Abstract
Background
Treatment of patients with residual disease after neoadjuvant chemotherapy for breast cancer is an unmet clinical need. We hypothesised that tumour subclones showing expansion in residual disease after chemotherapy would contain mutations conferring drug resistance.
Methods
We studied oestrogen receptor and/or progesterone receptor-positive, HER2-negative tumours from 42 patients in the EORTC 10994/BIG 00-01 trial who failed to achieve a pathological complete response. Genes commonly mutated in breast cancer were sequenced in pre and post-treatment samples.
Results
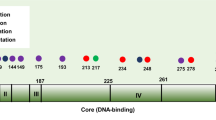
Oncogenic driver mutations were commonest in PIK3CA (38% of tumours), GATA3 (29%), CDH1 (17%), TP53 (17%) and CBFB (12%); and amplification was commonest for CCND1 (26% of tumours) and FGFR1 (26%). The variant allele fraction frequently changed after treatment, indicating that subclones had expanded and contracted, but there were changes in both directions for all of the commonly mutated genes.
Conclusions
We found no evidence that expansion of clones containing recurrent oncogenic driver mutations is responsible for resistance to neoadjuvant chemotherapy. The persistence of classic oncogenic mutations in pathways for which targeted therapies are now available highlights their importance as drug targets in patients who have failed chemotherapy but provides no support for a direct role of driver oncogenes in resistance to chemotherapy.
ClinicalTrials.gov
EORTC 10994/BIG 1-00 Trial registration number NCT00017095.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Clinical data can be accessed through the EORTC data-sharing platform (for details, see www.eortc.org/data-sharing). NGS data can be accessed through the European Genome-Phenome Archive (https://www.ebi.ac.uk/ega/, cram files EGAD00001003334, study accession number EGAS00001001223). The NGS data are only accessible under a Managed Access Agreement (for details, see www.ebi.ac.uk/ega/dacs).
Code availability
Code is available on request to AC or RI.
References
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Bonnefoi H, Litiere S, Piccart M, MacGrogan G, Fumoleau P, Brain E, et al. Pathological complete response after neoadjuvant chemotherapy is an independent predictive factor irrespective of simplified breast cancer intrinsic subtypes: a landmark and two-step approach analyses from the EORTC 10994/BIG 1-00 phase III trial. Ann Oncol. 2014;25:1128–36.
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804.
Bonnefoi H, MacGrogan G, Poncet C, Iggo R, Bergh J, Cameron D. Molecular apocrine tumours in EORTC 10994/BIG 1-00 phase III study: pathological response after neoadjuvant chemotherapy and clinical outcomes. Br J Cancer. 2019;120:913–21.
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N. Engl J Med. 2017;376:2147–59.
von Minckwitz G, Huang CS, Mano MS, Loibl S, Mamounas EP, Untch M, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N. Engl J Med. 2019;380:617–28.
Balko JM, Giltnane JM, Wang K, Schwarz LJ, Young CD, Cook RS, et al. Molecular profiling of the residual disease of triple-negative breast cancers after neoadjuvant chemotherapy identifies actionable therapeutic targets. Cancer Discov. 2014;4:232–45.
Kim C, Gao R, Sei E, Brandt R, Hartman J, Hatschek T, et al. Chemoresistance evolution in triple-negative breast cancer delineated by single-cell sequencing. Cell. 2018;173:879–893 e813.
Yates LR, Gerstung M, Knappskog S, Desmedt C, Gundem G, Van Loo P, et al. Subclonal diversification of primary breast cancer revealed by multiregion sequencing. Nat Med. 2015;21:751–59.
The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70.
Bertucci F, Ng CKY, Patsouris A, Droin N, Piscuoglio S, Carbuccia N, et al. Genomic characterization of metastatic breast cancers. Nature. 2019;569:560–64.
Andre F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N. Engl J Med. 2019;380:1929–40.
Tung NM, Robson ME, Ventz S, Santa-Maria CA, Nanda R, Marcom PK, et al. TBCRC 048: phase II study of olaparib for metastatic breast cancer and mutations in homologous recombination-related genes. J Clin Oncol. 2020. https://doi.org/10.1200/JCO.20.02151.
Hyman DM, Smyth LM, Donoghue MTA, Westin SN, Bedard PL, Dean EJ, et al. AKT Inhibition in Solid Tumors With AKT1 Mutations. J Clin Oncol. 2017;35:2251–2259.
Bonnefoi H, Piccart M, Bogaerts J, Mauriac L, Fumoleau P, Brain E, et al. TP53 status for prediction of sensitivity to taxane versus non-taxane neoadjuvant chemotherapy in breast cancer (EORTC 10994/BIG 1-00): a randomised phase 3 trial. Lancet Oncol. 2011;12:527–39.
Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–60.
Tischler G, Leonard S. biobambam: tools for read pair collation based algorithms on BAM files. Source Code Biol Med. 2014;9:13.
Raine KM, Hinton J, Butler AP, Teague JW, Davies H, Tarpey P, et al. cgpPindel: identifying somatically acquired insertion and deletion events from paired end sequencing. Curr Protoc Bioinforma. 2015;52:15 17 11-12.
Chang MT, Asthana S, Gao SP, Lee BH, Chapman JS, Kandoth C, et al. Identifying recurrent mutations in cancer reveals widespread lineage diversity and mutational specificity. Nat Biotechnol. 2016;34:155–63.
Zehir A, Benayed R, Shah RH, Syed A, Middha S, Kim HR, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23:703–13.
Condorelli R, Mosele F, Verret B, Bachelot T, Bedard PL, Cortes J, et al. Genomic alterations in breast cancer: level of evidence for actionability according to ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann Oncol. 2019;30:365–73.
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature. 2012;486:346–52.
Nik-Zainal S, Davies H, Staaf J, Ramakrishna M, Glodzik D, Zou X, et al. Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature. 2016;534:47–54.
Farmer P, Bonnefoi H, Anderle P, Cameron D, Wirapati P, Becette V, et al. A stroma-related gene signature predicts resistance to neoadjuvant chemotherapy in breast cancer. Nat Med. 2009;15:68–74.
Quenel-Tueux N, Debled M, Rudewicz J, MacGrogan G, Pulido M, Mauriac L, et al. Clinical and genomic analysis of a randomised phase II study evaluating anastrozole and fulvestrant in postmenopausal patients treated for large operable or locally advanced hormone-receptor-positive breast cancer. Br J Cancer. 2015;113:585–94.
Weigelt B, Pusztai L, Ashworth A, Reis-Filho JS. Challenges translating breast cancer gene signatures into the clinic. Nat Rev Clin Oncol. 2011;9:58–64.
Sachs N, de Ligt J, Kopper O, Gogola E, Bounova G, Weeber F, et al. A living biobank of breast cancer organoids captures disease heterogeneity. Cell. 2018;172:373–86.
Sflomos G, Dormoy V, Metsalu T, Jeitziner R, Battista L, Scabia V, et al. A preclinical model for ERalpha-positive breast cancer points to the epithelial microenvironment as determinant of luminal phenotype and hormone response. Cancer Cell. 2016;29:407–22.
Richard E, Grellety T, Velasco V, MacGrogan G, Bonnefoi H, Iggo R. The mammary ducts create a favourable microenvironment for xenografting of luminal and molecular apocrine breast tumours. J Pathol. 2016;240:256–61.
Acknowledgements
We thank the patients, doctors and nurses involved in the EORTC 10994/BIG 1-00 study for their generous participation. We thank Ultan MacDermott and the Sanger Sample Management and Sequencing team for processing the specimens for NGS.
Funding
We thank the Fondation pour la lutte contre le cancer et pour des recherches medico-biologiques, the Site de Recherche Intégrée sur le Cancer—Bordeaux Recherche Intégrée Oncologie Grant INCa-DGOS-Inserm 6046, and the Breast Cancer Working Group EBCC12 grant for financial support. The funding sources had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the study data and the final responsibility for the decision to submit for publication. Trial design, conduct, and analysis were done at the EORTC headquarters, the Institut Bergonié and Wellcome Sanger Institute independently from all funding bodies.
Author information
Authors and Affiliations
Consortia
Contributions
HB, RI and DC conceived the study. DC, HB and EORTC clinical investigators provided clinical samples. CP analysed the clinical data. GMG analysed the histology. JS extracted the DNA. AC and RI analysed the NGS data and made the figures. RI, HB and AC wrote the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The EORTC 10994 clinical trial was registered with ClinicalTrials.gov number NCT00017095 and approved by National and/or Local Ethics Committees in all participating centres. Before registration, all patients signed an informed consent for the trial and for mandatory p53 gene assessment on tumour samples. Patients involved in this substudy gave consent for additional biological research on their tumour samples. The study was performed in accordance with the Declaration of Helsinki.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chatzipli, A., Bonnefoi, H., MacGrogan, G. et al. Patterns of genomic change in residual disease after neoadjuvant chemotherapy for estrogen receptor-positive and HER2-negative breast cancer. Br J Cancer 125, 1356–1364 (2021). https://doi.org/10.1038/s41416-021-01526-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01526-3