactions between IMB-XMA0038 and other anti-tuberculosis drugs, measured using a checkerboard assay, revealed that IMB-XMA0038 MICs of 0.5–1 μg/mL could be achieved in combinations. Synergistic effects were observed for IMB-XMA0038 when used together with almost all other anti-tuberculosis drugs against most Mtb isolates. IMB-XMA0038 exhibited greater activity than rifampin against Mtb under hypoxic conditions, as reflected by CFU decreases of 1.1-log-unit versus 0.8-log-unit, respectively, for IMB-XMA0038 and rifampin concentrations of 4 × MIC. IMB-XMA0038-induced PAEs (9, 10, 11 days) were comparable to INH PAEs (10, 11, 12 days). These findings suggest that addition of IMB-XMA0038 to current therapeutic regimens could be useful to improve the efficacy of treatments for drug-resistant and drug-susceptible TB.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Singh R, Dwivedi SP, Gaharwar US, Meena R, Rajamani P, Prasad T. Recent updates on drug resistance in Mycobacterium tuberculosis. J Appl Microbiol. 2020;128:1547–67.
Verma SK, Verma R, Verma S, Vaishnav Y, Tiwari SP, Rakesh KP. Anti-tuberculosis activity and its structure-activity relationship (SAR) studies of oxadiazole derivatives: A key review. Eur J Med Chem. 2021;209:112886.
Zuma NH, Smit FJ, Seldon R, Aucamp J, Jordaan A, Warner DF. et al. Single-step synthesis and in vitro anti-mycobacterial activity of novel nitrofurantoin analogues. Bioorg Chem. 2020;96:103587
Suliman S, Pelzer PT, Shaku M, Rozot V, Mendelsohn SC. Meeting report: virtual global forum on tuberculosis vaccines, 20–22 April 2021. Vaccine, 2021;39:7223–9.
Liu Y, Zhou S, Deng Q, Li X, Meng J, Guan Y. et al. Identification of a novel inhibitor of isocitrate lyase as a potent antitubercular agent against both active and non-replicating Mycobacterium tuberculosis. Tuberculosis. 2016;97:38–46.
Bahuguna A, Rawat DS. An overview of new antitubercular drugs, drug candidates, and their targets. Med Res Rev. 2020;40:263–92.
Chavan RR, Hosamani KM. Microwave-assisted synthesis, computational studies and antibacterial/ anti-inflammatory activities of compounds based on coumarin-pyrazole hybrid. R Soc Open Sci. 2018;5:172435.
Usha V, Lloyd AJ, Lovering AL, Besra GS. Structure and function of Mycobacterium tuberculosis meso-diaminopimelic acid (DAP) biosynthetic enzymes. FEMS Microbiol Lett. 2012;330:10–6.
Viola RE, Faehnle CR, Blanco J, Moore RA, Liu X, Arachea BT. et al. The catalytic machinery of a key enzyme in amino Acid biosynthesis. J Amino Acids. 2011;2011:352538
Azevedo RA, Lancien M, Lea PJ. The aspartic acid metabolic pathway, an exciting and essential pathway in plants. Amino Acids. 2006;30:143–62.
Cirillo JD, Weisbrod TR, Pascopella L, Bloom BR, Jacobs WR Jr. Isolation and characterization of the aspartokinase and aspartate semialdehyde dehydrogenase operon from mycobacteria. Mol Microbiol. 1994;11:629–39.
Vyas R, Tewari R, Weiss MS, Karthikeyan S. Structures of ternary complexes of aspartate-semialdehyde dehydrogenase (Rv3708c) from Mycobacterium tuberculosis H37Rv. Acta Crystallogr D Biol Crystallogr. 2012;68:671–9.
Kumar R, Garg P, Bharatam PV. Pharmacoinformatics analysis to identify inhibitors of Mtb-ASADH. J Biomol Struct Dyn. 2016;34:1–14.
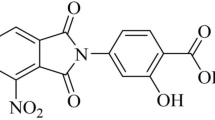
Wang X, Yang R, Liu S, Guan Y, Xiao C, Li C. et al. IMB-XMA0038, a new inhibitor targeting aspartate-semialdehyde dehydrogenase of Mycobacterium tuberculosis. Emerg Microbes Infect. 2021;10:2291–9.
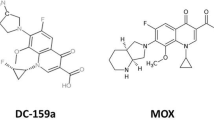
Leechawengwongs M, Prammananan T, Jaitrong S, Billamas P, Makhao N, Thamnongdee N, et al. In vitro activity and MIC of sitafloxacin against multidrug-resistant and extensively drug-resistant mycobacterium tuberculosis isolated in Thailand. Antimicrob Agents Chemother. 2018;62:e00825–17.
Martini MC, Zhang T, Williams JT, Abramovitch RB, Weathers PJ, Shell SS. Artemisia annua and Artemisia afra extracts exhibit strong bactericidal activity against Mycobacterium tuberculosis. J Ethnopharmacol. 2020;262:113191.
Sun Q, Wang S, Liao X, Jiang G, Huang H, Li H, et al. Fidaxomicin has high in vitro activity against Mycobacterium tuberculosis. J Med Microbiol. 2021;70:001324.
Coban AY, Akbal AU, Uzun M, Cayci YT, Birinci A, Durupinar B. Evaluation of crystal violet decolorization assay for minimal inhibitory concentration detection of primary antituberculosis drugs against Mycobacterium tuberculosis isolates. Mem Inst Oswaldo Cruz. 2016;111:454–9.
Hussain A, Rather MA, Bhat ZS, Majeed A, Maqbool M, Shah AM. et al. In vitro evaluation of dinactin, a potent microbial metabolite against Mycobacterium tuberculosis. Int J Antimicrob Agents. 2019;53:49–53.
Jadaun GP, Agarwal C, Sharma H, Ahmed Z, Upadhyay P, Faujdar J. et al. Determination of ethambutol MICs for Mycobacterium tuberculosis and Mycobacterium avium isolates by resazurin microtitre assay. J Antimicrob Chemother. 2007;60:152–5.
Joung DK, Choi SH, Kang OH, Kim SB, Mun SH, Seo YS. et al. Synergistic effects of oxyresveratrol in conjunction with antibiotics against methicillin-resistant Staphylococcus aureus. Mol Med Rep. 2015;12:663–7.
Santos NCS, Scodro RBL, Leal DC, do Prado SM, Micheletti DF, Sampiron EG. et al. Determination of minimum bactericidal concentration, in single or combination drugs, against Mycobacterium tuberculosis. Future Microbiol. 2020;15:107–14.
Betts JC, Lukey PT, Robb LC, McAdam RA, Duncan K. Evaluation of a nutrient starvation model of Mycobacterium tuberculosis persistence by gene and protein expression profiling. Mol Microbiol. 2002;43:717–31.
Wayne LG, Hayes LG. An in vitro model for sequential study of shiftdown of Mycobacterium tuberculosis through two stages of nonreplicating persistence. Infect Immun. 1996;64:2062–9.
Hurdle JG, Lee RB, Budha NR, Carson EI, Qi J, Scherman MS. et al. A microbiological assessment of novel nitrofuranylamides as anti-tuberculosis agents. J Antimicrob Chemother. 2008;62:1037–45.
Zhang M, Sala C, Hartkoorn RC, Dhar N, Mendoza-Losana A, Cole ST. Streptomycin-starved Mycobacterium tuberculosis 18b, a drug discovery tool for latent tuberculosis. Antimicrob Agents Chemother. 2012;56:5782–9.
Birteksoz-Tan AS, Zeybek Z. Postantibiotic effect of various antibiotics on Legionella pneumophila strains isolated from water systems. Folia Microbiol. 2012;57:495–9.
Hasenoehrl EJ, Rae Sajorda D, Berney-Meyer L, Johnson S, Tufariello JM, Fuhrer T. et al. Derailing the aspartate pathway of Mycobacterium tuberculosis to eradicate persistent infection. Nat Commun. 2019;10:4215
Cox H, Shah NS, Castro KG. Discovering a new drug is only the beginning: progress and challenges in expanding access to BDQ for MDR-TB treatment. Int J Tuberc Lung Dis. 2020;24:985–6.
Tato M, López Y, Morosini MI, Moreno-Bofarull A, Garcia-Alonso F, Gargallo-Viola D. et al. Characterization of variables that may influence ozenoxacin in susceptibility testing, including MIC and MBC values. Diagn Microbiol Infect Dis. 2014;78:263–7.
Cele ZED, Somboro AM, Amoako DG, Ndlandla LF, Balogun MO. Fluorinated quaternary chitosan derivatives: synthesis, characterization, antibacterial activity, and killing kinetics. ACS Omega. 2020;5:29657–66.
Peterson EJR, Abidi AA, Arrieta-Ortiz ML, Aguilar B, Yurkovich JT, Kaur A. et al. Intricate genetic programs controlling dormancy in mycobacterium tuberculosis. Cell Rep. 2020;31:107577
Fogel N. Tuberculosis: a disease without boundaries. Tuberculosis. 2015;95:527–31.
Esmail H, Barry CE 3rd, Wilkinson RJ. Understanding latent tuberculosis: the key to improved diagnostic and novel treatment strategies. Drug Disco Today. 2012;17:514–21.
Ai JW, Ruan QL, Liu QH, Zhang WH. Updates on the risk factors for latent tuberculosis reactivation and their managements. Emerg Microbes Infect. 2016;5:e10.
Khan MT, Kaushik AC, Bhatti AI, Zhang YJ, Zhang S, Wei AJ, et al. Marine natural products and drug resistance in latent tuberculosis. Mar Drugs. 2019;17:549.
Banerjee U, Sankar S, Singh A, Chandra N. A multi-pronged computational pipeline for prioritizing drug target strategies for latent tuberculosis. Front Chem. 2020;8:593497.
Doğan ŞD, Gündüz MG, Doğan H, Krishna VS, Lherbet C, Sriram D. Design and synthesis of thiourea-based derivatives as Mycobacterium tuberculosis growth and enoyl acyl carrier protein reductase (InhA) inhibitors. Eur J Med Chem. 2020;199:112402.
Chandramohan Y, Padmanaban V, Bethunaickan R, Tripathy S, Swaminathan S, Ranganathan UD. In vitro interaction profiles of the new antitubercular drugs bedaquiline and delamanid with moxifloxacin against clinical Mycobacterium tuberculosis isolates. J Glob Antimicrob Resist. 2019;19:348–53.
Acknowledgements
We thank the study coordinators and staff at the hospital for their contributions to this research. This study was supported by Natural Sciences Foundation of China (NSFC, Grant No. 81803412), and the Beijing Key Clinical Specialty Project.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yang, R., Cao, W., Liu, S. et al. Evaluation of a novel inhibitor of aspartate semialdehyde dehydrogenase as a potent antitubercular agent against Mycobacterium tuberculosis. J Antibiot 75, 333–340 (2022). https://doi.org/10.1038/s41429-022-00520-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-022-00520-y