Abstract
Vulvovaginal candidiasis (VVC) affects millions of women around the world every year. Candida albicans is the most frequently isolated pathogen in women and its rapid ability to develop resistance to first and second line therapies has boosted the search for new and effective antifungal agents. In this study, we show the in vitro anti-Candida activity of fifteen synthetic chalcone analogs and their antifungal potential in an in vivo model of VVC. Chalcone 12 showed potent antifungal effects, being able to inhibit the growth of Candida spp. at a concentration of 15.6 µg mL−1. In addition, mechanism of action studies have indicated the ergosterol fungal membrane as the target of this compound. Despite a considerable antifungal activity, the chalcone 12 showed high cytotoxicity in kidney cells lineages. Moreover, this compound was able to reduce Candida-associated virulence, impairing yeast–hyphal transition in C. albicans. An in vivo model of VVC showed that chalcone 12 significantly reduces the fungal load. Taken together, these findings showed that the chalcone 12 is a potent anti-Candida agent in vitro beyond of contribute to improve the fungal infection in a model of CVV. However, it showed low selectivity and high toxicity, suggesting molecular modifications to minimize these proprieties.
Similar content being viewed by others
Introduction
Vulvovaginal Candidiasis (VVC) stands out among the main causes of gynecological disorders worldwide [1]. This infection is a significant problem, affecting 75% of all women at least once during their lifetime [2]. In the USA, almost 10 million women visit physicians for the treatment of vaginitis annually [3, 4]. Although most episodes of symptomatic disease appear as sporadic attacks of acute VVC, some women have chronic manifestations, and various patients have shown frequent infections with manifestations ranging from four or more episodes for year, characterizing a board of VVC recurrent (VVCR) [5].
Candida albicans is the major etiological agent in VVC and VVCR. However, studies have shown an increase in the prevalence of non-albicans Candida which featured the species C. glabrata, C. tropicalis, C. krusei, and C. dubliniensis [6]. Additionally, there are many problems related to the currently available drugs and resistance to azoles and echinocandins has been shown with frequency in C. albicans and non-albicans [7]. In disparity to the steep rise in number of VVC cases for this species, only a few drugs have been developed over the past 5–6 decades [8].
In this context, chalcones have been highlighted as an important class in the search for new antifungal agents. Chemically known as 1,3-diaryl-2-propen-1-ones, the chalcones consist of open-chain flavonoids in which the two aromatic rings are joined by a three-carbon with an α,β-unsaturated carbonyl system [9]. Naturally occurring chalcones and their synthetic analogs display a wide spectrum of pharmacological activities, such as antibacterial [10] and antileishmanial, [11], and some studies have described the antifungal potential of this class [12,13,14,15]. However, limited information is available regarding the antifungal action of chalcones, and potential applications in in vivo infections model, especially regarding candidiasis. Thus, the aims of this paper were to evaluate the anti-Candida spectrum, the mechanism of action, the effect on virulence factor (yeast–hyphal transition) and the cytotoxicity in renal cells lineages, of fifteen synthetic chalcones. Additionally, we aimed to evaluate the potential utilization of the most active chalcone in the treatment of VVC.
Materials and methods
Synthesis and purification of chalcones
Reagents and solvents were purchased as reagent grade and used without further purification. ¹H and ¹³C Nuclear magnetic resonance (NMR) spectra for all chalcones were acquired in a Bruker AVANCE DRX-400 or Bruker Avance-600. Chemical shifts were reported as δ (ppm) downfield from tetramethylsilane (TMS) and the J values were reported in Hz. Spectra were recorded in chloroform-d (CDCl3) or dimethylsulfoxide-d6 (DMSO-d6) solutions. Mass spectra (MS) were recorded on a Bruker Daltonics Amazon SL (Supplementary material). Preparative chromatography was performed using silica gel (230–400 mesh) as described [16]. Thin layer chromatography (TLC) was performed using silica gel GF254, with a thickness of 0.25 mm. TLC plates were visualized under ultraviolet light or stained with iodine vapor or acidic vanillin. All procedures and spectral data are presented.
Fifteen synthetic chalcones with different structural modifications were synthesized, characterized and denominated from 1 to 15. Bromide C was obtained from compound A by a previously described O-alkylation method [17]. Compound D was synthesized by N-alkylation of compound C with morpholine in the presence of triethylamine and N, N-Dimethylformamide (DMF) at room temperature for 3 h. Desired morpholinochalcone 15 was synthesized by Claisen–Schmidt condensation of compound D with benzaldehyde.
Chemo-informatic study
To calculate the physicochemical (LogP, LogS, Molecular Weight, Numbers of acceptor and donors groups of hydrogen bond) and pharmaceutical (Druglikeness) properties of compounds, chemo-informatics analyses were employed. The two-dimensional chemical structures of the chalcones were inserted into DataWarrior 4.2.2 software and the parameters of interest were calculated [18]. After, values of molecular weight, LogP, and number of donor and acceptor groups of hydrogen bonds were compared with the Lipinsk rules [19]. The descriptor 'respect all' was added to the compounds that fit at all points. However, if any were violated, the descriptor 'not respect all' was employed followed by the description of the rule in non-compliance.
Cell culture and cytotoxicity assay
Cytotoxicity of active chalcones was evaluated using the African green monkey kidney epithelium (Vero, ATCC CCL-81) and Baby Hamster Kidney (BHK-21, ATCC CCL-10) cells. These were cultured in Dulbecco’s Modified Eagle supplemented with 10% fetal bovine serum (FBS) and 0.3% of solution content penicillin, streptomycin, and amphotericin B. Cell cultures were maintained at 35 ± 2 °C in a humidified atmosphere of 5% CO2. Cells lines were exposed to the compounds for 48 h and the cell viability was posteriorly quantified by the 3-(4.5-dimethylthiazol-2-yl)-2.5-diphenyltetrazolium bromide (MTT) colorimetric assay. Finally, the cytotoxic concentrations for 50% of the cells (CC50) were calculated by linear regression analysis. [20]
Antifungal activity
Fungal strains
Four fungal strains obtained from the American Type Culture Collection (ATCC) were used: C. albicans ATCC 10231, C. glabrata ATCC 2001, C. krusei ATCC 34135, and C. tropicalis ATCC 28707. In addition, eight clinical isolates were provided by Marivalda A. R. Oliveira (Laboratory, Biocentro Ltda, Divinopolis, Brazil) including three strains of C. albicans and five of C. dubliniensis. According to ATCC specifications, C. albicans ATCC 10231 is resistant to anidulafungin, voriconazole, itraconazole, fluconazole, and Ketoconazole. Moreover, C. glabrata ATCC 2001 showed high value of MIC to azole antifungals [21].
Determination of minimum inhibitory concentrations (MIC) and minimum fungicidal concentrations (MFC)
Minimum inhibitory concentration (MIC) was determined by the microdilution method according to document M27-A3 of the Clinical and Laboratory Standards Institute [22], with minor modifications [23]. The fifteen chalcones, named from 1 to 15, were tested by employing concentrations ranging from 3.9–1000 μg mL−1. Ketoconazole and Nystatin were included as positive controls, and DMSO 2% v/v was used as the solvent control. The minimal fungicidal concentration (MFC), in turn, was determined as the absence of visible colonies in Sabourad-Dextrose agar (SDA), as previously described [24]. All tests were performed in triplicate from at least three independent experiments.
Mechanism of action studies
The probable mechanism of action was determined for the highest activity chalcone using ergosterol exogenous binding and cytoprotection with sorbitol assays. The MIC of compounds was determined as described above in the absence and presence of ergosterol (200 μg mL−1) or sorbitol (0.8 M) [25]. Any increase in MIC after ergosterol addition was considered to indicate that the compound interferes with the fungal membrane. In the case of an increase with the supplementation of sorbitol, the compound was considered to be due to changes in the cell wall [25]. Nystatin and Caspofungin were used as positive controls in ergosterol and sorbitol assays, respectively.
Time-kill curve
The kinetics of anti-Candida activity was studied for the most active chalcone, as previously described [26]. In brief, tubes with 10 mL Sabouraud-Dextrose broth containing C. albicans ATCC 10231 (106 CFU mL−1) and different concentrations of the most active chalcone were incubated at 35 ± 2 °C. Then, 0.1 mL from these tubes were taken at different time intervals (0, 2, 4, 6, 8, 10, 12, 24, 36, and 48 h) and inoculated on SDA plates. After, the plates were incubated at 35 ± 2 °C for 48 h for posterior colonies count, with the results expressed in CFU mL−1. Ketoconazole and DMSO (2% v/v) were included as positive and solvent controls, respectively.
Inhibition of yeast-hyphae transition
The most active chalcone was studied regarding its ability to inhibit yeast-hyphae transition in C. albicans ATCC 10231. Hyphal induction was conducted by the incubation of C. albicans ATCC 10231 (103 CFU mL−1) in microplate content FBS plus different concentrations of chalcone. The microplates were incubated for 24, 48, and 72 h at 35 ± 2 °C and the hyphal formation in C. albicans was observed through a light microscope (Nikon TE 2000-U Eclipse) with a magnification of ×400. Positive (ketoconazole) and solvent (DMSO 2% v/v) controls were included [27].
Therapeutic effect in a VVC animal model
Preparation of vaginal cream
An oil/water emulsion was obtained according to Bancroft's Rule, which contained (w/w) 5.0% nonionic emulsifying wax (PolawaxTM), 3.0% mineral oil, 0.05% butylated hydroxytoluene, 5.0% glycerol, 0.1% disodium ethylenediamine tetraacetic acid (EDTA), 2.0% propylene glycol, 0.2% parabens, and water q.s.p. 100% [28]. The vaginal cream was prepared for the addition of 0.1, 0.5, and 1.0% (w/w) of the most activity chalcone dispersed in isopropyl myristate. Citric acid was added to the emulsion to a final pH of 4.0–4.5 [29].
VVC Model
Female Wistar rats (100–150 g) were maintained in accordance with the institutional guidelines. The protocol was approved by the Animal Experimentation Ethics Committee of the Universidade Federal de São João Del-Rei (Protocol 002/2015). To establish a pseudo-estro state, the subcutaneous administration of estradiol cypionate (Pfizer, Brazil) at the dose of 0.2 mg mL−1 was performed for 24/24 h over 5 days before infection and for 48/48 h from of day 7. Rats were immunosuppressed by the administration of cyclophosphamide (Sigma-Aldrich, Brazil, 50 mg kg-1 b.w.). On the first day, 0.1 mL of a viable suspension of C. albicans ATCC 10231 (5.0 × 107 CFU mL−1) was inoculated into the rat vaginal cavity. Two days after infection (day 0) the vaginal fungal load was evaluated through lavage with 0.1 mL of saline, and determined in culture of SDA supplemented with 0.05% chloramphenicol, with the results expressed as CFU mL−1. The infection was considered sufficient if a count for the vaginal lavage cultures from each rat was 102 CFU mL−1 [30].
Treatment of animals
Wistar females were randomized into seven equal groups (n = 6 in each): non-infected (1); infected and untreated (2); infected and treated with clotrimazole 1% cream vaginal (Medley, Brazil) (3); infected and treated with vaginal cream containing the most active chalcone at doses of 0.1% (4), 0.5% (5), and 1% (6); and infected and treated with base vaginal cream (7). Treatments were administered intravaginally once per day for 6 consecutive days. On days 0, 2, 4, and 6 after infection, the vaginal fungal load was evaluated to verify the effectiveness of the treatments [31].
Statistical analysis
All in vitro tests were performed in triplicate with at least three independent experiments. For in vivo studies, the normality was evaluated by Shapiro–Wilk test. An one-way analysis of variance (ANOVA) was used to demonstrate the differences between the groups. The Tukey test was used to compare the results of the treatments and the Dunnett test to compare the results of the treatment and control [32]. A p-value less than 0.05 was considered statistically significant.
Results
Synthesis of chalcones
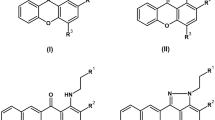
As shown in Fig. 1, the treatment of resacetophenone (A) with 3,4-Dihydro-2H-pyran (DHP) in dichloromethane and catalytic amount of pyridinium-p-toluene sulfonate (PPTS) gave the corresponding compound B. Tetrahydropyranyl chalcones (1–7) were synthesized from compound B by Claisen–Schmidt condensation with different aromatic aldehydes. Dihydroxychalcones (8–14) were obtained by the treatment of tetrahydropyranyl chalcones in ethanolic acid media after 4 h at room temperature. Morpholinochalcone (15) was synthesized from compound C, that was prepared by selective O-alkylation of resacetophenone with 1,4-dibromobutane. Then, compound D was prepared by the nucleophilic substitution reaction of compound C with morpholine in DMF. Morpholinochalcone (15) was obtained by Claisen–Schmidt condensation with benzaldehyde, similarly to tetrahydropyranyl chalcones. The fifteen novel chalcones were synthesized with yields ranging between 70 and 86% (Fig. 1). All the compounds and their intermediates were successfully characterized by ¹H and ¹³C NMR and ESI-MS (Supplementary material).
General route to the synthesis of chalcones 1–15. Reagents and conditions: (i) PPTS, dichloromethane, DHP, r.t., 24 h; (ii) Aromatics benzaldehyde, methanol, KOH, r.t., 24 h; (iii) Ethanol, HCl (4 mol L−1), r.t., 4 h; (iv) 1,4-dibromobutane, K2CO3, acetonitrile, 45 °C, 5 h; (v) Morpholine, DMF, triethylamine, r.t.,3 h; (vi) Benzaldehyde, methanol, KOH, r.t., 24 h
Fungistatic and fungicidal activity of chalcones
Chalcone 12 presents the best value of MIC and MFC (15.6 μg mL−1) against C. albicans. This activity pattern was also observed against C. glabrata (MIC 15.6 μg mL−1 and MFC 125 μg mL−1), C. krusei (MIC and MFC 15.6 μg mL−1), and C. tropicalis (MIC 15.6 μg mL−1 and MFC 31.25 μg mL−1) (Table 1). In addition, chalcone 12 retained the antifungal activity against clinical specimens obtained from vaginal secretion. Three different clinical isolates of C. albicans (MIC 31.25 μg mL−1), as well as five isolates of non-albicans Candida (C. dubliniensis, MIC 31.25 μg mL−1) were susceptible to chalcone 12. For the specimen of C. albicans called CVV1, for example, the effect was observed to the same level as ketoconazole (Table 2). Compound 15 was moderately active against C. krusei and C. tropicalis (MIC 31.25 μg mL−1) (Table 1). The MIC and MFC results for chalcones 1–7 were described in Tables S1 and S2 in the supplementary material section.
Cytotoxicity assay
The two active chalcones (12 and 15), showed cytotoxicity in vitro against cells renal lineages. We found that the CC50 of chalcone 12 for BHK-21 and Vero cells was 8.67 ± 4.16 μg mL−1 and 2.10 ± 0.69 μg mL−1, respectively. In addition, the CC50 of chalcone 15 showed values of 2.79 ± 0.540 μg mL−1 for BHK-21 and 5.21 ± 0.0 μg mL−1 for Vero cells. Ketoconazole was also considerably cytotoxic, showing a CC50 of 42.48 ± 1.16 μg mL−1 and 10.31 ± 0.60 μg mL−1 for Vero and BHK-21 cells, respectively.
Structure-activity relationship (SAR) and chemo-informatics analysis
The SAR studies showed that a lower biological activity is associated with the presence of substituents in benzene ring of dihydroxychalcones (8–14) (Fig. 2). In fact, the substitution with the OMe (8), OEt (9), OBu (10), OHex (11), or Cl (13 and 14) groups into aromatic core decrease the antifungal activity in these analogs. Furthermore, only the unsubstituted chalcone (12) showed a potent antifungal effect. Already the unsatisfactory activity of hydroxychalcones (1–7) can be justified by substitution of the hydroxyl group by oxa-hexane (Fig. 2), which involves to loss of one hydrogen bonding donor centers in relation the dihydroxychalcones (Table 3). Chalcone 15, in turn, exhibits a species-specific behavior, possessing a moderate fungistatic effect against C. krusei and C. tropicalis, but shows low activity against C. albicans, C. glabrata, and C. dubliniensis. This effect is associated with the presence of morpholine group, which is a pharmacophore exclusive this compound.
Chemo-informatics analysis (Table 3) showed that chalcone 12, which has fungistatic/fungicidal effect, presented physicochemical characteristics in accordance with all of the Lipinski's rules (MW: 240.26 g mol−1; cLogP: 2.61; H-donors: 2; H-acceptors: 3), predicting good oral bioavailability. Druglikeness, which suggests a significant pharmaceutical potential when greater than 0, was mostly unsatisfactory, ranging from −14.99 to 0.22. Chalcone 12 presented a considerable druglikeness (0.13); however, it was considerable inferior to ketoconazole (8.14). Furthermore, all of the evaluated compounds (including the ketoconazole) were predicted for reduced water solubility, because cLogS ranged from −5.93 to −2.99.
Mechanism of action of chalcone 12
To determine the target of action antifungal of chalcone 12, the potential of this compound to bind to the ergosterol membrane or to fungal cell walls was investigated (Table 4). Chalcone 12 showed a two-fold increase of MIC in the presence of exogenous ergosterol for C. albicans and C. krusei (the test was performed in three independent experiments using the same conditions). Thus, in these species, it is suggest that the action of the compound involve the bind with the sterol fungal. The MICs of nystatin were increased in the presence of ergosterol, validating the experimental conditions of this study.
In tests, after the addition of sorbitol, MICs remained unchanged for all four species evaluated against chalcone 12, suggesting that this compound does not interfere with the fungal cell wall. Caspofungin, as expected, showed an increase in the MICs after sorbitol supplementation.
Time-kill curve study
The kill kinetics assay showed that after 4 h of exposure to chalcone 12, a reduction of one log at the concentration of 2-fold MIC and two logs at the concentration of the MIC was observed against C. albicans. Posteriorly, chalcone 12 showed a maximum fungicidal effect at 2-fold MIC and at MIC with 6 and 10 h of incubation, respectively (Fig. 3). Ketoconazole did not show a fungicidal effect, presenting the same density of fungal cells during the entire period of time considered in this experiment (48 h).
Time-Kill curve test to chalcone 12 against Candida albicans ATCC 10231. The compound was tested at concentrations of 1 × MIC (15.6 µg mL−1) (●) and 2 × MIC (31.25 µg mL−1) (■). Ketoconazole was employed as positive control in concentration of 1 × MIC (125 µg mL−1) (▲) and fungal cells untreated as growth control (▼)
Inhibition of yeast-hyphae transition
The chalcone 12 was able to reduce yeast-hyphae transition at all concentrations tested (7.8, 15.6, and 31.25 μg mL−1) in relation to untreated cells. This effect can be observed in first 24 h of incubation, been remained for up to 72 h (Fig. 4).
Hyphal formation of Candida albicans ATCC 10231. Candida albicans were cultured with different concentration of chalcone 12 (7.8, 15.6, and 31.25 µg mL−1) during 24, 48, and 72 h at 37 °C. Ketoconzole was used as a positive control. The experiments were performed in duplicate and repeated three times. Representative microphotographs are showed. The white bar represents a length of 50 μm (magnification of ×400)
Therapeutic effect of chalcone 12 in a VVC animal model
Pharmaceutical preparations containing chalcone 12 were employed to treat VVC in rats. Table 5 showed that in relation to the infected group, the animals treated with cream containing 0.5 and 1.0% of chalcone 12 showed a significant reduction in fungal load (p < 0.05) after 6 days. However, no interaction existed between the tested doses (0.1, 0.5, and 1.0%) and the time evaluated (days 0, 2, 4, and 6) (p > 0.05). On the last day, for example, all doses of chalcone 12 showed a cure rate of 60%. Clotrimazole, in turn, showed a complete remission of the infection in all animals on day 4, being statistically different from untreated and chalcone-treated groups (p < 0.05).
Discussion
In this study, we showed that chalcone 12 has considerable antifungal activity in vitro and in vivo. The fungistatic effect was equipotent to C. albicans, C. glabrata, C. krusei, and C. tropicalis, revealing an extend-spectrum that covers the most frequent species involved in candidiasis. Furthermore, the compound 15 showed promising antifungal activity in vitro against C. krusei and C. tropicalis. In contrast to the others compounds employed, this chalcone was synthetized by the insertion of the morpholine group, which was recently described as an important pharmacophore in molecules with antifungal activity [33]. Similar to these results, Kant and collaborators [14] showed the potential antifungal activity of 25 chalcones against Candida spp., revealing MICs in the range of 6.25–50 µg mL−1. Candida albicans was particularly sensitive to compounds of the chalcone class, showing MICs that ranged from 1 to 64 µg mL−1 [34]. Thus, the results presented here corroborate those of previous works that point to chalcones as a promising class in the development of prototypes targeted to antifungal therapy.
Chalcone 12 presented fungicidal action against all Candida species evaluated. Fungicidal activity is of paramount importance; because substances able to kill pathogens are strong candidates for clinical use [35]. The time-kill curve study revealed that the fungicidal activity of this compound was rapid, with a maximum effect after 6 h at 2-fold MIC and 10 h at MIC. Thus, an efficient fungicidal effect is attributed to chalcone 12, which is pharmacologically important because the rapid elimination of microorganisms guarantees therapeutic success to prevent the spread of pathogens and the progression of disease to boards of greater severity [36, 37].
One of the proposed mechanisms of actions for antifungal agents is binding to membrane ergosterol, which leads to fungal cell disruption and a loss of intracellular content [38]. The exogenous ergosterol binding assay suggests that chalcone 12 targets this sterol of the fungal membrane. Corroborating with this result, the cell membrane disrupting nature of Candida spp. by compounds of the chalcones class was confirmed in other study, which showed that these compounds increase the intracellular levels of propidium iodide, a fluorescent intercalating agent that only penetrates cells with damaged membranes [39]. However, in this study, the effect on membrane ergosterol was species-specific, as the compound was able to bind to ergosterol only in C. albicans and C. krusei. These behaviors appoint that the binding of chalcone 12 to ergosterol is not single action mechanism. In fact, chalcones are also believed to inhibit the synthesis of 1,3-β-D-glucan [40], but the action of chalcone 12 on this and others fungal cells component remain to be determined in future studies.
Although chalcone 12 acts on targets conserved exclusively in fungal cells (ergosterol), the cytotoxicity of this compound was high against mammalian eukaryotic cells. CC50 was considerably lower in Vero (CC50 2.10 ± 0.69 μg mL−1) and BHK-21 (CC50 8.67 ± 4.16 μg mL–1) cells, which was also observed in other studies that employed chalcones as antimicrobial agents [41]. In contrast to the several pharmacological proprieties attributed to chalcones derivatives, it was also discovered that many of them have a strong cytotoxic potential and might cause severe adverse effects [42]. Synthetic and natural chalcones are known by their myotoxicity, generally associated with the breakage and collapse of myofibrils, reduction of cell numbers, and disorganization of thick (myosin) and thin (actin) filaments [43], as well as by their mitotoxicity, related with the ability of chalcones in inhibit tubulin assembly and actuate on other components of cell cycle [42]. Thus, chalcones derivatives showed high toxicity on eukaryotic cells. Hence, as both, fungal, and mammalian cells are eukaryotic, is not a surprise that this compounds shown a no selective toxicity [35, 44]. In other study, conducted by Zenger et al. (2015) showed that cytotoxic effects are correlated with the presence and positions of the hydroxyl groups on the chalcone scaffold [42]. In addition, the chemical characteristic of α,β-double bond (Michael-system) is also a crucial element for toxicity of chalcones derivatives [45]. Hence, it has been shown that Michael-system is involved in the inhibition of cell proliferation, reduction of mitochondrial mass, and cytochrome c release from mammalian cells [42].
Candida albicans show several virulence factors such as significant thermotolerance, dimorphism with production of filamentous structures that aid tissue invasion, enzymatic production, and the ability to form biofilms [32]. In this study, we evaluated the ability of chalcone 12 to inhibit yeast–hyphal transition, which is the main virulence factor in this species. In relation to untreated cells, chalcone 12 showed a considerable reduction in filamentous structures of C. albicans, with this effect occurring in a dose-dependent manner (Fig. 3). Similarly to these results, Messier and collaborators [46] revealed that chalcones were able to inhibit yeast-hyphae transition when tested at concentrations between 50−200 μg mL−1, sustaining the potential anti-hyphae activity of this compound class.
Lastly, to clarify the anti-Candida potential of chalcone 12, we opted to evaluate the pharmacologic effect of this compound in a model of VVC in rats [32]. Previous reports showed that immunosuppressed rats in a prolonged pseudo-estrus state are particularly susceptive to fungal colonization in vaginal mucosa [27, 32]. After intravaginal instillation of a C. albicans suspension (5 × 107 CFU mL−1) in immunosuppressive rats in the pseudo-estrus state, we observed maintained infection in all animals, with a fungal load greater than 102 CFU mL−1. In these animals, after 6 days of treatment with the cream containing the chalcone 12 at 0.5% and 1.0%, the fungal burden was reduced significantly compared to the infected and untreated group (p < 0.05). These results showed for the first time the potential of chalcones in the treatment of CVV.
In summary, chalcone 12 showed potent antifungal effects, being able to completely eliminate the yeast C. albicans after six hours of exposure at a concentration of 31.25 µg mL−1. In addition, this chalcone inhibited the yeast–hyphal transition of C. albicans, which is an important virulence factor associated with tissue invasion in this pathogen. Chalcone 12 possibly acts as an antifungal with a target for membrane ergosterol, but more studies should be considered for analyses other action mechanism involved, such as inhibition in the synthesis of 1,3-β-D-glucan. Finally, we also provide robust evidence about the in vivo effects of chalcone 12 in the treatment of VVC. However, molecular modifications of this compound should be encouraged, with the aim of reducing toxicity and potentiating the antifungal effect.
References
Olowe OA, Makanjuola OB, Olowe R, Adekanle DA. Prevalence of vulvovaginal candidiasis, trichomoniasis and bacterial vaginosis among pregnant women receiving antenatal care in southwestern Nigeria. Eur J Microbiol Immunol. 2014;4:193–7.
Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961–71.
Ventolini G, Baggish MS. Recurrent vulvovaginal candidiasis. Clin Microbiol Newsl. 2006;28:15–21.
Ahmad A, Khan AU. Prevalence of Candida species and potential risk factors for vulvovaginal candidiasis in Aligarh, India. Eur J Obstet Gyn Reprod Biol. 2009;144:68–71.
Pappas PG, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of america. Clin Infect Dis. 2016;62:1–50.
Silva S, et al. Candida glabrata, Candida parapsilosis and Candida tropicalis: biology, epidemiology, pathogenicity and antifungal resistance. Fems Microbiol Rev. 2012;36:288–305.
Cleveland AA, et al. Changes in incidence and antifungal drug resistance in candidemia: results from population-based laboratory surveillance in Atlanta and Baltimore, 2008–2011. Clin Infect Dis. 2012;55:1352–61.
Maurya IK, et al. Mechanism of action of novel synthetic dodecapeptides against Candida albicans. Biochim Biophys Acta. 2013;1830:5193–203.
Sahu NK, Balbhadra SS, Choudhary J, Kohli DV. Exploring pharmacological significance of chalcone scaffold: a review current. Med Chem. 2012;19:209–25.
Hu Y, Keniry M, Palmer SO, Bullarda JM. Discovery and analysis of natural-product compounds inhibiting protein synthesis in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2016;60:4820–9.
Passalacqua TG, et al. 2′,4′-dihydroxychalcone could be explored to develop new inhibitors against the glycerol-3-phosphate dehydrogenase from Leishmania species. Bioorg Med Chem Lett. 2015;17:3564–8.
Batovska D, et al. Study on the substituents’ effects of a series of synthetic chalcones against the yeast Candida albicans. Eur J Med Chem. 2007;42:87–92.
Konduru NK, Dey S, Sajid M, Owais M, Ahmed N. Synthesis and antibacterial and antifungal evaluation of some chalcone based sulfones and bisulfones. Eur J Med Chem. 2013;59:23–30.
Kant R, et al. Synthesis of newer 1,2,3-Triazole linked chalcone and flavone hybrid compounds and evaluation of their antimicrobial and cytotoxic activities. Eur J Med Chem. 2016;113:34–49.
Yadav M, Lavania A, Dasaray K, Anand AVK. Synthesis of chalcone and their derivatives as antimicrobial agents by using Poly Ethylene Glycol PEG(400). J Appl Chem. 2016;5:136–41.
Still WC, Kahn M, Mitra A. Rapid chromatographic technique for preparative separations with moderate resolution. J Org Chem. 1978;43:2923–25.
Evangelista FCG, et al. Synthesis and in vitro evaluation of novel triazole/azide chalcones. Med Chem Res. 2016;26:27–43.
Sander T, Freyss J, Von KM, Rufener C. DataWarrior: an open-source program for chemistry aware data visualization and analysis. J Chem Inf Model. 2015;55:460–73.
Leeson P. Drug discovery: chemical beauty contest. Nature. 2012;481:455–6.
Souza MA, et al. The antimicrobial activity of lapachol and its thiosemicarbazone and semicarbazone derivatives. Mem Inst Oswaldo Cruz. 2013;108:342–51.
Lima WG, et al. Absence of antibacterial, anti-Candida, and anti-dengue activities of a surfactin isolated from Bacillus subtilis. J Pharm Negat Results. 2017;8:1–6.
CLSI. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard. 3rd edn. Wayne, PA: Clinical and Laboratory Standards Institute; 2008. CLSI document M27-A3
Allochio Filho JF, et al. Synthesis, in vitro antifungal activity and molecular modeling studies of new mannich bases derived from lawsone. J Braz Chem Soc. 2016;27:2127–40.
Guo Z, et al. Synthesis, characterization, and antifungal activity of novel inulin derivatives with chlorinated benzene. Carbohydr Polym. 2014;99:469–73.
Escalante A, Gattuso M, Perez P, Zacchino S. Evidence for the mechanism of action of the antifungal Phytolaccoside B isolated from Phytolaccatetramera Hauman. J Nat Prod. 2008;71:1720–5.
Zore GB, Thakre AD, Jadhav J, Karuppayil SM. Terpenoids inhibit Candida albicans grow by affecting membrane integrity and arrest od cell cycle. Phytomedicine. 2011;18:1181–90.
Araújo MGF, et al. Evaluation of Syngonanthusnitens (Bong.) Ruhl. extract as antifungal and in treatment of vulvovaginal candidiasis. Med Mycol. 2013;1:1–10.
Eccleston GM. Emulsions and microemilsions. In: Swarbick J, Boylan JC, editors. Encyclopedia of Pharmaceutical Technology. 2nd ed. New York: Marcel Dekker; 2002. p. 1060–85. Vol. 2.
Soper DE. Genitourinary infections and sexually transmitted diseases. In: Berek JS, editors. Berek & Novak’s Gynecology. 14th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p. 1017–48.
Yano J, Fidel PL Jr. Protocols for vaginal inoculation and sample collection in the experimental mouse model of Candida vaginitis. J Vis Exp. 2011;58:1–7.
Carrara M, et al. A new model of vaginal infection by Candida albicans in rats. Mycopathologia. 2010;1:1–8.
Ramos MAS, et al. Syngonanthusnitens Bong. (Rhul.)-loaded nanostructured system for vulvovaginal candidiasis treatment. Int J Mol Sci. 2016;17:1–19.
Karad SC, Purohit VB, Thakor P, Thakkar VR, Raval DK. Novel morpholinoquinoline nucleus clubbed with pyrazoline scaffolds: Synthesis, antibacterial, antitubercular and antimalarial activities. Eur J Med Chem. 2016;112:270–9.
Wei Z, et al. Synthesis and biological evaluation of chalcone derivatives containing aminoguanidine or acylhydrazone moietie. Bioorg Med Chem Lett. 2016;26:5920–5.
Wong SSW, et al. In vitro and in vivo activity of a novel antifungal small molecule against Candida Infections. PLoS ONE 2014;9:1–17.
Nóbrega HN, Ferreira JAB, Romão CMCPA, Capasso IRVF. Atividade antimicrobiana in vitro de produtos antissépticos por meio de técnica. Time Kill Rev Inst Adolfo Lutz. 2013;72:226–33.
Ling LL, et al. New antibiotic kills pathogens without detectable resistance. Nature. 2015;517:455–73.
Perfect JR. The antifungal pipeline: a reality check. Nat Rev Drug Discov. 2017;12:1–14.
Sivakumar PM, Mathu KT, Doble M. Antifungal activity, mechanism and QSAR studies on chalcones. Chem Biol Drug Des. 2009;74:68–79.
Lopez SN, et al. In vitro antifungal evaluation and structure-activity relationships of a new series of chalcone derivatives and synthetic analogues with inhibitory properties against polymers of the fungal cell wall. Bioorg Med Chem. 2001;9:1999–2013.
Hameed A, et al. Anti-HIV cytotoxicity enzyme inhibition and molecular docking studies of quinoline based chalcones as potential non-nucleoside reverse transcriptase inhibitors (NNRT). Bioorg Chem. 2016;65:175–82.
Zenger K, Dutta S, Wolff H, Genton MG, Kraus B. In vitro structure-toxicity relationship of chalcones in human hepatic stellate cells. Toxicology. 2015;2:26–33.
Lee YT, et al. Toxicity assessments of chalcone and some synthetic chalcone analogues in a zebrafish model. Molecules. 2014;19:641–50.
Krcmery V, Kalavsky E. Antifungal drug discovery, six new molecules patented after 10 years of feast: why do we need new patented drugs apart from new strategies? Recent Pat Antiinfect Drug Discov. 2007;2:182–7.
Díaz-Tielas C, Graña E, Reigosa MJ, Sánchez-Moreiras AM. Biological activities and novel applications of chalcones. Planta daninha. 2016;34:607–16.
Messier C, Epifano F, Genovese S, Grenier D. Inhibition of Candida albicans biofilm formation and yeast-hyphal transition by 4-hydroxycordoin. Phytomedicine. 2011;18:380–3.
Acknowledgements
We would like to thank Universidade Federal de São João del-Rei, Conselho Nacional de Desenvolvimento Científico and Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Fundação de Amparo à Pesquisa do estado de Minas Gerais (FAPEMIG) by financial support. JTA and WGL are grateful to UFSJ and FAPEMIG for a fellowship, respectively.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Andrade, J.T., Santos, F.R.S., Lima, W.G. et al. Design, synthesis, biological activity and structure-activity relationship studies of chalcone derivatives as potential anti-Candida agents. J Antibiot 71, 702–712 (2018). https://doi.org/10.1038/s41429-018-0048-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-018-0048-9
This article is cited by
-
Chalcone derivatives disrupt cell membrane integrity of Saccharomyces cerevisiae cells and alter their biochemical composition
Archives of Microbiology (2024)
-
Chalcone Schiff bases disrupt cell membrane integrity of Saccharomyces cerevisiae and Candida albicans cells
Archives of Microbiology (2023)
-
Novel eco-friendly [1,2,4]triazolo[3,4-a]isoquinoline chalcone derivatives efficiency against fungal deterioration of ancient Egyptian mummy cartonnage, Egypt
Archives of Microbiology (2023)
-
Mechanisms of Candida Resistance to Antimycotics and Promising Ways to Overcome It: The Role of Probiotics
Probiotics and Antimicrobial Proteins (2021)
-
Antibacterial and antibiofilm activities of synthetic analogs of 3-alkylpyridine marine alkaloids
Medicinal Chemistry Research (2020)