Abstract
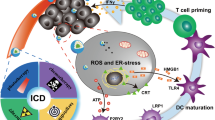
Nowadays, the landscape of cancer treatments has broadened thanks to the clinical application of immunotherapeutics. After decades of failures, cancer immunotherapy represents an exciting alternative for those patients suffering from a wide variety of cancers, especially for those skin cancers, such as the early stages of melanoma. However, those cancers affecting internal organs still face a long way to success, because of the poor biodistribution of immunotherapies. Here, nanomedicine appears as a hopeful strategy to modulate the biodistribution aiming at target organ accumulation. In this way, efficacy will be improved, while reducing the side effects at the same time. In this review, we aim to highlight the most promising cancer immunotherapeutic strategies. From monoclonal antibodies and their traditional use as targeted therapies to their current use as immune checkpoint inhibitors; as well as adoptive cell transfer therapies; oncolytic viruses, and therapeutic cancer vaccination. Then, we aim to discuss the important role of nanomedicine to improve the performance of these immunotherapeutic tools to finally review the already marketed nanomedicine-based cancer immunotherapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
GCO. Global Cancer Observatory. 2020. p. 1–2.
Abbas Z, Rehman S. An overview of cancer treatment modalities. In: Shahzad HN, editor. Neoplasm; 2018.
Morrissey K, Yuraszeck T, Li CC, Zhang Y, Kasichayanula S. Immunotherapy and novel combinations in oncology: current landscape, challenges, and opportunities. Clin Transl Sci. 2016;9:89–104.
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, et al. On the receiving end-patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol. 1983;19:203–8.
Farkona S, Diamandis EP, Blasutig IM. Cancer immunotherapy: the beginning of the end of cancer? BMC Med. 2016;14:1–18.
Weiner LM, Murray JC, Shuptrine CW. Antibody-based immunotherapy of cancer. Cell. 2012;148:1081–4.
Topalian SL, Weiner GJ, Pardoll DM. Cancer immunotherapy comes of age. J Clin Oncol. 2011;29:4828–36.
Sambi M, Bagheri L, Szewczuk MR. Current challenges in cancer immunotherapy: Multimodal approaches to improve efficacy and patient response rates. J Oncol. 2019;4508794.
Martin JD, Cabral H, Stylianopoulos T, Jain RK. Improving cancer immunotherapy using nanomedicines: progress, opportunities and challenges. Nat Rev Clin Oncol. 2020;17:251–66.
Howard KA, Vorup-jensen T, Peer D. Nanomedicine. Springer; 2016.
Hare JI, Lammers T, Ashford MB, Puri S, Storm G, Barry ST. Challenges and strategies in anti-cancer nanomedicine development: an industry perspective. Adv Drug Deliv Rev. 2017;108:25–38.
Bawa R, Audette GF, Rubinstein I. Clinical nanomedicine. Vol. 1; 2016.
Wicki A, Witzigmann D, Balasubramanian V, Huwyler J. Nanomedicine in cancer therapy: Challenges, opportunities, and clinical applications. J Control Release. 2015;200:138–57.
Singh M, Salnikova M, editors. Novel approaches and strategies for biologics, vaccines and cancer therapies. Academic Press, Elsevier; 2015.
Levene AP, Singh G, Palmieri C. Therapeutic monoclonal antibodies in oncology. J R Soc Med. 2005;98:146–52.
Simpson A, Caballero O. Monoclonal antibodies for the therapy of cancer. BMC Proc. 2014;8:6–8.
Harris TJ, Drake CG. Primer on tumor immunology and cancer immunotherapy. J Immunother Cancer. 2013;1:1–9.
Kimiz-Gebologlu I, Gulce-Iz S, Biray-Avci C. Monoclonal antibodies in cancer immunotherapy. Mol Biol Rep. 2018;45:2935–40.
Lefebvre ML, Krause SW, Salcedo M, Nardin A. Ex vivo-activated human macrophages kill chronic lymphocytic leukemia cells in the presence of rituximab: mechanism of antibody-dependent cellular cytotoxicity and impact of human serum. J Immunother. 2006;29:388–97.
van de Donk NWCJ. Immunomodulatory effects of CD38-targeting antibodies. Immunol Lett. 2018;199:16–22.
Segal DM, Weiner GJ, Weiner LM. Bispecific antibodies in cancer therapy. Curr Opin Immunol. 1999;11:558–62.
Fan G, Wang Z, Hao M, Li J. Bispecific antibodies and their applications. J Hematol Oncol. 2015;8:130.
Spiess C, Zhai Q, Carter PJ. Alternative molecular formats and therapeutic applications for bispecific antibodies. Mol Immunol. 2015;67:95–106.
Chelius DC, Gruber P, Plöscher M, Liedtke R, Gansberger E, Hess J, et al. Structural and functional characterization of the trifunctional antibody catumaxomab. MAbs 2010;2:309–19.
Kubota T, Niwa R, Satoh M, Akinaga S, Shitara K, Hanai N. Engineered therapeutic antibodies with improved effector functions. Cancer Sci. 2009;100:1566–72.
Papachristos A, Pippa N, Demetzos C, Sivolapenko G. Antibody-drug conjugates: a mini-review. The synopsis of two approved medicines. Drug Deliv. 2016;23:1662–6.
Thomas A, Teicher BA, Hassan R. Antibody–drug conjugates for cancer therapy. Lancet Oncol. 2016;17:e254–62.
Abdollahpour-Alitappeh M, Lotfinia M, Gharibi T, Mardaneh J, Farhadihosseinabadi B, Larki P, et al. Antibody–drug conjugates (ADCs) for cancer therapy: Strategies, challenges, and successes. J Cell Physiol. 2019;234:5628–42.
Nejadmoghaddam M, Minai-tehrani A, Ghahremanzadeh R. Antibody-drug conjugates: possibilities and challenges. Avicenna J Med Biotechnol. 2019;11:3–23.
Chen H, Lin Z, Arnst KE, Miller DD, Li W. Tubulin inhibitor-based antibody-drug conjugates for cancer therapy. Molecules. 2017;22:1281.
Gheibi Hayat SM, Sahebkar AH. Antibody drug conjugates for cancer therapy. J Babol Univ Med Sci. 2017;19:20–7.
Fu Y, Ho M. DNA damaging agent-based antibody-drug conjugates for cancer therapy. Antib Ther. 2018;1:43–53.
Sau S, Alsaab HO, Kashaw SK, Tatiparti K, Iyer AK. Advances in antibody–drug conjugates: A new era of targeted cancer therapy. Drug Discov Today. 2017;22:1547–56.
Dyck L, Mills KHG. Immune checkpoints and their inhibition in cancer and infectious diseases. Eur J Immunol. 2017;47:765–79.
Huang PW, Chang JWC. Immune checkpoint inhibitors win the 2018 Nobel Prize. Biomed J 2019;42:299–306.
Jenkins RW, Barbie DA, Flaherty KT. Mechanisms of resistance to immune checkpoint inhibitors. Nat Publ Gr. 2018;118:9–16.
Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science. 1996;271:1734–6.
Chambers CA, Kuhns MS, Egen JG, Allison JP. CTLA-4-mediated inhibition in regulation of T cell responses: mechanisms and manipulation in tumor Immunotherapy. Annu Rev Immunol. 2001;19:565–94.
Chang J-F, Phillips J, Kufe D, Greenburg G. MUC1 can function as a potent negative regulator of T cell activation. FASEB J. 1998;12:405–13.
Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–64.
Moya-Horno I, Viteri S, Karachaliou N, Rosell R. Combination of immunotherapy with targeted therapies in advanced non-small cell lung cancer (NSCLC). Ther Adv Med Oncol. 2018;10:1–12.
Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science. 2018;359:1350–5.
Okazaki T, Honjo T. PD-1 and PD-1 ligands: from discovery to clinical application. Int Immunol. 2007;19:813–24.
Fessler MB, Rudel, Lawrence L, Brown M. 基因的改变NIH public access. Bone 2008;23:1–7.
Guo L, Zhang H, Chen B. Nivolumab as programmed death-1 (PD-1) inhibitor for targeted immunotherapy in tumor. J Cancer. 2017;8:410–6.
Cyprian FS, Akhtar S, Gatalica Z, Vranic S. Targeted immunotherapy with a checkpoint inhibitor in combination with chemotherapy: A new clinical paradigm in the treatment of triple-negative breast cancer. Bosn J Basic Med Sci. 2019;19:227–33.
Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192:1027–34.
Gaillard SL, Secord AA, Monk B. The role of immune checkpoint inhibition in the treatment of ovarian cancer. Gynecol Oncol Res Pr. 2016;3:1–14.
Buchbinder EI, Desai A. CTLA-4 and PD-1 pathways similarities, differences, and implications of their inhibition. Am J Clin Oncol. Cancer Clin Trials. 2016;39:98–106.
Hargadon KM, Johnson CE, Williams CJ. Immune checkpoint blockade therapy for cancer: An overview of FDA-approved immune checkpoint inhibitors. Int Immunopharmacol. 2018;62:29–39. (July)
Ramagopal UA, Liu W, Garrett-Thomson SC, Bonanno JB, Yan Q, Srinivasan M, et al. Structural basis for cancer immunotherapy by the first-in-class checkpoint inhibitor ipilimumab. Proc Natl Acad Sci USA. 2017;114:E4223–32.
García-Fernandez C, Fornaguera C, Borrós S. Nanomedicine in non-small cell lung cancer: from conventional treatments to immunotherapy. Cancers 2020;12:1609.
Rosenberg SA, Restifo NP, Yang JC, Morgan RA, Mark E. Adoptive cell transfer: a clinical path to effective cancer immunotherapy. Nat Rev Cancer. 2008;8:299–308.
Subklewe M, Von Bergwelt-Baildon M, Humpe A. Chimeric antigen receptor T cells: a race to revolutionize cancer therapy. Transfus Med Hemotherapy. 2019;46:15–24.
Rohaan MW, Wilgenhof S, Haanen JBAG. Adoptive cellular therapies: the current landscape. Virchows Arch. 2019;474:449–61.
Nethanel T, Moav N, Ran M, Witz IP. Separation of tumor-seeking small lymphocytes and tumor cells using Percoll velocity gradients. J Immunol Methods. 1981;41:43–56.
Geukes Foppen MH, Donia M, Svane IM, Haanen JBAG. Tumor-infiltrating lymphocytes for the treatment of metastatic cancer. Mol Oncol. 2015;9:1918–35.
Dudley ME, Wunderlich JR, Shelton TE, Even J, Rosenberg SA. Generation of tumor-infiltrating lymphocyte cultures for use in adoptive transfer therapy for melanoma patients. J Immunother. 2003;26:332–42.
Gattinoni L, Finkelstein SE, Klebanoff CA, Antony PA, Palmer DC, Spiess PJ, et al. Removal of homeostatic cytokine sinks by lymphodepletion enhances the efficacy of adoptively transferred tumor-specific CD8+ T cells. J Exp Med. 2005;202:907–12.
Idos GE, Kwok J, Bonthala N, Kysh L, Gruber SB, Qu C. The prognostic implications of tumor infiltrating lymphocytes in colorectal cancer: a systematic review and meta-analysis. Sci Rep. 2020;10:1–14.
Monaco SE, Pantanowitz L, Xing J, Cuda J, Kammula US. Cytologic evaluation of tumor-infiltrating lymphocytes for adoptive cell therapy. Am J Clin Pathol. 2020;153:513–23.
Smith-garvin JE, Koretzky GA, Jordan MS. NIH public access - T cell activation. Immunology 2010;27:591–619.
Abraham RT, Weiss A. Jurkat T cells and development of the T-cell receptor signalling paradigm. Nat Rev Immunol. 2004;4:301–8.
Linnemann C, Schumacher TNM, Bendle GM. T-cell receptor gene therapy: Critical parameters for clinical success. J Invest Dermatol. 2011;131:1806–16.
Nawaz W, Xu S, Li Y, Huang B, Wu X, Wu Z. Nanotechnology and immunoengineering: How nanotechnology can boost CAR-T therapy. Acta Biomater. 2020;109:21–36.
Almåsbak H, Aarvak T, Vemuri MC. CAR T cell therapy: a game changer in cancer treatment. J Immunol Res. 2016;2016:10.
Mohanty R, Chowdhury CR, Arega S, Sen P, Ganguly P, Ganguly N. CAR T cell therapy: A new era for cancer treatment (review). Oncol Rep. 2019;42:2183–95.
Chimeric T, Receptor A, Grywalska E, Sosnowska-pasiarska B, Smok-kalwat J. Paving the way toward successful multiple myeloma. Cells. 2020;9:983.
D’Aloia MM, Zizzari IG, Sacchetti B, Pierelli L, Alimandi M. CAR-T cells: the long and winding road to solid tumors review-article. Cell Death Dis. 2018;9:282.
Nam J, Son S, Park KS, Zou W, Shea LD, Moon JJ. Cancer nanomedicine for combination cancer immunotherapy. Nat Rev Mater. 2019;4:398–414.
Garner H, de Visser KE. Immune crosstalk in cancer progression and metastatic spread: a complex conversation. Nat Rev Immunol. 2020;20:483–97.
Muenst S, Läubli H, Soysal SD, Zippelius A, Tzankov A, Hoeller S. The immune system and cancer evasion strategies: Therapeutic concepts. J Intern Med. 2016;279:541–62.
Minutolo NG, Hollander EE, Powell DJJ. The emergence of universal immune receptor t cell therapy for cancer. Front Oncol. 2019;9:176.
Oki Y, Younes A. Heat shock protein-based cancer vaccines. Expert Rev Vaccines. 2004;3:403–11.
Wada S, Yada E, Ohtake J, Sasada T. Personalized peptide vaccines for cancer therapy: Current progress and state of the art. Expert Rev Precis Med Drug Dev. 2017;2:371–81.
Ward S, Casey D, Labarthe MC, Whelan M, Dalgleish A, Pandha H, et al. Immunotherapeutic potential of whole tumour cells. Cancer Immunol Immunother. 2002;51:351–7.
Hirschowitz EA, Mullins A, Prajapati D, Baeker T, Kloecker G, Foody T, et al. Pilot study of 1650-G: A simplified cellular vaccine for lung cancer. J Thorac Oncol. 2011;6:169–73.
Saxena M, Balan S, Roudko V, Bhardwaj N. Towards superior dendritic-cell vaccines for cancer therapy. Nat Biomed Eng. 2018;2:341–4.
Higano CS, Small EJ, Schellhammer P, Yasothan U, Gubernick S, Kirkpatrick P, et al. Sipuleucel-T. Nat Rev Drug Discov. 2010;9:513–4.
Pardi N, Hogan MJ, Porter FW, Weissman D. mRNA vaccines-a new era in vaccinology. Nat Rev Drug Discov. 2018;17:261–79.
Jahanafrooz Z, Baradaran B, Mosafer J, Hashemzaei M, Rezaei T, Mokhtarzadeh A, et al. Comparison of DNA and mRNA vaccines against cancer. Drug Discov Today. 2020;25:552–60.
Zhao Y, Huang L. Lipid nanoparticles for gene delivery. Adv Genet. 2014;88:13–36.
Islam MA, Reesor EKG, Xu Y, Zope HR, Zetter BR, Shi J. Biomaterials for mRNA delivery. Biomater Sci. 2015;3:1519–33.
Hong HS, Koch SD, Scheel B, Gnad-Vogt U, Schröder A, Kallen KJ, et al. Distinct transcriptional changes in non-small cell lung cancer patients associated with multi-antigenic RNActive® CV9201 immunotherapy. Oncoimmunology. 2016;5:e1249560.
Wilhelm S, Tavares AJ, Dai Q, Ohta S, Audet J, Dvorak HF, et al. Analysis of nanoparticle delivery to tumours. Nat Rev Mater. 2016;1:16014.
Jiang W, Von Roemeling CA, Chen Y, Qie Y, Liu X, Chen J, et al. Designing nanomedicine for immuno-oncology. Nat Biomed Eng. 2017;1:1–11.
Irvine DJ, Dane EL. Enhancing cancer immunotherapy with nanomedicine. Nat Rev Immunol. 2020;20:321–34.
Sindhwani S, Syed AM, Ngai J, Kingston BR, Maiorino L, Rothschild J, et al. The entry of nanoparticles into solid tumours. Nat Mater. 2020;19:566–75.
Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17:20–37.
Nakamura T, Harashima H. Integration of nano drug-delivery system with cancer immunotherapy. Ther Deliv. 2017;8:987–1000.
Jovčevska I, Muyldermans S. The therapeutic potential of nanobodies. BioDrugs 2020;34:11–26.
Yang EY, Shah K. Nanobodies: next generation of cancer diagnostics and therapeutics. Front Oncol. 2020;10:1182.
Al-Baradie RS. Nanobodies as versatile tools: a focus on targeted tumor therapy, tumor imaging and diagnostics. Hum Antibodies. 2020;1:1–14.
Barenholz Y. Doxil® - the first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160:117–34.
Kuai R, Ochyl LJ, Bahjat KS, Schwendeman A, Moon JJ. Designer vaccine nanodiscs for personalized cancer immunotherapy. Nat Mater. 2017;16:489–98.
Kuai R, Yuan W, Son S, Nam J, Xu Y, Fan Y, et al. Elimination of established tumors with nanodisc-based combination chemoimmunotherapy. Sci Adv. 2018;4:1–14.
van der Meel R, Sulheim E, Shi Y, Kiessling F, Mulder WJM, Lammers T. Smart cancer nanomedicine. Nat Nanotechnol. 2019;14:1007–17.
Zhang F, Stephan SB, Ene CI, Smith TT, Holland EC, Stephan MT. Nanoparticles that reshape the tumor milieu create a therapeutic window for effective T-cell therapy in solid malignancies. Cancer Res. 2018;78:3718–30.
Liu Z, Jiang W, Nam J, Moon JJ, Kim BYS. Immunomodulating nanomedicine for cancer therapy. Nano Lett. 2018;18:6655–9.
Stephan MT, Moon JJ, Um SH, Bershteyn A, Irvine DJ. Therapeutic cell engineering with surface-conjugated synthetic nanoparticles. Nat Med. 2010;16:1035–41.
Goldberg MS. Improving cancer immunotherapy through nanotechnology. Nat Rev Cancer. 2019;19:587–602.
Fan YN, Li M, Luo YL, Chen Q, Wang L, Zhang HB, et al. Cationic lipid-assisted nanoparticles for delivery of mRNA cancer vaccine. Biomater Sci. 2018;6:3009–18.
Fornaguera C, Guerra-rebollo M, Lázaro MÁ, Castells-sala C, Meca-cortés O, Ramos-pérez V, et al. mRNA delivery system for targeting antigen-presenting cells in vivo. 2018;7:1–11.
Yuan H, Jiang W, Von Roemeling CA, Qie Y, Liu X, Chen Y, et al. Multivalent bi-specific nanobioconjugate engager for targeted cancer immunotherapy. Nat Nanotechnol. 2017;12:763–9.
Bhutani D, Vaishampayan UN. Monoclonal antibodies in oncology therapeutics: Present and future indications. Expert Opin Biol Ther. 2013;13:269–82.
Normanno N, De Luca A, Bianco C, Strizzi L, Mancino M, Maiello MR, et al. Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 2006;366:2–16.
Agustoni F, Suda K, Yu H, Ren S, Rivard CJ, Ellison K, et al. EGFR-directed monoclonal antibodies in combination with chemotherapy for treatment of non-small-cell lung cancer: an updated review of clinical trials and new perspectives in biomarkers analysis. Cancer Treat Rev. 2019;72:15–27.
Pirker R, Pereira JR, Szczesna A, von Pawel J, Krzakowski M, Ramlau R, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet 2009;373:1525–31.
Bertino EM, McMichael EL, Mo X, Trikha P, Davis M, Paul B, et al. A phase I trial to evaluate antibody-dependent cellular cytotoxicity of cetuximab and lenalidomide in advanced colorectal and head and neck cancer. Mol Cancer Ther. 2016;15:2244–50.
Zhou X, Hu W, Qin X. The role of complement in the mechanism of action of rituximab for B‐cell lymphoma: implications for therapy. Oncologist 2008;13:954–66.
Schütze K, Petry K, Hambach J, Schuster N, Albrecht B, Haag F, et al. CD38-specific biparatopic heavy chain antibodies display potent complement-dependent cytotoxicity against multiple myeloma. Cells 2018;9:1–11.
Pereira NA, Chan KF, Lin PC, Song Z. The “less-is-more” in therapeutic antibodies: Afucosylated anti-cancer antibodies with enhanced antibody-dependent cellular cytotoxicity. MAbs 2018;10:693–711.
Linke R, Klein A, Seimetz D. Catumaxomab: clinical development and future directions. MAbs 2010;2:129–36.
Seimetz D. Novel monoclonal antibodies for cancer treatment: the trifunctional an-tibody catumaxomab (Removab®). J Cancer. 2011;2:309–16.
Schmitt M, Schmitt A, Reinhardt P, Thess B, Manfras B, Lindhofer H, et al. Opsonization with a trifunctional bispecific (alphaCD3 x alphaEpCAM) antibody results in efficient lysis in vitro and in vivo of EpCAM positive tumor cells by cytotoxic T lymphocytes. Int J Oncol. 2004;25:841–8.
Buchner A, Riesenberg R, Feicht W, Lindhofer H. Lysis of prostate carcinoma cells by bispecifie antibodies (αEpCAM x αCD3) -visualization by a video incubation system. Eur J Cancer. 2001;37:911–7. SUPPL. 1
Zeidler R, Mysliwietz J, Csánady M, Walz A, Ziegler I, Schmitt B, et al. The Fc-region of a new class of intact bispecific antibody mediates activation of accessory cells and NK cells and induces direct phagocytosis of tumour cells. Br J Cancer. 2000;83:261–6.
Dahlén E, Veitonmäki N, Norlén P. Bispecific antibodies in cancer immunotherapy. Ther Adv Vaccines Immunother 2018;6:3–17.
Brischwein K, Parr L, Pflanz S, Volkland J, Lumsden J, Klinger M, et al. Strictly target cell-dependent activation of T cells by bispecific single-chain antibody constructs of the BiTE class. J Immunother. 2007;30:798–807.
Ph D, Schuh AC, Ribera J, Ph D, Wei A. Blinatumomab versus chemotherapy for advanced acute lymphoblastic. Leukemia 2018;376:836–47.
Gaiser OJ, Piotukh K, Ponnuswamy MN, Planas A, Borriss R, Heinemann U. Structural basis for the substrate specificity of a Bacillus 1,3-1,4-β-glucanase. J Mol Biol. 2006;357:1211–25.
Finkelmeier F, Waidmann O, Trojan J. Nivolumab for the treatment of hepatocellular carcinoma. Expert Rev Anticancer Ther. 2018;18:1169–75.
Xu JX, Maher VE, Zhang L, Tang S, Sridhara R, Ibrahim A, et al. FDA approval summary: nivolumab in advanced renal cell carcinoma after anti‐angiogenic therapy and exploratory predictive biomarker analysis. Oncologist 2017;22:311–7.
Kazandjian D, Suzman DL, Blumenthal G, Mushti S, He K, Libeg M, et al. FDA approval summary: nivolumab for the treatment of metastatic non‐small cell lung cancer with progression on or after platinum‐based chemotherapy. Oncologist 2016;21:634–42.
Kasamon YL, de Claro RA, Wang Y, Shen YL, Farrell AT, Pazdur R. FDA approval summary: nivolumab for the treatment of relapsed or progressive classical Hodgkin lymphoma. Oncologist 2017;22:585–91.
Murakami S. Durvalumab for the treatment of non-small cell lung cancer. Expert Rev Anticancer Ther. 2019;19:1009–16.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gümüş M, Mazières J, et al. Pembrolizumab plus chemotherapy for squamous non–small-cell lung cancer. N. Engl J Med. 2018;379:2040–51.
Bradford D, Demko S, Jin S, Mishra‐Kalyani P, Beckles AR, Goldberg KB, et al. FDA accelerated approval of pembrolizumab for recurrent locally advanced or metastatic merkel cell carcinoma. Oncologist. 2020;25:e1077–82.
Suzman DL, Agrawal S, Ning Y, Maher VE, Fernandes LL, Karuri S, et al. FDA approval summary: atezolizumab or pembrolizumab for the treatment of patients with advanced urothelial carcinoma ineligible for cisplatin‐containing chemotherapy. Oncologist 2019;24:563–9.
Fashoyin‐Aje L, Donoghue M, Chen H, He K, Veeraraghavan J, Goldberg KB, et al. FDA approval summary: pembrolizumab for recurrent locally advanced or metastatic gastric or gastroesophageal junction adenocarcinoma expressing PD‐L1. Oncologist 2019;24:103–9.
Pai‐Scherf L, Blumenthal GM, Li H, Subramaniam S, Mishra‐Kalyani PS, He K, et al. FDA approval summary: pembrolizumab for treatment of metastatic non‐small cell lung cancer: first‐line therapy and beyond. Oncologist 2017;22:1392–9.
Larkins E, Blumenthal GM, Yuan W, He K, Sridhara R, Subramaniam S, et al. FDA approval summary: pembrolizumab for the treatment of recurrent or metastatic head and neck squamous cell carcinoma with disease progression on or after platinum‐containing chemotherapy. Oncologist 2017;22:873–8.
Maly J, Alinari L. Pembrolizumab in classical Hodgkin’s lymphoma. Eur J Haematol. 2016;97:219–27.
Chuk MK, Chang JT, Theoret MR, Sampene E, He K, Weis SL, et al. FDA Approval summary: accelerated approval of pembrolizumab for second-line treatment of metastatic melanoma. Clin Cancer Res. 2017;23:5666–70.
Choi B, McBride A, Scott AJ. Treatment with pembrolizumab after hypersensitivity reaction to nivolumab in a patient with hepatocellular carcinoma. Am J Heal Pharm. 2019;76:1749–52.
Markham A, Duggan S. Cemiplimab: first global approval. 2018;78:1841–6.
Reddy SM, Carroll E, Nanda R. Atezolizumab for the treatment of breast cancer. Expert Rev Anticancer Ther. 2020;20:151–8.
Weinstock C, Khozin S, Suzman D, Zhang L, Tang S, Wahby S, et al. U.S. Food and Drug Administration approval summary: Atezolizumab for metastatic non–small cell lung cancer. Clin Cancer Res. 2017;23:4534–9.
Gaiser MR, Bongiorno M, Brownell I. PD-L1 inhibition with avelumab for metastatic Merkel cell carcinoma. Expert Rev Clin Pharm. 2018;11:345–59.
Rao A, Patel MR. A review of avelumab in locally advanced and metastatic bladder cancer. Ther Adv Urol. 2019;11:175628721882348.
Lavaud P, Hamilou Z, Loriot Y, Massard C. Durvalumab in urothelial cancers. Expert Rev Anticancer Ther. 2018;18:311–8.
Philippidis A. Kymriah. First CAR-T cancer immunotherapy approved by FDA. 2017;4:8.
Bouchkouj N, Kasamon YL, Claro RA De, George B, Lin X, Lee S, et al. FDA Approval summary: axicabtagene ciloleucel for relapsed or refractory large B-cell lymphoma. 2019;25:1702–9.
Rodell CB, Arlauckas SP, Cuccarese MF, Garris CS, Li R, Ahmed MS, et al. TLR7/8-agonist-loaded nanoparticles promote the polarization of tumour-associated macrophages to enhance cancer immunotherapy. 2018;2:578–88.
Cho N, Cheong T, Min JH, Wu JH, Lee SJ, Kim D, et al. A multifunctional core-shell nanoparticle for dendritic cell-based cancer immunotherapy. 2011;6:675–82.
Schloßbauer A, Sauer AM, Cauda V, Schmidt A, Engelke H, Rothbauer U, et al. Cascaded photoinduced drug delivery to cells from multifunctional core-shell mesoporous silica. Adv Health Mater. 2012;1:316–20.
Oberli MA, Reichmuth AM, Dorkin JR, Mitchell MJ, Fenton OS, Jaklenec A, et al. Lipid nanoparticle assisted mRNA delivery for potent cancer immunotherapy. 2017;17:1326–35.
Mi Y, Smith CC, Yang F, Qi Y, Roche KC, Serody JS, et al. A Dual immunotherapy nanoparticle improves T-cell activation and cancer immunotherapy. 2018;1706098:1–9.
Luo M, Wang H, Wang Z, Cai H, Lu Z, Li Y, et al. A STING-activating nanovaccine for cancer immunotherapy. Nat Nanotechnol. 2017;12:648–54.
Acknowledgements
The Support of Agència de Gestió d’Ajuts Universitaris i de Recerca (AGAUR) from Generalitat de Catalunya for their support through SGR 2017 1559 grant is acknowledged. Financial support from Spanish Ministerio de Ciencia, Innovación y Universidades for the grant RTI2018-094734-B-C22. C.G-F would like to thank IQS for her Ph.D. fellowship. S.B. acknowledges Fundació Cellex research grant. Figures were created using biorender.com.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Disclaimer
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Fernández, C., Saz, A., Fornaguera, C. et al. Cancer immunotherapies revisited: state of the art of conventional treatments and next-generation nanomedicines. Cancer Gene Ther 28, 935–946 (2021). https://doi.org/10.1038/s41417-021-00333-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41417-021-00333-5
This article is cited by
-
Magnetic nanoparticles in theranostics of malignant melanoma
EJNMMI Research (2021)