Abstract
Background
Outcomes after metastasectomy for metastatic colorectal cancer (mCRC) vary with RAS and BRAF mutational status, but their effects on resectability and conversion rates have not been extensively studied.
Methods
This substudy of the prospective RAXO trial included 906 patients recruited between 2011 and 2018. We evaluated repeated centralised resectability assessment, conversion/resection rates and overall survival (OS), according to RAS and BRAF status.
Results
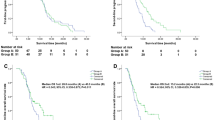
Patients included 289 with RAS and BRAF wild-type (RAS and BRAFwt), 529 with RAS mutated (RASmt) and 88 with BRAF mutated (BRAFmt) mCRC. Metastatic prevalence varied between the RAS and BRAFwt/RASmt/BRAFmt groups, for liver (78%/74%/61%), lung (24%/35%/28%) and peritoneal (15%/15%/32%) metastases, respectively. Upfront resectability (32%/29%/15%), conversion (16%/13%/7%) and resection/local ablative therapy (LAT) rates (45%/37%/17%) varied for RASa and BRAFwt/RASmt/BRAFmt, respectively. Median OS for patients treated with resection/LAT (n = 342) was 83/69/30 months, with 5-year OS-rates of 67%/60%/24%, while systemic therapy-only patients (n = 564) had OS of 29/21/15 months with 5-year OS-rates of 11%/6%/2% in RAS and BRAFwt/RASmt/BRAFmt, respectively. Resection/LAT was associated with improved OS in all subgroups.
Conclusions
There were significant differences in resectability, conversion and resection/LAT rates according to RAS and BRAF status. OS was also significantly longer for RAS and BRAFwt versus either mutant. Patients only receiving systemic therapy had poorer long-term survival, with variation according to molecular status.
Clinical trial registration
NCT01531621/EudraCT2011-003158-24
Similar content being viewed by others
Background
The majority of colorectal cancer (CRC) tumours develop through chromosomal instability and mutations in tumour suppressor genes and oncogenes [1]. RAS oncogene mutations are found in about 50% of CRC tumours with KRAS being the dominant and NRAS less frequent, while BRAF mutations are reported in 5–10% of tumours, with up to 21% reported in cohorts of patients with unresectable metastatic CRC (mCRC) [2, 3].
The RAS and BRAF genes encode proteins that mediate intracellular signalling pathways downstream of the epithelial growth factor receptor (EGFR) [4]. These mutations cause resistance to EGFR therapeutic antibodies and RAS and BRAF testing is now recommended for all patients with mCRC [2, 5,6,7]. BRAF-V600E is the dominant BRAF mutation in CRC, found in more than 90% of patients with a BRAF mutated type (BRAFmt) gene [8]. BRAFmt is associated with higher tumour grade, right-sided primary tumours, female gender, older age, deficient mismatch repair (dMMR) status and higher prevalence of peritoneal and lymph node metastases [4]. RAS mutated type (RASmt) genes have been linked to a higher prevalence of lung metastases [4].
Both RAS and BRAF mutations have been associated with worse survival after resection of CRC liver metastases [9, 10]. For BRAF mutations even the rationale for resecting patients with mCRC has been questioned [11], although some encouraging reports of long-term survival have also been published [12, 13]. Outcomes after metastasectomy vary with RAS and BRAF status, but the significance of these mutations in the setting of multiorgan metastatic disease and resection with curative intent is still unclear.
The aim of this study was to evaluate how RAS and BRAF mutational status affects resectability, conversion and resection rates, differences in metastatic profile and overall survival (OS) after resection and/or local ablative therapy (LAT) and systemic therapy in patients with mCRC.
Methods
Study design
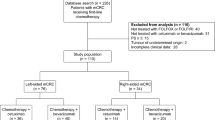
The prospective, investigator-initiated, nationwide Finnish RAXO-study (NCT01531621, EudraCT 2011-003158-24) included 1086 patients with metastatic colorectal cancer recruited from 2012 to 2018 [14, 15]. The oncology departments of all 5 university hospitals and all 16 regional hospitals in Finland participated in the study. Inclusion criteria were patients eligible for first-line systemic therapy, age over 18 years and histologically confirmed colorectal adenocarcinoma with distant metastases or locally advanced primary tumours not curatively treatable. The main protocol has been published in detail [14]. A part of this substudy was presented as a poster and oral presentation at the American Society of Clinical Oncology’s (ASCO) Annual Meeting, 4–8 June 2021 [16].
Patients
Of the whole RAXO-study population, we excluded patients not accurately defined as RAS and BRAF wild-type (RAS and BRAFwt) because of incomplete mutational analysis, i.e. no KRAS, NRAS of BRAF mutation found but all mutations not tested (n = 155), those who received only best supportive care (n = 17) or who had an atypical BRAF (non-V600E) mutation (n = 8). The remaining 906 patients formed the cohort for this substudy that was used to evaluate the secondary aim of prognostic and predictive biomarkers. Computed tomography (CT) for detecting the extent of disease was often done after the diagnostic colonoscopy, and thus even truly synchronous metastases were often detected only shortly after the primary tumour. Because of this, metastases were considered to be synchronous, if they were detected before or within two months of diagnosis of the primary tumour. The data cut-off date for follow-up was 27 March 2020. At that time 609 of the patients (67%) were deceased, mostly due to progressive mCRC.
Molecular pathology
KRAS, NRAS and BRAF-V600E mutations were analysed with reverse transcriptase-polymerase chain reaction (PCR) in 42%, Next-generation sequencing (NGS) in 45%, Idylla panels in 12% and Sanger sequencing and pyrosequencing in 1%, from either histological biopsy or resection specimen from the primary tumour or liver metastasis. The RAS and BRAFwt were tested for KRAS and NRAS exons 2–4 and BRAF-V600E. Of the RASmt patients 294 were not analysed but assumed BRAFwt as the coexistence of RAS and BRAF mutations was considered very rare [4]. Immunohistochemistry with primary antibodies for MLH1, MSH2, MSH6 and PMS2 proteins was used to identify deficient mismatch repair status, and PCR was used when the results of immunohistochemistry were indeterminate.
Systemic therapy
Standard local treatment protocols based on ESMO [5] and NCCN [6, 7] guidelines were used for systemic therapy, which was given until disease progression, unacceptable toxicity or resection/LAT was achieved. In the perioperative setting mainly oxaliplatin and fluoropyrimidine-based treatment regimens were used [17]. For conversion chemotherapy the most intensive regimen was used, preferably a doublet or triplet chemotherapy combined with a targeted agent (bevacizumab, cetuximab or panitumumab) based on RAS and BRAF status [5].
Resectability assessment
The first local resectability assessment was done at the local hospital before starting first-line treatment, often before recruitment to the RAXO-study. After study inclusion, baseline demographics were provided online and the multidisciplinary team (MDT) at Helsinki University Hospital tertiary centre evaluated the technical resectability of the liver, lung and other metastases based on imaging. The imaging examinations included whole body (chest, abdomen and pelvis) CT supplemented by magnetic resonance imaging and 18F-fluoro-deoxyglucose positron emission tomography (PET) as needed. The MDT consisted of experts in liver surgery and abdominal radiology with medical oncologists, radiation oncologists, colorectal and cytoreductive surgeons, thoracic surgeons, gynaecologists, thoracic radiologists and PET specialists, as required. The MDT assessment was performed on baseline radiology (when the metastatic disease was noted) and repeated twice, if needed, after 2–3 and 4–6 months of systemic therapy and provided electronically to the treating physicians. The treatment decisions were made by local or central MDTs and resections were mostly carried out at specialised centres at the six largest hospitals.
Statistical analysis
For differences in demographics and other nominal factors, Bonferroni correction for Chi-square analyses per variable was applied. For variables with significant differences logistic regression was used to calculate odds ratios (OR) with 95% confidence intervals (95% CI). The Kaplan–Meier method was used to estimate OS, which was calculated from the diagnosis of metastatic disease to the date of death or censored at the last follow-up. Conditional 12-month Landmark analysis of OS was used to control a potential guarantee-time bias as reported previously [15]. Hazard ratios (HR) and corresponding 95% CI for survival were calculated using Cox proportional hazard regression. Univariate analyses were first performed and variables with significant HR were then entered into the multivariable analysis. The study had 609 OS events which allowed for several covariates in multivariable analysis. The median follow-up time was calculated with the reverse Kaplan–Meier method. All analyses were carried out using SPSS Statistics, Version 25.0, Armonk, NY.
Results
The molecular substudy included 906 patients, of which 289 were RAS and BRAFwt (32%), 529 were RASmt (58%) and 88 were BRAF-V600Emt (10%). KRASmt (n = 491, 54%) and NRASmt (n = 38, 4%) patients were analysed as one group (RASmt). Mismatch repair status was examined in 294 patients, 12 of whom had dMMR (4%), including 2 RAS and BRAFwt, 5 RASmt and 5 BRAFmt. The median follow-up time was 55 months, with a minimum follow-up of 18 months.
The median age of the treatable patients was 66 years. Demographics (Table 1) showed that BRAFmt tumours were more common among women (OR 3.3) and in ECOG performance status 2–3 patients (OR 1.5) with RAS and BRAFwt as reference (ref) in all analyses. Primaries with BRAFmt were predominantly right-sided (OR 11.8), whereas RAS and BRAFwt tumours were mostly left-sided (either colon or rectum), and RASmt patients’ tumours were in between (OR 2.3). Tumours with BRAFmt had more often signet cell or mucinous histology (OR 4.2), and this was also more likely for RASmt tumours (OR 1.7) than for RAS and BRAFwt. RASmt patients received adjuvant therapy after resection of the primary tumour less often than RAS and BRAFwt (OR 0.7). No differences were noted in Charlson comorbidity index, low body mass index (BMI), surgery of the primary tumour or synchronous presentation.
The metastatic profiles at baseline, when mCRC was diagnosed, were different according to mutational status (Table 1, Fig. 1). Liver metastases were less common for BRAFmt (OR 0.5) than RAS and BRAFwt patients. RASmt patients were more likely to have lung metastases than RAS and BRAFwt (OR 1.7). Peritoneal metastases were more common in BRAFmt (OR 2.7) than for RAS and BRAFwt (ref) or RASmt (OR 1.0) patients. No differences were observed for distant lymph node metastases, for other metastatic sites or for the number of metastatic sites.
The liver was the most common metastatic site at the time of diagnosis of metastatic disease as well as throughout the disease trajectory (Fig. 1). Liver metastases during disease trajectory were more likely for RAS and BRAFwt (82%, ref) and RASmt (80%, OR 1.1 [95% CI 0.8–1.6]) compared with BRAFmt patients (69%, 0.6 [0.3–0.9]). Lung metastases during disease trajectory were more common for RASmt (61%, 2.0 [1.5–2.7]) than for RAS and BRAFwt (44%, ref) with BRAFmt patients in between (50%, 1.3[0.8–2.1]). Peritoneal metastases during trajectory were more common among BRAFmt (43%, 2.4 [1.4–3.9]) and less common among RASmt (26%, 1.1 [0.7–1.5]), and RAS and BRAFwt patients (24%, ref). There were no significant differences in the prevalence of lymph node, bone, ovarian, suprarenal or brain metastases, and local relapse between the molecular subtypes. Bone, brain and suprarenal metastases were more likely to appear later during the disease (Fig. 2).
The likelihood of upfront resectability of all metastatic sites in central assessment (Fig. 3) was lower for BRAFmt (15%, OR 0.3 [0.2–0.6]) than for RASmt (29%, OR 0.8 [0.6–1.1]) or RAS and BRAFwt (32%, ref). For borderline resectable, conversion to resectable with systemic therapy was higher for RAS and BRAFwt (23%, ref) and RASmt (19%, OR 0.8 [0.5–1.2]) than for BRAFmt (8%, OR 0.3 [0.1–0.7]). The overall resectability rates (including conversion) were higher for RAS and BRAFwt (48%, ref) and RASmt (43%, OR 0.8 [0.6–1.1]) than for BRAFmt (22%, OR 0.3 [0.2–0.5])
There were differences in upfront resectability assessment between centralised tertiary MDT and local evaluation (Fig. 4). The discrepancy was highest in patients centrally classified as upfront resectable. The underestimation of upfront resectability was 47% for RAS and BRAFwt, 40% for RASmt and 69% for BRAFmt. When the central assessment was borderline resectable, the local assessment was concordant in 57–85% of cases, but even then, up to 25% of patients were locally considered completely unresectable.
In total, 342 (38% of 906) patients were resected and/or treated with LAT. Resection and/or LAT rates were highest for RAS and BRAFwt (45%, ref), slightly lower for RASmt (37%, OR 0.7 [0.5–1.0]) and lowest for BRAFmt (17%, OR 0.2 [0.1–0.5]).
Patients with RAS and BRAFwt tumours had the longest mOS after the diagnosis of metastatic disease of 83 months with a 5-year OS-rate of 67% in resected and/or LAT treated and RASmt patients had a mOS of 69 months, with a 5-year OS-rate of 60% (HR 1.53 [95% CI 1.04–1.76], Fig. 5). BRAFmt patients had a shorter mOS of 30 months with a 5-year OS-rate of 24% with resection and/or LAT (HR 3.11 [95% CI 1.49–6.49] vs RAS and BRAFwt).
At mCRC diagnosis 46–48% of patients presented with multiple metastatic sites (2–6 sites) with no differences between mutational groups. The resected and/or LAT patients had a better OS than those not resected (Supplementary Fig. 1). Only two BRAFmt patients with multiple metastatic sites were resected.
OS in “systemic therapy only” patients (n = 564, 62%) was longest for RAS and BRAFwt (29 months), intermediate for RASmt (21 months) and shortest for BRAFmt (15 months). The 5-year OS-rates were 11%, 6% and 2%, respectively (Fig. 5). Patients who only received systemic therapy had worse survival than resected and/or LAT patients in all the mutational groups (Supplementary Fig. 2). Similar results were also seen in a 12-month conditional Landmark analysis of OS for RAS and BRAFwt and RASmt (Supplementary Fig. 3).
Prognostic baseline factors for OS in univariate analyses are presented in (Supplementary Table 1). In univariate analysis HR for OS for right-sided primary tumour (others as reference) was 1.82 (95% CI 1.24–2.67) for RAS and BRAFwt, 1.25 (1.00–1.55) for RASmt and 1.14 (0.70–1.85) for BRAFmt. In the multivariable analysis of prognostic factors for OS (Supplementary Table 1) metastasectomy and/or LAT was the strongest factor associated with survival (HR 0.24). The second most notable factor was the mutational status with BRAFmt (HR 2.39) and RASmt (HR 1.54). Poor ECOG performance status, right-sided primary tumour and presence of baseline liver, peritoneal or suprarenal metastases were also associated with impaired OS.
Discussion
Based on the repeated centralised assessment of resectability of multisite metastases [14, 15], this study demonstrated high upfront resectability (32% vs 29% vs 15%), conversion (23% vs 19% vs 8%) and resection/LAT (45% vs 37% vs 17%) rates in our real-world clinical material, in RAS and BRAFwt, RASmt and BRAFmt patients, respectively. These figures were highly dependent on mutational status. Upfront resectability rates are rarely reported in the literature, see review in ref. [14], and to the best of our knowledge upfront resectability by mutational status has not previously been reported for non-selected mCRC patients.
In mCRC study populations RASwt rates have been reported to be in the range of 40–54% [2, 18], slightly higher than the rate observed in this study, excluding patients who were not accurately RASwt. In contrast, the RASmt rates observed in our study were higher than those previously presented in the literature at 40–51% [2, 18]. In population-based series of unresectable patients, BRAFmt rates of 21% have been noted. We observed a BRAFmt rate of 10%, a number which is more in line with the rates observed in study populations of 5–10% [2, 3].
The SEER database shows that the liver is the most common site for CRC metastases (74%), followed by the lung (22%) [19], figures well in line with our data. However, no data according to molecular status is presented in that study [19]. KRAS mutations are associated with a higher prevalence and a more aggressive form of lung metastases [20], the former also supported by our data. Also, BRAFmt patients have more peritoneal and lymph node metastases but fewer liver and lung metastases than BRAFwt [3, 21], in line with our peritoneal metastasis findings. In a large Swedish national mCRC cohort, tumours with mucinous or signet cell histology have more peritoneal and fewer liver metastases, but the mutational status was not reported [22]. BRAFmt associates with this histology in our material, which could at least partially explain the Swedish findings.
Folprecht reported that response rates for combination chemotherapy correlated with conversion rates, and later verified “the higher the response, the better the conversion rate” for the addition of cetuximab to combination chemotherapy in KRASwt disease [23, 24]. In the TRIBE-study of combination chemotherapy with bevacizumab, response rates and OS varied according to RAS and BRAF status, but conversion rates according to RAS and BRAF status were not reported [25]. Studies of triplet chemotherapy plus biologics for the treatment of borderline resectable patients have noted high response (81–87%) and conversion (33–61%) rates for liver-limited patients treated with triplet chemotherapy plus bevacizumab [26], or panitumumab [27]. In a study that used hepatic arterial infusion for unresectable CRC liver metastases. Datta et al. reported conversion rates of 45% in RAS and BRAFwt ± TP53mt, 45% in RASmt + TP53wt, 39% in RASmt + TP53mt, and no conversions for BRAFmt patients [28]. Further, a conversion rate of 22% for RASwt was observed in the FIRE-3 trial [29]. In a Scandinavian population-based study conversion and resection rates of 11% in KRAS and BRAFwt, 8% in KRASmt and only 1% in BRAFmt were reported [3]. Taken together, these results correspond well with our observation that the highest conversion rates were seen in RAS and BRAFwt, were almost as high in RASmt and were clearly lower in BRAFmt, with the caveat of inclusion of multiple and multisite metastases in our real-world study.
The aforementioned publications that refer to resection rates for molecular subtypes mostly focus on initially unresectable or borderline diseases. We are not aware of other population-based series that report total resectability rates for all treatable mCRC patients according to RAS and BRAF status. Recently, a retrospective series of liver metastases noted a 34% resection/LAT rate in treated BRAFmt patients [30].
In addition to our RAXO group [14, 15], central resectability assessment for CRC liver metastases has been described by Huiskens [31], and for mCRC by Modest [32]. Both of these studies reported a high level of disagreement in evaluation, supporting the use of specialised MDT assessment without segregation for mutational status. When comparing central and local assessments of upfront resectability in our study, there were considerable discrepancies of 40–47% in RAS and BRAFwt and RASmt, but as high as 69% in BRAFmt. BRAFmt patients in our study as in the literature [3], had poorer ECOG performance status and a metastatic profile more difficult for resection. Therefore, local pessimism is understandable, but undesirable as there were patients in this group who derived long-term benefits from resection. The repeated central assessment of technical resectability was performed without knowledge of mutational status, which probably partly explains this discrepancy in BRAFmt. The implications of a discrepancy between the central and local review of resectability status need to be addressed separately in each country. Resectability should repeatedly be addressed in organ-specific MDTs with significant experience in conversion treatments and challenging resections and/or LATs.
Outcome after resection and/or LAT in this study was excellent for RAS and BRAFwt (OS of 83 months) and very good for RASmt (60 months), while it was modest for BRAFmt (30 months). In a review from Tsilimiras [33], 24 liver resection studies reported RASmt as a negative prognostic factor for OS, in line with our study including all metastatic sites, whereas four studies found no effect of RAS status on OS. In these studies, OS was over 70 months for RASwt and 20–51 months for RASmt, somewhat shorter than in our study. Twelve studies included in the review reported impaired outcomes for patients with BRAFmt, in line with our findings. Also, a meta-analysis of 11 prospective and retrospective studies of liver resection reported that KRASmt and BRAFmt mutational status was negatively associated with OS and relapse-free survival (RFS) [9]. Also, a recent retrospective real-world study from US reported worse survival for BRAFmt mCRC patients compared to BRAFwt [34]. The worse outcome in RASmt and BRAFmt is probably due to both the mutations and right-sided primary according to multivariable analysis. Sidedness affects metastatic profile, with less resectable metastatic sites in BRAFmt. In univariate analysis there was no significant OS difference for BRAFmt with right versus left-sided primaries. Despite the worse prognosis, long-term survival without relapse is still possible for BRAFmt after liver resection [13], and longer OS in BRAFmt is observed after resection than with systemic therapy only [30].
Patients with RASmt or BRAFmt and synchronous CRC liver metastases have worse survival after resection than patients with wild-type tumours, but this difference is not observed in the case of metachronous metastases [35]. This may describe the more indolent nature of the metachronous disease and could be one factor favouring the decision to perform a resection. In a retrospective analysis of patients treated with any metastasectomy, RASmt and the presence of liver metastases were the only independent risk factors of the impaired OS with a 4-year OS-rate of 81% for RASwt versus 60% for RASmt [36]. This is in line with our multivariate findings for RAS and BRAF status and liver metastases, but not for synchronous presentation.
Lung metastases themselves may not present the decisive factor for survival, and the role of pulmonary metastasectomy is not fully clear based on the PulMiCC study [37]. As a part of complete clearance of the disease, lung resection provides a possible cure in mCRC, as is also noted in the ESMO guidelines [5]. A recent meta-analysis in pulmonary resection reported impaired OS and RFS for RASmt versus RASwt patients, and similarly BRAFmt patients had worse survival than BRAFwt [20]. This is well in line with our findings and a favourable molecular profile could provide support for the decision of whether or not to perform lung resection.
Some studies have identified RASmt as a negative prognostic marker after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal metastasectomy [38], but a recent Norwegian study found a similar OS of around 49 months after cytoreductive surgery with HIPEC irrespective of RAS and BRAF status [39]. In the latter study a BRAFmt subgroup with dMMR had superior survival among the patients with BRAFmt and this has also been reported in an unselected CRC cohort [40]. In line with these findings, we observed impaired survival for BRAFmt patients with peritoneal metastases, with the caveat that our study only included small patient numbers in this group. In addition, we had MMR analysis available from a fraction of the patients and therefore cannot compare these results.
The major strength of this study is the analysis of a complete set of data from 906 prospective real-world mCRC patients that were all considered treatable and, thus, the results are applicable to our everyday practice. Secondly, molecular pathology was mostly assessed as part of the clinical routine with accredited methods thus optimising systemic treatment choices regarding chemotherapy and biologics. Third, a repeated central assessment of resectability was performed at a tertiary centre maximising resectability, conversion and resection rate analyses. Fourth, central assessments were performed without knowledge of molecular status, making bias due to pre-knowledge of the potentially negative prognosis of BRAF and RAS mutants unlikely. Fifth, we included all metastatic sites in the resectability assessment and recorded sites and resections throughout the disease trajectory.
A clear limitation of this study is the observational design without any randomisation. Secondly, we had only 15 resected BRAFmt patients making confidence intervals wide. Given the often more widespread and aggressive nature of BRAFmt mCRC, this will be a problem in all prospective studies comparing different molecular subtypes. One way of overcoming this is conducting BRAFmt only studies such as the BEACON-study [41], although that specific study only concentrated on unresectable diseases. Large collaborative registries for BRAFmt would be of uttermost importance in overcoming this limitation. Third, MMR status was missing for 68% of patients, as testing was not recommended until the ESMO recommendations were updated in 2016 [5]. Fourth, all but the liver resection subgroups were quite small for robust comparisons. Fifth, we cannot currently provide accurate enough systemic treatment information per RAS/BRAF group. We are collecting later line treatment information and validating the correct use of biologics in the entire cohort of treatable patients.
In conclusion, there were significant differences in metastatic profile, resectability, conversion and resection/LAT rates according to RAS and BRAF status. Repeated centralised MDT assessment gives all patients an optimal chance for the best possible treatment. Outcomes for patients with multisite and multiple metastases were significantly better for RAS and BRAF wild-type compared with either mutant. Even BRAFmt patients have a chance of long-term survival with resection. Patients only receiving systemic therapy still have poorer long-term survival than resected patients, similarly, varying according to molecular status.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data collected for this study can be made available to others in de-identified form after all primary and secondary endpoints have been published, in the presence of a data transfer agreement and if the purpose of use complies with Finnish legislation. Requests for data sharing can be made to the last author, including a proposal that must be approved by the steering committee.
References
Harada S, Morlote D. Molecular pathology of colorectal cancer. Adv Anat Pathol. 2020;27:20–26.
Modest DP, Ricard I, Heinemann V, Hegewisch-Becker S, Schmiegel W, Porschen R, et al. Outcome according to KRAS-, NRAS- and BRAF-mutation as well as KRAS mutation variants: pooled analysis of five randomized trials in metastatic colorectal cancer by the AIO colorectal cancer study group. Ann Oncol. 2016;27:1746–53.
Sorbye H, Dragomir A, Sundstrom M, Pfeiffer P, Thunberg U, Bergfors M, et al. High BRAF mutation frequency and marked survival differences in subgroups according to KRAS/BRAF mutation status and tumor tissue availability in a prospective population-based metastatic colorectal cancer cohort. PLoS ONE. 2015;10:e0131046.
Custodio A, Feliu J. Prognostic and predictive biomarkers for epidermal growth factor receptor-targeted therapy in colorectal cancer: beyond KRAS mutations. Crit Rev Oncol Hematol. 2013;85:45–81.
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386–422.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. Colon cancer, version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19:329–59.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. Rectal cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. 2021. https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf.
Rosati G, Aprile G, Basile D, Avallone A. Perspectives in the treatment of RAS or BRAF mutated metastatic colorectal cancer patients. Front Oncol. 2021;11:602596.
Tosi F, Magni E, Amatu A, Mauri G, Bencardino K, Truini M, et al. Effect of KRAS and BRAF mutations on survival of metastatic colorectal cancer after liver resection: a systematic review and meta-analysis. Clin Colorectal Cancer. 2017;16:e153–e163.
Margonis GA, Buettner S, Andreatos N, Kim Y, Wagner D, Sasaki K, et al. Association of BRAF mutations with survival and recurrence in surgically treated patients with metastatic colorectal liver cancer. JAMA Surg. 2018;153:e180996.
Pikoulis E, Margonis GA, Andreatos N, Sasaki K, Angelou A, Polychronidis G, et al. Prognostic role of BRAF mutations in colorectal cancer liver metastases. Anticancer Res. 2016;36:4805–11.
Bachet JB, Moreno-Lopez N, Vigano L, Marchese U, Gelli M, Raoux L, et al. BRAF mutation is not associated with an increased risk of recurrence in patients undergoing resection of colorectal liver metastases. Br J Surg. 2019;106:1237–47.
Gagniere J, Dupre A, Gholami SS, Pezet D, Boerner T, Gonen M, et al. Is hepatectomy justified for BRAF mutant colorectal liver metastases?: A multi-institutional analysis of 1497 patients. Ann Surg. 2020;271:147–54.
Osterlund P, Salminen T, Soveri LM, Kallio R, Kellokumpu I, Lamminmaki A, et al. Repeated centralized multidisciplinary team assessment of resectability, clinical behavior, and outcomes in 1086 Finnish metastatic colorectal cancer patients (RAXO): a nationwide prospective intervention study. Lancet Reg Health Eur. 2021;3:100049.
Isoniemi H, Uutela A, Nordin A, Lantto E, Kellokumpu I, Ovissi A, et al. Centralized repeated resectability assessment of patients with colorectal liver metastases during first-line treatment: prospective study. Br J Surg. 2021. https://doi.org/10.1093/bjs/znaa145.
Osterlund PJ, Osterlund E, Uutela A, Halonen P, Kallio RS, Ålgars A, et al. Resectability, conversion and resections rates, and outcomes in RAS&BRAF wildtype (wt), RAS mutant (mt) and BRAFmt metastatic colorectal cancer (mCRC) subgroups in the prospective Finnish RAXO-study. J Clin Oncol. 2021;39:3532–3532.
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14:1208–15.
Loupakis F, Moretto R, Aprile G, Muntoni M, Cremolini C, Iacono D, et al. Clinico-pathological nomogram for predicting BRAF mutational status of metastatic colorectal cancer. Br J Cancer. 2016;114:30–36.
Wang J, Li S, Liu Y, Zhang C, Li H, Lai B. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: A population-based analysis. Cancer Med. 2020;9:361–73.
Huang J, Zang Q, Wen Y, Pan Z, Yao Z, Huang M, et al. Prognostic value of KRAS mutation in patients undergoing pulmonary metastasectomy for colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2021;160:103308.
Nakayama I, Hirota T, Shinozaki E. BRAF mutation in colorectal cancers: from prognostic marker to targetable mutation. Cancers (Basel). 2020;12:3236.
Riihimaki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6:29765.
Folprecht G, Grothey A, Alberts S, Raab HR, Kohne CH. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol. 2005;16:1311–9.
Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Cremolini C, Loupakis F, Antoniotti C, Lupi C, Sensi E, Lonardi S, et al. FOLFOXIRI plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 TRIBE study. Lancet Oncol. 2015;16:1306–15.
Gruenberger T, Bridgewater J, Chau I, Garcia Alfonso P, Rivoire M, Mudan S, et al. Bevacizumab plus mFOLFOX-6 or FOLFOXIRI in patients with initially unresectable liver metastases from colorectal cancer: the OLIVIA multinational randomised phase II trial. Ann Oncol. 2015;26:702–8.
Modest DP, Martens UM, Riera-Knorrenschild J, Greeve J, Florschutz A, Wessendorf S, et al. FOLFOXIRI plus panitumumab as first-line treatment of RAS wild-type metastatic colorectal cancer: the randomized, open-label, phase II VOLFI study (AIO KRK0109). J Clin Oncol. 2019;37:3401–11.
Datta J, Narayan RR, Goldman DA, Chatila WK, Gonen M, Strong J, et al. Distinct genomic profiles are associated with conversion to resection and survival in patients with initially unresectable colorectal liver metastases treated with systemic and hepatic artery chemotherapy. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000004613
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Kaiser F, Al-Batran SE, et al. FOLFIRI plus cetuximab or bevacizumab for advanced colorectal cancer: final survival and per-protocol analysis of FIRE-3, a randomised clinical trial. Br J Cancer. 2021;124:587–94.
Ye LF, Ji XM, Ren C, Wang ZQ, Lin CP, Chen DL, et al. The prognostic value of locoregional interventions for BRAF V600E metastatic colorectal cancer: a retrospective cohort analysis. Biomolecules. 2021;11:1268.
Huiskens J, Bolhuis K, Engelbrecht MR, De Jong KP, Kazemier G, Liem MS, et al. Outcomes of resectability assessment of the dutch colorectal cancer group liver metastases expert panel. J Am Coll Surg. 2019;229:523–32 e522.
Modest DP, Denecke T, Pratschke J, Ricard I, Lang H, Bemelmans M, et al. Surgical treatment options following chemotherapy plus cetuximab or bevacizumab in metastatic colorectal cancer-central evaluation of FIRE-3. Eur J Cancer. 2018;88:77–86.
Tsilimigras DI, Ntanasis-Stathopoulos I, Bagante F, Moris D, Cloyd J, Spartalis E, et al. Clinical significance and prognostic relevance of KRAS, BRAF, PI3K and TP53 genetic mutation analysis for resectable and unresectable colorectal liver metastases: a systematic review of the current evidence. Surg Oncol. 2018;27:280–8.
Trunk A, Braithwaite M, Nevala-Plagemann C, Pappas L, Haaland B, Garrido-Laguna I. Real-world outcomes of patients with BRAF-mutated metastatic colorectal cancer treated in the United States. J Natl Compr Canc Netw. 2022;20:144–50.
Huang CJ, Teng HW, Chien CC, Lin JK, Yang SH. Prognostic significance of C-reactive protein polymorphism and KRAS/BRAF in synchronous liver metastasis from colorectal cancer. PLoS ONE. 2014;8:e65117.
Osumi H, Shinozaki E, Suenaga M, Matsusaka S, Konishi T, Akiyoshi T, et al. RAS mutation is a prognostic biomarker in colorectal cancer patients with metastasectomy. Int J Cancer. 2016;139:803–11.
Milosevic M, Edwards J, Tsang D, Dunning J, Shackcloth M, Batchelor T, et al. Pulmonary Metastasectomy in Colorectal Cancer: updated analysis of 93 randomized patients—control survival is much better than previously assumed. Colorectal Dis. 2020;22:1314–24.
Arjona-Sanchez A, Rodriguez-Ortiz L, Baratti D, Schneider MA, Gutierrez-Calvo A, Garcia-Fadrique A, et al. RAS mutation decreases overall survival after optimal cytoreductive surgery and hyperthermic intraperitoneal chemotherapy of colorectal peritoneal metastasis: a modification proposal of the peritoneal surface disease severity score. Ann Surg Oncol. 2019;26:2595–604.
Larsen SG, Goscinski MA, Dueland S, Steigen SE, Hofsli E, Torgunrud A, et al. Impact of KRAS, BRAF and microsatellite instability status after cytoreductive surgery and HIPEC in a national cohort of colorectal peritoneal metastasis patients. Br J Cancer. 2021. https://doi.org/10.1038/s41416-021-01620-6.
Seppala TT, Bohm JP, Friman M, Lahtinen L, Vayrynen VM, Liipo TK, et al. Combination of microsatellite instability and BRAF mutation status for subtyping colorectal cancer. Br J Cancer. 2015;112:1966–75.
Kopetz S, Grothey A, Yaeger R, Van Cutsem E, Desai J, Yoshino T, et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N Engl J Med. 2019;381:1632–43.
Acknowledgements
We wish to thank the patients and their families, the investigators, study personnel and the hospitals that have participated in this study. We acknowledge Celina Österlund for preparation of figures and the medical writers at Meducom BV, Wilko Coers, PhD and Sandy Field, PhD, for English language editing of the manuscript. CÖ, WC and SF were compensated for their support by the last author. This work was presented in part at the American Society of Clinical Oncology’s (ASCO) Annual Meeting 4–8th June 2021 [16].
Funding
This investigator-initiated RAXO-study was supported by Finska Läkaresällskapet (2016, 2018, 2019, 2020, 2021, 2022); Cancer Foundation Finland (2019–2020, 2021, 2022–2023; Relander’s Foundation (2020–2022); the Competitive State Research Financing of the Expert Responsibility Area of Tampere, Helsinki and Turku (2016, 2017, 2018, 2019, 2020, 2021, 2022); Tampere University Hospital Funds (Tukisäätiö 2019, 2020; OOO 2020); and the Research Fund of Helsinki University Hospital (2019, 2020, 2021). The infrastructure with database and study nurses were partly supported by pharmaceutical companies (Amgen unrestricted grant 2012–2020, Eli Lilly 2012–2017, Merck KGaA 2012–2020, Roche Oy 2012–2020, Sanofi 2012–2017 and Servier unrestricted grant 2016–2020). The funders had no role in the study design, analysis, interpretation of the data, decision to publish or writing of this report. Open Access funding provided by University of Helsinki including Helsinki University Central Hospital.
Author information
Authors and Affiliations
Contributions
AU, EO, HI and PO wrote the original manuscript. All authors interpreted the data and were involved in the review and writing of the manuscript. PO, HI, LMS, PH, TS, AÅ, RR, EH, RK, AML and KL comprised the RAXO steering committee and participated in all phases of the study, including the design or conduct of the study, analyses and interpretation of the data and preparation of the manuscript. All authors recruited patients or gathered data for the study. AU and PO performed the statistical analyses supervised by statistician Tuija Poussa.
Corresponding author
Ethics declarations
Competing interests
All authors report institutional research funding from Eli Lilly, Merck KGaA, Roche Oy, Sanofi and unrestricted grants from Amgen and Servier, during the conduct of the study. AU, EO, PH, RK, AÅ, TS, AL, LMS, RR, KL, HS, EH, TM, JK, AN, AO, AK, MK, JS, LN, MM, TK, AR, HI and PO report grants, personal fees or non-financial support from Abbvie, Amgen, Astra-Zeneca, Baxalta/Shire, Bayer, BMS, Celgene, Eisai/Ewopharma, Eli Lilly, Erythech Pharma, Fresenius, Incyte, Jansen-Cilag, Medicom, Merck, MSD, Nordic Drugs/Pharma, Novartis, Nutricia/Danone, Pierre-Fabre, Roche Oy, Sanofi, Servier, Sobi and/or Varian.
Ethics approval and consent to participate
This study was conducted in accordance with the declaration of Helsinki and monitored independently. The study protocol was approved by the Ethics Committee at Helsinki University Hospital (242/13/03/02/2011 and HUS/1288/2016) and all patients provided written informed consent.
Consent for publication
All authors had full access to the data and had final responsibility for the decision to submit for publication, and all authors have accepted the manuscript and the decision to submit it for publication. No individual patients can be recognised in the publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A full list of the RAXO Study Group members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uutela, A., Osterlund, E., Halonen, P. et al. Resectability, conversion, metastasectomy and outcome according to RAS and BRAF status for metastatic colorectal cancer in the prospective RAXO study. Br J Cancer 127, 686–694 (2022). https://doi.org/10.1038/s41416-022-01858-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01858-8
This article is cited by
-
BRAFV600E Metastatic Colorectal Cancer: Perspective from a Patient, a Caregiver, and an Oncologist
Advances in Therapy (2023)