Abstract
Bcl-2 inhibitors display an effective activity in acute myeloid leukemia (AML), but its clinical efficacy as a monotherapy was limited in part owing to failure to target other antiapoptotic Bcl-2 family proteins, such as Mcl-1. In this context, the combination strategy may be a promising approach to overcome this barrier. Here, we report the preclinical efficacy of a novel strategy combining ABT-199 with triptolide (TPL), a natural product extracted from a traditional Chinese medicine, in AML. Combination treatment exhibited markedly increased cytotoxicity in leukemic cells irrespective of p53 status while largely sparing normal cells of the hematopoietic lineage. Moreover, co-administration of ABT-199 with TPL dramatically suppressed leukemia progression as well as prolonged animal survival in a xenograft AML model. The potentiated effect of ABT-199 and TPL against AML was associated with activation of the mitochondrum-related intrinsic apoptotic pathway through a mechanism reciprocally modulating Bcl-2 family proteins. In this case, TPL not only downregulated Mcl-1 but also upregulated proapoptotic BH3-only proteins, thereby overcoming the resistance toward ABT-199. Conversely, ABT-199 abrogated Bcl-2-mediated cytoprotection against TPL. Together, these findings suggest that the regimen combining TPL and ABT-199 might be active against AML by inducing robust apoptosis through reciprocal regulation of anti- and proapoptotic Bcl-2 family proteins, therefore providing a strong rationale for the clinical investigation of this combination regimen for the treatment of AML.
Similar content being viewed by others
Introduction
Targeted therapies for the treatment of acute myeloid leukemia (AML) have been emerging as a promising strategy to overcome chemo-resistance1. Among numerous potential targets, Bcl-2, an antiapoptotic protein, has been well characterized as one of the most attractive targets involved in chemo-resistance2,3. However, the clinical outcome of AML patients who received the Bcl-2 inhibitor ABT-199 (also known as venetoclax), which has been approved by the FDA for the treatment of chronic lymphocytic leukemia, as monotherapy was discouraging4. Therefore, rational combination approaches may be needed to improve the efficacy of ABT-199 in AML. In this context, when combined with azacitidine, ABT-199 displays superior antileukemia activity in AML patients4,5,6.
Mechanistically, ABT-199 acts as a BH3-mimetic, which is highly selective toward Bcl-27. However, Bcl-2 inhibition could incur the upregulation of Mcl-1, another antiapoptotic protein of the Bcl-2 family, thereby resulting in the resistance to ABT-199 in AML8,9. In this case, although ABT-199 antagonizes the antiapoptotic function of Bcl-2 by releasing BH3-only proteins (e.g., Bim), it does not increase the levels of these proteins, another major factor that determines their proapoptotic effects10. For example, upregulation of BH3 proteins by DNA damage or stress could bind to and activate either or both of the proapoptotic multi-domain protein Bcl-2-associated X protein (BAX) and Bcl-2 antagonist/killer (BAK), triggering apoptosis via mitochondrial outer membrane permeabilization11. As the proapoptotic proteins including BH3-only proteins as well as multi-domain proteins can bind to and be neutralized by multiple antiapoptotic proteins, e.g., Bcl-2, Bcl-xL, Mcl-1, either upregulation of other antiapoptotic proteins (particularly, Mcl-1) or insufficient amount of BH3-only proteins, or both could confer resistance to highly selective Bcl-2 inhibitors like ABT-199 and therefore contribute to the unfavorable clinical outcome of ABT-199 as single agent. Rationally, a combination strategy encompassing both aspects, i.e., disability or downregulation of antiapoptotic proteins (e.g., Bcl-2, Mcl-1) and unleashing or upregulation of proapoptotic BH3-only proteins, may thus overcome such resistance and improve the clinical outcome of Bcl-2 inhibitors like ABT-199.
As reported previously, Mcl-1 was upregulated in chemo-resistant AML cells, an event resulting in intrinsic resistance to ABT-19911. One approach to overcome this resistance is to combine ABT-199 with an Mcl-1 inhibitor, which indeed enhances inhibition of AML cell growth12. However, similar to ABT-199, the Mcl-1 inhibitor has no effect on the levels of BH3-only proteins. Interestingly, it has been reported that the MDM2 inhibitor RG, which activates p53, in combination with ABT-199 exhibits superior antileukemic efficacy and overcome ABT-199 resistance through simultaneous antagonism of Mcl-1 and upregulation of BH3-only proteins13. But this combination strategy was effective only toward p53 wild-type AML cells, but not mutant or null cells. In this context, triptolide (TPL) has been demonstrated to execute its antitumor activity by inducing apoptosis via both p53-dependent and -independent mechanisms14,15,16. Mechanistically, this agent acts to increase the levels of BH3-only proteins (e.g., BIM and BID) as well as to downregulate expression of Mcl-1 in various malignant cells17,18. Considering its properties of not only suppressing Mcl-1 but also upregulate BH3-only proteins, TPL with a broader antileukemia spectrum might thus represent an optimal agent to potentiate antitumor activity of ABT-199 in AML. Here, we report that TPL interacts with ABT-199 to induce apoptosis and overcome ABT-199-resistance through reciprocal regulation of anti- and proapoptotic Bcl-2 family proteins in AML.
Materials and methods
Chemicals and reagents
TPL (formula: C20H24O6, MW: 360.40) and ABT-199 were purchased from Sigma-Aldrich (St. Louis, Missouri, USA) and AbbVie (Chicago, IL, USA), respectively. All compounds were prepared as 10 mm stock solution in 100% dimethyl sulfoxide (Sigma-Aldrich, St Louis, Missouri, USA) and stored at −20 °C or −80 °C. They were diluted to the required concentrations with culture medium immediately before the experiments.
Cell culture and patient samples
MV4–11 and MOLM-13 (TP53 wild type, FLT3-ITD positive) and U937, THP-1, and KG-1a (TP53 mutated or null), as well as MV4–11-luciferase-GEP cells were kindly provided by professor PT Liu (Wellcome Trust Sanger Institute, UK). Cells were cultured in RPMI-1640 medium or Iscove’s modified Dulbecco’s medium (HyClone, Thermo Scientific, MA, USA) supplemented with 10% fetal bovine serum (FBS; Gibco, Life Technologies, NY, USA) at 37 °C in a humidified CO2 incubator. Bone marrow samples were obtained with the informed consent from healthy donors of hematopoietic stem cell transplantation (n = 10) and AML patients (n = 40) at Department of Hematology, the First Affiliated Hospital of Xiamen University (Xiamen, China). Bone marrow mononuclear cells (BMMC) were isolated by density gradient centrifugation using Lymphoprep (BD, Franklin Lakes, NJ, USA) and cultured in RPMI-1640 medium supplemented with 10% FBS. This study was approved by the Ethics Committee of the First Affiliated Hospital of Xiamen University and conducted in agreement with the guidelines of the Declaration of Helsinki and.
Cell proliferation assay
The cytotoxic effect of TPL and ABT-199 toward AML cells was determined by Cell Counting Kit-8 (CCK-8) assay (Dojindo, Kumamoto, Japan). In brief, cells (2 × 104 cells/well) were seeded in 96-well plates containing 100 μl growth medium and treated with designated doses of TPL or ABT-199 alone or in combination for 24 or 48 h. CCK-8 reagents (10 μl/well) were then added and incubated for additional 1–3 h, after which the absorbance at 450 nm was detected by a microplate reader (ELx800; BioTek Instruments Inc., Winooski, VT, USA). The results were obtained from at least three independent experiments and expressed as a mean for percentage of living cells by comparing to untreated control in the same experiment. The inhibitory rate was calculated using the following formula: inhibition rate (%) = (1 − absorbance of experimental group/absorbance of control group) × 100%.
Flow cytometric assay for determining apoptosis and mitochondrial membrane potential
To assess apoptosis, cells were treated with TPL and ABT-199 alone or in combination for 24 and 48 h, followed by staining with Annexin-V-FITC/PI (eBioscience, San Diego, California, USA) for 15 min at room temperature in the dark according to the manufacturer’s instructions. Cells were then analyzed by NovoCyte flow cytometry with NovoExpress software (ACEA Biosciences, Inc., USA) to determine the percentage of Annexin-V positive (apoptotic) cells. Loss of the mitochondrial membrane potential (Δψm) was measured using JC-1 Fluorescent Probe Kit (Beyotime Company, Shanghai, China) by following the manufacturer’s instructions as described previously15. To assess the interaction between TPL and ABT-199, two separate approaches (i.e., CompuSyn and CalcuSyn) were used to calculate the combination index (CI). CI < 1.0 indicates synergism, while CI = 1.0 and CI > 1.0 indicate an additive or antagonistic effect, respectively.
Western blot analysis
After treatment, a total 5 × 106/ml cells per condition were lysed and the protein concentration was determined using BCA Protein Assay Kit (Pierce, Rockford, IL, USA). Whole cell lysates (50 μg for each sample) were electrophoresed in 10% sodium dodecyl sulphate polyacrylamide gel electrophoresis and then transferred to polyvinylidene difluoride membrane (Millipore, Billerica, MA, USA). The membranes were incubated with primary antibodies (1:1000 in 5% bovine serum albumin tris-buffered saline with polysorbate 20; TBS-T) overnight at 4 °C, followed by horseradish peroxidase-conjugated secondary antibodies (Cell Signaling Technology; 1:10,000 in 5% fat-free milk TBS-T) for 1.5 h at room temperature. The primary antibodies against Bcl-2 (CA4223S), Mcl-1 (CA2538S), caspase 3 (CA9662S), caspase 9 (CA5340S), PARP (CA9532S), BIM (CA2933S), PUMA (CA3741S), BID (CA7382S), and β-actin (CA4970S) were purchased from Cell Signaling Technology (Danvers, MA, USA). The blots were probed with anti-β-actin antibody (rabbit mAb 1:1000, Cell Signaling Technology) to ensure equal loading and transfer. The proteins were visualized using ECL Western Blotting Detection Kit (Gene-Flow, Staffordshire, UK).
Animal study
The animal study was approved by the First Affiliated Hospital of Xiamen University Animal Care and Use Committee. Two xenograft models were employed in this study. For the model #1, 5~6 week-old female BALB/C nude mice (18–20 g; Beijing HFK bioscience Co. Ltd.) were injected subcutaneously with 5.8 × 106 MOLM-13 cells at the right flank of mice. Once the tumor volume reached to ~75 mm3, mice were randomly assigned to four groups (n = 5/group), including control, TPL, ABT-199, and combination, and treated for 2 consecutive weeks with vehicle (0.2% methyl cellulose and 0.1% Tween-80 in PBS), TPL (0.5 mg/kg/day, intraperitoneal injection), ABT-199 (50 mg/kg/day, oral gavage), or combination of TPL and ABT-199, respectively. During treatment, mice were monitored and weighed daily for toxicity. After 2 weeks of treatment, tumor volume (V) was measured daily by caliper and calculated using the equation: V = (L × W2)/2, where L and W represent the length and width of tumor, respectively.
For the model #2, six-week-old male NOD-SCID IL-2Rγ null (NSG) mice (BEIJING IDMO Co. Ltd, China) were injected intravenously with 4 × 106 MV4–11-luciferase-GFP cells. After engraftment was confirmed, mice were randomly assigned to four groups (n = 7/group) and treated daily with vehicle, TPL (0.5 mg/kg/day, intraperitoneal injection), ABT-199 (50 mg/kg/day, oral gavage), or their combination. The tumor burden was monitored by bioluminescent imaging at designated time points. In brief, mice were anesthetized and injected intraperitoneally with the firefly luciferase substrate d-luciferin (Gold Biotechnology, St. Louis, MO, USA) and then imaged using IVIS-200 Imaging System (PerkinElmer, Waltham, MA, USA). Five mice in each group were used for the analysis of animal survival. Other two mice in each group were killed at day 21 for control group, day 28 for ABT-199 or TPL group, and day 35 for combinatory group. Spleens were removed and subjected to immunohistochemical staining with human CD45 antibody or western blot analysis on whole tissue homogenate.
Statistical analysis
The value was expressed as the mean ± standard deviation (S.D.) for at least three independent experiments. Two groups were compared using the Student t test. Multiple-group comparisons were conducted using the one-way analysis of variance followed by the Bonferroni post hoc test. Survival was estimated using the Kaplan–Meier analysis and analyzed with the log-rank test. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 20.0 software (La Jolla, CA).
Results
Co-treatment with TPL and ABT-199 markedly induces apoptosis in AML cells, irrespective of p53 status
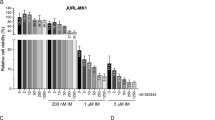
First, we examined whether the combination of TPL and ABT-199 would have an interactive effect on AML cells. To this end, various leukemia cell lines (including p53 wild type and mutation/null) were treated with indicated concentrations of TPL and ABT-199, after which cell viability was analyzed using CCK-8 assay. As shown in Fig. 1a, b, treatment with TPL and ABT-199 alone significantly inhibited cell growth in a dose-dependent manner in both p53 wild type (MV4–11 and MOLM-13, both carrying FLT3-ITD, a genetic marker for poor prognosis; Fig. 1a) and mutant or null cells (U937, THP-1, and KG-1α; Fig. 1b). Notably, co-administration of TPL and ABT-199 led to markedly enhanced growth inhibition in all of these AML cell lines (Fig. 1a, b). To verify whether the cytotoxicity of TPL and ABT-199 was associated with induction of apoptosis, the percentage of apoptotic cells was determined by Annexin-V/PI dual staining. As shown in Fig. 1c, d, each single-agent treatment resulted in a modest increase in apoptosis, whereas the percentage of apoptotic cells was dramatically increased after co-exposure to TPL and ABT-199. CI values were further determined using the Calcusyn and CompuSyn software, respectively. CI < 1.0 for virtually all conditions (except two conditions for Molm13) indicates synergism between TPL and ABT-199 in both p53 wild type (Fig. 1e and Supplementary Fig. 1A, B) and mutant/null AML cell lines (Fig. 1f and Supplementary Fig. 1C–E). These results were confirmed by another analysis using the Bliss Independence model (Supplemental Table S1). Together, these findings suggest that the combination of TPL and ABT-199 might markedly reduced cell viability and markedly induce apoptosis in AML cells regardless of their p53 status.
a, b Inhibition on proliferation of both p53 wild type (MV4–11 and MOLM-13) and mutant/null AML cells (KG-1a, U937, and THP-1) were exposed to the indicated concentrations of TPL ± ABT-199 for 48 h, after which the CCK-8 assay was performed to monitor cell viability. c, d Alternatively, cells were treated with the indicated concentrations of TPL ± ABT-199 for 48 h, after which the percentage of Annexin-V+apoptotic cells was determined by flow cytometry after Annexin-V and PI double staining. e, f The combination index (CI) was calculated based on apoptosis using the CompuSyn and CalcuSyn software to evaluate the interaction between TPL and ABT-199 in both p53 wild type and mutant/null AML cell lines (CI < 1.0 = 1.0, and >1.0, indicating synergistic, additive, and antagonistic effect, respectively). ABT, ABT-199; Comb: combination of TPL and ABT-199.
Combined treatment with TPL and ABT-199 results in an enhanced cytotoxicity against primary AML blasts, whereas largely sparing normal BMMCs
The antileukemic effect of TPL and ABT-199 alone or in combination was further investigated ex vivo in the primary blasts isolated from 40 AML patients and BMMCs from 10 healthy donors. Clinical characteristics of the patients were summarized in Table 1. Consistent with the results obtained from AML cell lines, co-treatment of primary AML blasts with TPL and ABT-199 at the concentrations ranging from 1.25 to 5 nmol/L resulted in significant increased in the percentage of apoptotic cells when compared with each agent alone (Fig. 2a). In sharp contrast, combined treatment with TPL and ABT-199 at the same dose range had almost no cytotoxicity toward BMMCs obtained from healthy donors (Fig. 2b). Together, these results suggest that the combination of TPL with ABT-199 might be preferably targeted AML blasts while potentially sparing normal cells of the hematopoietic lineage.
a, b Primary blasts and bone marrow mononuclear cells (BMMC) were isolated from 40 patients with AML and 10 healthy donors, respectively. Cells were exposed to the indicated concentrations (nm) of TPL (T) or ABT-199 (A) alone or in combination c for 48 h, after which the percentage of Annexin-V + apoptotic cells was determined by flow cytometry after Annexin-V and PI double staining. *P < 0.05, **P < 0.01.
The regimen combining TPL and ABT-199 displays antileukemic activity in murine xenograft models
We next evaluated the activity and toxicity of the regimen combining TPL and ABT-199 in two xenograft models bearing either MOLM-13 or MV4–11 cells, both of which carry FLT-ITD, representing an AML subset with poor clinical outcomes. The first model established by subcutaneously inoculating MOLM-13 cell line into flank of mice were treated with vehicle, TPL, ABT-199, or their combination, respectively. Compared with each single agent, combined treatment resulted in a marked inhibition of tumor growth (Fig. 3a), manifested by a significant reduction in tumor volume and weight (Fig. 3b,c). Of note, this combination regimen was well tolerated, without significant loss of body weight (Fig. 3d). Moreover, toxicity of TPL was further examined in non-immunocompromised mice. Neither blood cell account nor liver function was affected when compared with control group (Supplementary Fig. 2), supporting a notion that the dose of TPL used in this study is tolerable.
a–d BALB/C nude mice were injected subcutaneously with 5.8 × 106 MOLM-13 cells at the right flank. Once the tumor volume reached to ~75 mm3, mice were randomly assigned to four groups (n = 5/group) including control (ctrl), TPL, ABT-199, and combination (combo), and treated for 2 consecutive weeks with vehicle (0.2% methyl cellulose and 0.1% Tween-80 in PBS), TPL (0.5 mg/kg/day, intraperitoneal injection), ABT-199 (50 mg/kg/day, oral gavage), or combination of TPL and ABT-199, respectively. At the end of the study, images of mice and removed tumors were captured a, and tumor volume b and weight c were measured. During treatment, body weight of mice was monitored daily d. Data represent the mean ± SD. e, f NOD-SCID IL-2Rγ null mice were injected intravenously with 4 × 106 MV4–11-luciferase-GFP cells. After engraftment was confirmed, mice were randomly assigned to four groups (n = 7/group) and treated daily with vehicle (ctrl), TPL (0.5 mg/kg/day, intraperitoneal injection), ABT-199 (50 mg/kg/day, oral gavage) or their combination (Combo). The tumor burden was monitored by bioluminescent imaging at designated time points e. Animal survival was analyzed using the Kaplan–Meier survival curve f. *P < 0.05, **P < 0.01.
To further investigate whether the combination of TPL and ABT-199 would confer a survival benefit, the second xenograft model was established by intravenously injecting with GFP/luciferase-labeled MV4–11 cells. Mice were then treated with vehicle, TPL (0.5 mg/kg/day), ABT-199 (50 mg/kg/day) or their combination, respectively. As shown in Fig. 3e, TPL or ABT-199 administrated individually resulted in a moderate reduction in tumor burden, whereas combined treatment remarkably reduced tumor burden. Consistently, although mice received TPL and ABT-199 as single agent displayed longer survival than those only received vehicle, combined treatment led to markedly prolonged survival, compared with each agent alone, with median survival time of 38 days for the combination group vs 32 days for ABT-199 or 30 days for TPL monotherapy group (Fig. 3f, p < 0.05 for each case).
Antileukemic effect of ABT-199 and TPL is associated with activation of the intrinsic apoptotic pathway
To examine whether cytotoxicity of the TPL+ABT-199 combination is associated with activation of the intrinsic apoptotic pathway, cleavage of caspases and PARP, markers of apoptosis were first monitored. As shown in Fig. 4a, b, treatment with ABT-199 and TPL in combination markedly increased cleavage of caspase 9, caspase 3 and PARP, compared with each agent administrated individually in both p53 wild type MV4–11 (Fig. 4a) and p53 mutant KG-1α cells (Fig. 4b). Flow cytometry was then performed to assess depolarization of mitochondrial membrane. Consistent to induction of apoptosis, co-treatment with TPL and ABT-199 resulted in a marked loss of mitochondrial membrane enhanced in a dose-dependent manner in MV4–11 (Fig. 4c) and KG-1α cells (Fig. 4d), suggesting activation of the mitochondrum-related intrinsic apoptotic pathway. Last, Z-VAD-fmk, a pan-caspase inhibitor, was used to rescue apoptosis induced by the combination treatment. Indeed, Z-VAD-fmk significantly prevent leukemic cells from apoptosis induced by the combination of TPL and ABT-199 in both MV4–11 (Fig. 4e) and KG-1α (Fig. 4f). Together, these results suggest that the antileukemic effect of ABT-199 and TPL in combination might primarily stem from activation of the intrinsic apoptotic pathway.
a, b MV4–11 and KG-1α cells were exposed to the indicated concentrations of TPL ± ABT-199 for 48 h, after which western blot analysis was performed to monitor cleavage caspase 3, caspase 9, and PARP. c, d Alternatively, cells were treated with the indicated concentrations of TPL ± ABT-199 for 48 h, after which flow cytometry was performed to assess depolarization of mitochondrial membrane after JC-1 staining. e, f MV4–11 and KG-1α cells were incubated for 24 h with the indicated concentrations of TPL ± ABT-199 in the absence or presence of the pan-caspase inhibitor Z-VAD-fmk, after which the percentage of apoptotic cells was determined by flow cytometry after Annexin-V and PI staining.
Reciprocal regulation of Bcl-2 family proteins contributes to activity of TPL and ABT-199 against AML cells
Finally, the mechanism of action of the TPL+ABT-199 combination was investigated. As the effect of TPL and ABT-199 was associated with activation of the mitochondrial apoptotic pathway that is primarily governed by pro- and antiapoptotic proteins of the Bcl-2 family19, the expression of Bcl-2 family proteins was monitored at 12 hr after drug treatment, prior to apoptosis (Supplementary Fig. 3). As shown in Fig. 5a, b, whereas ABT-199 barely affect the levels of Bcl-2 and Mcl-1, TPL moderately but clearly reduced the expression of Mcl-1 but not Bcl-2. Notably, combined treatment with TPL and ABT-199 markedly reduced the protein levels of both Bcl-2 and Mcl-1 in MV4–11 (Fig. 5a) and KG-1α cells (Fig. 5b), an event occurred prior to cleavage of caspase 3 and PARP. In parallel, exposure to TPL or ABT-199 alone resulted in a moderate increase in the protein levels of several BH3-only proteins, including PUMA, BIM, BID, and NOXA, co-treatment with two agents dramatically upregulated the expression of these proapoptotic proteins (Fig. 5a, b).
a, b MV4–11 and KG-1α cells were exposed to the indicated concentrations of TPL ± ABT-199 for 12 h, after which western blot analysis was performed to monitor expression of proapoptotic BH3-only proteins (PUMA, NOXA, BID, BIM) and antiapoptotic proteins (Bcl-2 and Mcl-1), as well as cleavage of caspase 3 and PARP. c, d Animal study was performed as described in Fig. 3e, f, after which spleen was removed at the indicated time points (Ctrl, day 21; TPL and ABT-199 alone, day 28; combination, day 35) and subjected to immunohistochemical staining (IHC) for human CD45 c (Scale bar, 35 μm) and western blot analysis for BH3-only proteins (NOXA, BIM), Bcl-2, and Mcl-1 on spleen homogenate.
Similar phenomena were observed in infiltrating leukemic cells in spleen of xenograft mice bearing GFP/luciferase-labeled MV4–11 cells. It was noticed that although TPL or ABT-199 as monotherapy displayed a moderate but clear suppressive effect on tumor growth at early time points, neither of them was able to prevent progression of leukemia at late stage (e.g., day 28; Fig. 3e). As shown in Fig. 5c, combined treatment with TPL and ABT-199 markedly reduced the amount of infiltrating leukemia cells in spleen harvested at indicated time points, consistent with the observation that the combination virtually eliminated tumor burden (Fig. 3e). Interestingly, western blot revealed that the protein level of Mcl-1 and Bcl-2 was increased in ABT-199 and TPL group, respectively (Fig. 5d), probably accounting for the insufficiency of either agent alone to prevent disease progression. However, these events were diminished by combination treatment, accompanied by upregulation of proapoptotic BH3-only proteins such as BIM and NOXA (Fig. 5d). Together, these findings argue that TPL and ABT-199 might interact to induce robust apoptosis and overcome resistance to each single drug through disruption of the compensatory responses to these agents alone by simultaneously downregulation of antiapoptotic Bcl-2 family proteins and upregulation of proapoptotic BH3-only proteins in AML cells.
Discussion
Most targeted therapies focus on upstream nodes of tumor-driven signaling pathways19. However, drug resistance is often inevitable especially for the monotherapy of targeted agents due to various compensatory mechanisms via the complex signaling networks19,20. In this context, the Bcl-2-selective inhibitor ABT-199 as monotherapy has displayed a limited efficacy due to compensatory upregulation of Mcl-1 and/or incapability to induce BH3-only protein expression12,21. Thus, the combination approach is required for overcoming this barrier and thereby potentiate antitumor activity of ABT-199. An ideal partner for such a combination strategy compound should be able to not only enhance proapoptotic effect of ABT-199 by up-regulating BH3-only proteins but also overcome its resistance due to Mcl-1 upregulation. In this study, we found that TPL interacts ABT-199 to markedly induce apoptosis in AML cells irrespective of p53 status. We also noticed that in contrast to transient inhibitory effect of TPL or ABT-199 monotherapy, the regimen combining these two agents displays persistent antileukemic activity in vivo, while is well tolerated.
To overcome Mcl-1-mediated resistance of ABT-199 in AML cells, Mcl-1 inhibitors have been used to reverse this resistance. Indeed, combination of an Mcl-1 inhibitor and ABT-199 did enhance the inhibition of leukemia growth. However, this strategy might be further optimized, because both ABT-199 and Mcl-1 inhibitors are BH3 mimetics that antagonize antiapoptotic proteins of the Bcl-2 family but do not affect the expression of BH3-only proteins in AML cells21. In this context, BH3-only proteins are considered as a key factor to initiate the intrinsic apoptotic pathway10,22. As ABT-199 or Mcl-1 inhibitors can only release the preexisted BH3-only proteins from binding of neutralization by Bcl-2 or Mcl-1, an ideal candidate partner for combining with ABT-199 would be an agent that not only downregulate or inhibit Mcl-1 but also upregulate BH3-only proteins. For example, it has been demonstrated that a p53 activator in combination with ABT-199 could result in synthetic lethality by both targeting Mcl-1 and up-regulating BH3-only proteins in AML cells13. Unfortunately, this combination approach was effective only against p53 wild-type AML, whereas failed to kill AML cells carrying p53 mutation or deletion, a common and poor-prognostic genetic abnormality in this disease. In this study, we found that although AML cells carrying p53 mutation or deletion seemed less sensitive to ABT-199 or TPL than those with wild-type p53, the regimen combining TPL and ABT-199 markedly induced apoptosis and displayed a significantly increased antitumor activity in AML regardless of p53 status. It is noteworthy that the concentrations of ABT-199 and TPL used in this study were comparable to the achievable plasma concentrations in clinical settings23,24. In ranges of these concentrations, neither agent alone nor in combination resulted in significant toxicity toward BMMC obtained from healthy donors, suggesting that these dose ranges might be tolerated in vivo. Therefore, the regimen combining TPL with ABT-199 might have a broader antileukemic spectrum in AML carrying both wild type and mutant/deleted p53, with a likelihood of clinical tolerability.
Mechanistically, the marked antileukemic effect of TPL and ABT-199 in AML was associated with activation of the mitochondrum-related intrinsic apoptotic pathway through reciprocal regulation of both anti- and proapoptotic Bcl-2 family proteins. In this case, TPL could not only downregulate Mcl-1 but also upregulate BH3-only proteins, which compensate for the Mcl-1-mediated resistance to ABT-199. Conversely, ABT-199 might rescues Bcl-2-mediated paralysis toward TPL. Together, combination of TPL and ABT-199 might potentially overcome drug resistance to both agents. As a consequence, the regimen combining TPL and ABT-199 displayed a potent and persistent antileukemic efficacy in vitro and in vivo, as well as conferred a superior animal survival in the murine xenograft AML models. However, a possibility that the mechanisms, other than those involving the Bcl-2 family, might also contribute to the interaction between ABT-199 and TPL could not be excluded.
In summary, this study provides strong preclinical evidence supporting that a novel strategy combining TPL and ABT-199 markedly induces apoptosis of AML cells regardless of their p53 status and thereby displays the markedly improved efficacy towards AML in vitro and in vivo. Mechanistically, the interaction between these two agents is associated with reciprocal regulation of anti- and proapoptotic Bcl-2 family proteins, which might thus overcome drug resistance for each single agent administrated as monotherapy. Therefore, this combination regimen warrants further clinical investigation for the treatment of AML patients, particularly those carrying adverse genetic abnormalities such as p53 mutation or deletion.
References
Ricciardi, M. R., Mirabilii, S., Licchetta, R., Piedimonte, M. & Tafuri, A. Targeting the Akt, GSK-3, Bcl-2 axis in acute myeloid leukemia. Adv. Biol. Regul.65, 36–58 (2017).
Konopleva, M. & Letai, A. BCL-2 inhibition in AML: an unexpected bonus? Blood132, 1007–1012 (2018).
Yogarajah, M. & Stone, R. M. A concise review of BCL-2 inhibition in acute myeloid leukemia. Exp. Rev. Hematol.11, 145–154 (2018).
Sharma, P. & Pollyea, D. A. Shutting down acute myeloid leukemia and myelodysplastic syndrome with BCL-2 family protein inhibition. Curr. Hematol. Malig. Rep.13, 256–264 (2018).
Pollyea, D. A. et al. Venetoclax with azacitidine disrupts energy metabolism and targets leukemia stem cells in patients with acute myeloid leukemia. Nat. Med.24, 1859–1866 (2018).
Nguyen, L. X. T. et al. The Bcl-2 inhibitor venetoclax inhibits Nrf2 antioxidant pathway activation induced by hypomethylating agents in AML. J. Cell Physiol.234, 14040–14049 (2019).
Delbridge, A. R., Grabow, S., Strasser, A. & Vaux, D. L. Thirty years of BCL-2: translating cell death discoveries into novel cancer therapies. Nat. Rev. Cancer16, 99–109 (2016).
Pan, R. et al. Inhibition of Mcl-1 with the pan-Bcl-2 family inhibitor (−)BI97D6 overcomes ABT-737 resistance in acute myeloid leukemia. Blood126, 363–372 (2015).
Rahmani, M. et al. Cotargeting BCL-2 and PI3K induces BAX-dependent mitochondrial apoptosis in AML cells. Cancer Res.78, 3075–3086 (2018).
Ashkenazi, A., Fairbrother, W. J., Leverson, J. D. & Souers, A. J. From basic apoptosis discoveries to advanced selective BCL-2 family inhibitors. Nat. Rev. Drug Discov.16, 273–284 (2017).
Singh, R., Letai, A. & Sarosiek, K. Regulation of apoptosis in health and disease: the balancing act of BCL-2 family proteins. Nat. Rev. Mol. Cell Biol.20, 175–193 (2019).
Luedtke, D. A. et al. Inhibition of Mcl-1 enhances cell death induced by the Bcl-2-selective inhibitor ABT-199 in acute myeloid leukemia cells. Signal Transduct. Target Ther.2, 17012 (2017).
Pan, R. et al. Synthetic lethality of combined Bcl-2 inhibition and p53 activation in AML: mechanisms and superior antileukemic efficacy. Cancer Cell32, 748–760 (2017).
Chen, F. et al. Triptolide, a Chinese herbal extract, enhances drug sensitivity of resistant myeloid leukemia cell lines through downregulation of HIF-1alpha and Nrf2. Pharmacogenomics14, 1305–1317 (2013).
Zhao, H. et al. Low dose triptolide reverses chemoresistance in adult acute lymphoblastic leukemia cells via reactive oxygen species generation and DNA damage response disruption. Oncotarget7, 85515–85528 (2016).
Zhou, Z. L., Yang, Y. X., Ding, J., Li, Y. C. & Miao, Z. H. Triptolide: structural modifications, structure-activity relationships, bioactivities, clinical development and mechanisms. Nat. Prod. Rep.29, 457–475 (2012).
Carter, B. Z. et al. Triptolide induces caspase-dependent cell death mediated via the mitochondrial pathway in leukemic cells. Blood108, 630–637 (2006).
Hou, Z. Y., Tong, X. P., Peng, Y. B., Zhang, B. K. & Yan, M. Broad targeting of triptolide to resistance and sensitization for cancer therapy. Biomed. Pharmacother.104, 771–780 (2018).
Chandarlapaty, S. Negative feedback and adaptive resistance to the targeted therapy of cancer. Cancer Discov.2, 311–319 (2012).
Trusolino, L. & Bertotti, A. Compensatory pathways in oncogenic kinase signaling and resistance to targeted therapies: six degrees of separation. Cancer Discov.2, 876–880 (2012).
Niu, X. et al. Binding of released Bim to Mcl-1 is a mechanism of intrinsic resistance to ABT-199 which can be overcome by combination with daunorubicin or cytarabine in AML cells. Clin. Cancer Res.22, 4440–4451 (2016).
Reichenbach, F. et al. Mitochondrial BAX determines the predisposition to apoptosis in human AML. Clin. Cancer Res.23, 4805–4816 (2017).
Salem, A. H., Dunbar, M. & Agarwal, S. K. Pharmacokinetics of venetoclax in patients with 17p deletion chronic lymphocytic leukemia. Anti-cancer Drugs28, 911–914 (2017).
Han, R., Rostami-Yazdi, M., Gerdes, S. & Mrowietz, U. Triptolide in the treatment of psoriasis and other immune-mediated inflammatory diseases. Br. J. Clin. Pharm.74, 424–436 (2012).
Acknowledgements
The work was supported by National Natural Science Foundation of China (grant no. 81570156, 81770126, 81800163, and 81770161); Y.F. Shi and L.L. He performed the experiments and analysis of data. L. Liu collected primary AML samples and interpret data and wrote the manuscript. J. Ye, D.L. Yuan, and M.M. Deng performed the experiments. Z.J. Lin collected donor bone marrow samples. B. Xu, B.Z. Carter, and Z.H. Fang contributed to study design, data analysis, and interpretation and manuscript revision.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by G. Dewson
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, YF., Liu, L., He, LL. et al. Combining triptolide with ABT-199 is effective against acute myeloid leukemia through reciprocal regulation of Bcl-2 family proteins and activation of the intrinsic apoptotic pathway. Cell Death Dis 11, 555 (2020). https://doi.org/10.1038/s41419-020-02762-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41419-020-02762-w
This article is cited by
-
Bcl-2 inhibition combined with PPARα activation synergistically targets leukemic stem cell-like cells in acute myeloid leukemia
Cell Death & Disease (2023)
-
Increased MCL1 dependency leads to new applications of BH3-mimetics in drug-resistant neuroblastoma
British Journal of Cancer (2023)
-
Therapeutic synergy of Triptolide and MDM2 inhibitor against acute myeloid leukemia through modulation of p53-dependent and -independent pathways
Experimental Hematology & Oncology (2022)
-
BH3-mimetics: recent developments in cancer therapy
Journal of Experimental & Clinical Cancer Research (2021)