Abstract
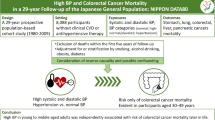
Background
Hypertension and the use of antihypertensive medications have been intensively investigated in relation to colorectal cancer (CRC). Prior epidemiologic studies have not been able to examine this topic with adequate confounding control and follow-up time, or disentangle the effects of antihypertensive agents and hypertension.
Methods
Eligible participants in the Nurses’ Health Study and Health Professionals Follow-up Study were followed for up to 28 years, with repeat assessments of exposures. Cox proportional hazards models were used to estimate hazard ratios and 95% confidence intervals.
Results
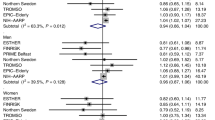
In fully adjusted analyses based on both new-user and prevalent-user designs, there was no association between the use of beta-blockers, calcium-channel blockers, thiazide diuretics, angiotensin-converting enzyme inhibitors, furosemide, other antihypertensive drugs and CRC risk and mortality reached the statistically significant threshold after Bonferroni correction. The results remained similar in sensitivity analyses among participants with hypertension. Before Bonferroni correction, suggestive associations between beta-blocker use and CRC risk and between furosemide use and CRC-specific mortality were observed specifically in analyses using a new-user design. Hypertension was not associated with CRC risk in analyses based on both new-user and prevalent-user designs.
Conclusions
Hypertension and long-term use of major classes of antihypertensive medications are unlikely to be associated with CRC risk and mortality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data described in the manuscript may be made available upon application to and approval by the Channing Division of Network Medicine at Brigham and Women’s Hospital, and Harvard T.H. Chan School of Public Health. Further information, including the procedures to obtain and access data from the Nurses’ Health Study and Health Professionals Follow-up Study, is described at https://www.nurseshealthstudy.org/researchers (email: nhsaccess@channing.harvard.edu) and https://sites.sph.harvard.edu/hpfs/for-collaborators/.
References
Xuan K, Zhao T, Sun C, Patel AS, Liu H, Chen X, et al. The association between hypertension and colorectal cancer: a meta-analysis of observational studies. Eur J Cancer Prev. 2021;30:84–96.
Makar GA, Holmes JH, Yang YX. Angiotensin-converting enzyme inhibitor therapy and colorectal cancer risk. J Natl Cancer Inst. 2014;106:djt374.
Dai YN, Wang JH, Zhu JZ, Lin JQ, Yu CH, Li YM. Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers therapy and colorectal cancer: a systematic review and meta-analysis. Cancer Causes Control. 2015;26:1245–55.
Hicks BM, Filion KB, Yin H, Sakr L, Udell JA, Azoulay L. Angiotensin converting enzyme inhibitors and risk of lung cancer: population based cohort study. BMJ. 2018;363:k4209.
Cronin-Fenton D. Angiotensin converting enzyme inhibitors and lung cancer. BMJ. 2018;363:k4337.
Lever AF, Hole DJ, Gillis CR, McCallum IR, McInnes GT, MacKinnon PL, et al. Do inhibitors of angiotensin-I-converting enzyme protect against risk of cancer? Lancet 1998;352:179–84.
Boudreau DM, Koehler E, Rulyak SJ, Haneuse S, Harrison R, Mandelson MT. Cardiovascular medication use and risk for colorectal cancer. Cancer Epidemiol Biomark Prev. 2008;17:3076–80.
Michels KB, Rosner BA, Walker AM, Stampfer MJ, Manson JE, Colditz GA, et al. Calcium channel blockers, cancer incidence, and cancer mortality in a cohort of U.S. women: the nurses’ health study. Cancer 1998;83:2003–7.
Chen X, Yi CH, Ya KG. Renin-angiotensin system inhibitor use and colorectal cancer risk and mortality: a dose-response meta analysis. J Renin Angiotensin Aldosterone Syst. 2020;21:1470320319895646.
Engineer DR, Burney BO, Hayes TG, Garcia JM. Exposure to ACEI/ARB and beta-blockers is associated with improved survival and decreased tumor progression and hospitalizations in patients with advanced colon cancer. Transl Oncol. 2013;6:539–45.
Bangalore S, Kumar S, Kjeldsen SE, Makani H, Grossman E, Wetterslev J, et al. Antihypertensive drugs and risk of cancer: network meta-analyses and trial sequential analyses of 324,168 participants from randomised trials. Lancet Oncol. 2011;12:65–82.
Bhaskaran K, Douglas I, Evans S, van Staa T, Smeeth L. Angiotensin receptor blockers and risk of cancer: cohort study among people receiving antihypertensive drugs in UK General Practice Research Database. BMJ. 2012;344:e2697.
Sipahi I, Debanne SM, Rowland DY, Simon DI, Fang JC. Angiotensin-receptor blockade and risk of cancer: meta-analysis of randomised controlled trials. Lancet Oncol. 2010;11:627–36.
Jansen L, Weberpals J, Kuiper JG, Vissers PAJ, Wolkewitz M, Hoffmeister M, et al. Pre- and post-diagnostic beta-blocker use and prognosis after colorectal cancer: results from a population-based study. Int J Cancer. 2017;141:62–71.
Jansen L, Below J, Chang-Claude J, Brenner H, Hoffmeister M. Beta blocker use and colorectal cancer risk: population-based case-control study. Cancer 2012;118:3911–9.
Ahl R, Matthiessen P, Sjolin G, Cao Y, Wallin G, Ljungqvist O, et al. Effects of beta-blocker therapy on mortality after elective colon cancer surgery: a Swedish nationwide cohort study. BMJ Open. 2020;10:e036164.
Musselman RP, Bennett S, Li W, Mamdani M, Gomes T, van Walraven C, et al. Association between perioperative beta blocker use and cancer survival following surgical resection. Eur J Surg Oncol. 2018;44:1164–9.
Ahl R, Matthiessen P, Cao Y, Sjolin G, Ljungqvist O, Mohseni S. The relationship between severe complications, beta-blocker therapy and long-term survival following emergency surgery for colon cancer. World J Surg. 2019;43:2527–35.
Hicks BM, Murray LJ, Powe DG, Hughes CM, Cardwell CR. beta-Blocker usage and colorectal cancer mortality: a nested case-control study in the UK Clinical Practice Research Datalink cohort. Ann Oncol. 2013;24:3100–6.
Cui Y, Wen W, Zheng T, Li H, Gao YT, Cai H, et al. Use of Antihypertensive medications and survival rates for breast, colorectal, lung, or stomach cancer. Am J Epidemiol. 2019;188:1512–28.
Grimaldi-Bensouda L, Klungel O, Kurz X, de Groot MC, Maciel Afonso AS, de Bruin ML, et al. Calcium channel blockers and cancer: a risk analysis using the UK Clinical Practice Research Datalink (CPRD). BMJ Open. 2016;6:e009147.
George AJ, Thomas WG, Hannan RD. The renin-angiotensin system and cancer: old dog, new tricks. Nat Rev Cancer. 2010;10:745–59.
Mravec B, Horvathova L, Hunakova L. Neurobiology of cancer: the role of beta-adrenergic receptor signaling in various tumor environments. Int J Mol Sci. 2020;21:7958.
Chin CC, Li JM, Lee KF, Huang YC, Wang KC, Lai HC, et al. Selective beta2-AR blockage suppresses colorectal cancer growth through regulation of EGFR-Akt/ERK1/2 signaling, G1-phase arrest, and apoptosis. J Cell Physiol. 2016;231:459–72.
Mason RP. Calcium channel blockers, apoptosis and cancer: is there a biologic relationship? J Am Coll Cardiol. 1999;34:1857–66.
Janne PA, Mayer RJ. Chemoprevention of colorectal cancer. N Engl J Med. 2000;342:1960–8.
Giovannucci E. Aspirin and delayed chemoprevention of colorectal cancer. Clin Chem. 2018;64:1668–9.
Cuzick J, Otto F, Baron JA, Brown PH, Burn J, Greenwald P, et al. Aspirin and non-steroidal anti-inflammatory drugs for cancer prevention: an international consensus statement. Lancet Oncol. 2009;10:501–7.
Zhang Y, Chan AT, Meyerhardt JA, Giovannucci EL. Timing of aspirin use in colorectal cancer chemoprevention: a prospective cohort study. J Natl Cancer Inst. 2021;113:841–51.
Zhang Y, Wu K, Chan AT, Meyerhardt JA, Giovannucci EL. Long-term statin use, total cholesterol level, and risk of colorectal cancer: a prospective cohort study. Am J Gastroenterol. 2022;117:158–66.
Bibbins-Domingo K. Force USPST. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016;164:836–45.
Belanger CF, Hennekens CH, Rosner B, Speizer FE. The nurses’ health study. Am J Nurs. 1978;78:1039–40.
Harvard School of Public Health. Health professionals follow-up study. https://sites.sph.harvard.edu/hpfs/ (Accessed September 10, 2022).
Yoshida K, Solomon DH, Kim SC. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol. 2015;11:437–41.
Colditz GA, Martin P, Stampfer MJ, Willett WC, Sampson L, Rosner B, et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol. 1986;123:894–900.
Lee DH, Keum N, Giovannucci EL. Colorectal cancer epidemiology in the Nurses’ Health Study. Am J Public Health. 2016;106:1599–607.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16:713–32.
Stampfer MJ, Willett WC, Speizer FE, Dysert DC, Lipnick R, Rosner B, et al. Test of the national death index. Am J Epidemiol. 1984;119:837–9.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Samanic CM, Barbour KE, Liu Y, Fang J, Lu H, Schieb L, et al. Prevalence of self-reported hypertension and antihypertensive medication use among adults—United States, 2017. MMWR Morb Mortal Wkly Rep. 2020;69:393–8.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Song M, Giovannucci EL. Antihypertension and colorectal cancer prevention: getting two birds with one stone. J Natl Cancer Inst. 2014;106:djt438.
Nissen SE. Angiotensin-receptor blockers and cancer: urgent regulatory review needed. Lancet Oncol. 2010;11:605–6.
Cheung KS, Chan EW, Seto WK, Wong ICK, Leung WK. ACE (angiotensin-converting enzyme) inhibitors/angiotensin receptor blockers are associated with lower colorectal cancer risk: a territory-wide study with propensity score analysis. Hypertension 2020;76:968–75.
Brasky TM, Flores KF, Larson JC, Newton AM, Shadyab AH, Watanabe JH, et al. Associations of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with colorectal cancer risk in the Women’s Health Initiative. Cancer Epidemiol Biomarkers Prev. 2021;30:1029–32.
Htoo PT, Sturmer T, Jonsson-Funk M, Pate V, Simpson RJ Jr., Lund JL. Renin-angiotensin-aldosterone system-based antihypertensive agents and the risk of colorectal cancer among medicare beneficiaries. Epidemiology 2019;30:867–75.
Zhu X, Liang J, Shrubsole MJ, Ness RM, Cai Q, Long J, et al. Calcium intake and ion transporter genetic polymorphisms interact in human colorectal neoplasia risk in a 2-phase study. J Nutr. 2014;144:1734–41.
Zhao J, Zhu X, Shrubsole MJ, Ness RM, Hibler EA, Cai Q, et al. Interactions between calcium intake and polymorphisms in genes essential for calcium reabsorption and risk of colorectal neoplasia in a two-phase study. Mol Carcinog. 2017;56:2258–66.
Acknowledgements
The authors thank all participants and staff of the Nurses’ Health Study and Health Professionals Follow-up Study for their contributions to this research. The authors thank the Channing Division of Network Medicine, Brigham and Women’s Hospital and Harvard Medical School for leading the Nurses’ Health Study. The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Central registries may also be supported by state agencies, universities, and cancer centers. Participating central cancer registries include the following: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Maine, Maryland, Michigan, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Seattle SEER Registry, South Carolina, Tennessee, Texas, Utah, Virginia, West Virginia, Wyoming. The authors assume full responsibility for the analyses and interpretation of these data.
Funding
Nurses’ Health Study and Health Professionals Follow-up Study was supported by grants UM1 CA186107, U01 CA176726, P01 CA87969, and U01 CA167552 from the National Institutes of Health (NIH). This work was additionally supported by the American Cancer Society Mentored Research Scholar Grant MRSG-17–220–01-NEC and the NIH grant R00 CA215314 (Dr. Song); NIH grants R01 CA137178, R35 CA253185 (Dr. Chan); and a grant from the World Cancer Research Fund (Dr. Giovannucci). Dr. Zhang is supported by Irene M. & Fredrick J. Stare Nutrition Education Fund Doctoral Scholarship and Mayer Fund Doctoral Scholarship. Dr. Chan is a Stuart and Suzanne Steele MGH Research Scholar. The funding sources played no role in the study design, data collection, data analysis and interpretation of the results, or the decisions made in the preparation and submission of the article.
Author information
Authors and Affiliations
Contributions
Concept and design: YZ, WCW and ELG. Acquisition, analysis or interpretation of the data: YZ. Drafting of the manuscript: YZ. Critical revision of the manuscript for important intellectual content: ELG, WCW, JAM, ATC and MS. Statistical analysis: YZ. Obtained funding: YZ, MS, ATC and ELG. Administrative, technical or material support: ELG and WCW. Supervision: ELG. The authors assume full responsibility for the analyses and interpretation of these data.
Corresponding author
Ethics declarations
Competing interests
Dr. Meyerhardt declares institutional research funding from Boston Biomedical and consulting for Ignyta, Taiho Pharmaceutical, and Cota, outside the submitted work. Dr. Chan declares research funding from Bayer and consulting for Bayer, Pfizer Inc. and Boehringer Ingelheim, outside the submitted work. The remaining authors declare no competing interests.
Ethics approval and consent to participate
The Nurses’ Health Study and Health Professionals Follow-up Study were approved by the Institutional Review Boards of the Brigham and Women’s Hospital and the Harvard T.H. Chan School of Public Health (Boston, MA), and those of participating registries as required. Written informed consent was required to retrieve medical records.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Song, M., Chan, A.T. et al. Long-term use of antihypertensive medications, hypertension and colorectal cancer risk and mortality: a prospective cohort study. Br J Cancer 127, 1974–1982 (2022). https://doi.org/10.1038/s41416-022-01975-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01975-4
This article is cited by
-
Pancreatic cancer is associated with medication changes prior to clinical diagnosis
Nature Communications (2023)