Abstract
Background
Five-year ovarian cancer survival rates are below 50%; there is considerable interest in whether common medications like statins may improve survival.
Methods
We identified women diagnosed with ovarian cancer in Australia from 2003 to 2013 through the Australian Cancer Database and linked these records to national medication and death databases. We used Cox proportional hazards regression to estimate hazard ratios (HR) and confidence intervals (CI) for associations between statins and survival.
Results
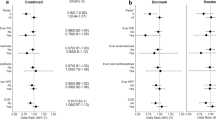
Pre-diagnosis statin use was not associated with survival overall but was associated with better survival among women with endometrioid cancers. Statin use after diagnosis was associated with better ovarian cancer-specific survival (OVS, HR = 0.87, 95%CI 0.81–0.94), but this association was largely restricted to women who started using statins after their cancer diagnosis (OVS HR = 0.68, 0.57–0.81 vs. HR = 0.94, 0.87–1.01 for continuing users). The association was strongest for endometrioid cancers (OVS HR = 0.48, 0.29–0.77).
Conclusions
Use of statins may confer a survival benefit for women with ovarian cancer but it is impossible to rule out bias in observational studies. Particularly problematic are reverse causation where disease status affects statin use, confounding by indication and the absence of data for women with normal cholesterol levels. A randomised trial is required to provide definitive evidence.
Similar content being viewed by others
Background
Statins inhibit 3-hydroxy-3-methylglutaryl-coenzyme A (HMGCoA) reductase, a key enzyme in the mevalonate pathway. This inhibition lowers levels of cholesterol and may also affect other non-sterol side-products involved in cell growth, repair and survival [1]. In vitro studies suggest elevated HMG-CoA reductase gene expression allows more rapid growth of tumour cells and prolongs their survival compared to normal cells [2], and that statin-induced reduction in mevalonate side-products could induce apoptosis thereby restricting tumour growth [3], with greater effects seen for lipophilic statins, which may penetrate solid tumours more easily, than for hydrophilic statins [4]. In vitro and animal studies also suggest that concurrent use of statins may improve the effectiveness of chemotherapy [5].
In a meta-analysis of 95 studies and more than one million cancer patients with a variety of cancers, statin use was associated with a 30% reduction in all-cause mortality and a 40% reduction in cancer-specific mortality [6]. There is also evidence that the use of statins (3-hydroxy-3-methylglutaryl coenzyme A [HMG-CoA] reductase inhibitors) might improve ovarian cancer survival. In a recent meta-analysis, we observed a consistent reduction in ovarian cancer mortality associated with the use of statins with similar associations seen for use of statins before, around the time of, or after diagnosis [7]. One small study has also reported an association between higher pre-diagnosis low-density lipoprotein (LDL) levels and shorter survival after a diagnosis of advanced ovarian cancer [8]. Previous studies have, however, had limited power to compare lipophilic and hydrophilic statins and to assess whether the association differs for the different histotypes of ovarian cancer although these differ in both aetiology [9] and prognosis [10].
We have used a national linked dataset to further evaluate the potential effects of statin use after a diagnosis of ovarian cancer.
Methods
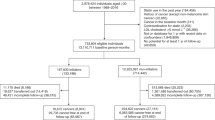
Data from the Australian Medicare Enrolments database, which includes all women eligible to receive reimbursement for health care in Australia (citizens and permanent residents), were linked to the Australian Cancer Database (ACD), the Pharmaceutical Benefits Scheme database (PBS) and the Australian National Death Index (NDI). The ACD provided information on all cancers diagnosed in Australia from 1982 to 2013 (2012 in New South Wales, NSW), including the date and site of primary cancer diagnosis and date and cause of death (to 2013); information about the stage and grade of cancer at diagnosis and debulking status was not available. The NDI provided date of death, age at death, and cause(s) of death with complete information from 1996 to 2015. The PBS provided information about prescriptions for cholesterol-lowering and diabetes medications and chemotherapy, filled between 2002 and 2017. Linkage was performed by the Data Linkage Unit at the Australian Institute of Health and Welfare (AIHW) and the resulting de-identified dataset was made available to the authors for analysis via the Secure Unified Research Environment (SURE) at the Sax Institute, Sydney, Australia. The study was approved by the Human Research Ethics Committees at QIMR Berghofer Medical Research Institute, the AIHW and all relevant data custodians.
Before mid-2002, prescriptions could not reliably be linked to individual family members so for this analysis we included women newly diagnosed with ovarian, fallopian tube or primary peritoneal cancer (ICD-10 codes C56, C57.0 or C48.2), henceforth referred to as ovarian cancer, between 1/7/2003 and 31/12/2013 (31/12/2012 in NSW) (Fig. 1, N = 14,545). This date range ensured we had prescription data for at least one year prior to cancer diagnosis. Women with a previous or concurrent invasive cancer (N = 2062, 14%) or aged less than 18 or more than 89 years at diagnosis (N = 453, 3%) were excluded. We also excluded women diagnosed less than one year after they enrolled for Medicare (N = 92, 0.6%) as they did not have a full year of prescription information prior to their diagnosis. Consistent with previous reports [11], we excluded women who died in the first year after diagnosis (N = 2796, 19%) as we considered it unlikely that statin use would have affected their outcome. We excluded a further 7 women missing the information needed to derive an area-level measure of socioeconomic status. We further excluded 506 women with non-epithelial or borderline cancers, leaving a final cohort of 8629 women including 5136 with serous cancer, 602 mucinous, 777 endometrioid, 514 clear cell, 244 carcinosarcomas, 1047 with ‘carcinoma not-otherwise specified’ (likely to be serous cancer) and 309 with other epithelial or unknown cancer types (see Supplementary Table S1 for histotype classification). Survival was measured from one year after diagnosis to the earliest of death, or the end of follow-up at 31/12/2015. The outcomes of interest were ovarian cancer-specific and all-cause mortality.
Prior to mid-2012, the PBS database only recorded prescriptions for medications that attracted a government rebate because they cost more than the ‘co-payment threshold’. This threshold is the maximum amount an individual has to pay for a medication with a much lower level set for those who qualify for a Medicare concession card (primarily those over the age of 65 or with a government allowance or pension). Most statins were above the general co-payment threshold throughout the study period so prescription data for statins are close to complete. However, other medications (e.g. for diabetes) fall below this threshold and thus, prior to mid-2012, complete data are only available for concession card holders. Women were classified as a concession card holder if they were recorded as filling at least one prescription (for any medication) with a concession card in the calendar year prior to their cancer diagnosis.
We defined pre-diagnosis statin use as two or more prescriptions for statins filled on separate dates within one year prior to the ovarian cancer diagnosis. Post-diagnosis use was defined as two or more statin prescriptions filled on separate dates after diagnosis. Women were classified as users of lipophilic (simvastatin, fluvastatin, and atorvastatin) or hydrophilic (pravastatin and rosuvastatin) statins if at least 80% of prescriptions they filled were for that class of statin; women who filled prescriptions for a mix of types were excluded from analyses of statin type. Lovastatin is not available in Australia.
We used Cox proportional hazards regression to derive hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between statin use and survival. All analyses were adjusted for age and year at diagnosis, and the area-level Index of Relative Socio-economic Disadvantage (IRSD, categorised into quintiles) [12]. Analyses of post-diagnosis use were further adjusted for histotype and treatment with chemotherapy in the first 90 days as a proxy for cancer severity. We did not adjust for country of birth, state/territory of residence at diagnosis, or an area-level measure of remoteness (Accessibility and Remoteness Index, ARIA [13]) as these variables were not strongly associated with statin use or survival and including them made little difference to the estimates of interest.
In primary analyses of post-diagnosis statin use, we examined ever/never use as a time-varying covariate with a 12-month lag period. Women were initially considered non-users post-diagnosis and then reclassified as users 12 months after their second post-diagnosis statin prescription. Similarly, we also assessed short (2-12 30-day prescriptions after diagnosis) and long-term (>12 prescriptions) statin use, again with a 12-month lag. Women were initially classified as short-term users and then reclassified as long-term users when they met this definition. The use of a lag minimised the potential that events towards the end of life might influence statin use. We then assessed the effect of timing of statin use by categorising women as never users (no pre- or post-diagnosis use, reference group), new users (post-diagnosis use only), continuous users (both pre- and post-diagnosis use), and prior users (pre-diagnosis use only). Women thus started follow-up as never or prior users based on their pre-diagnosis use and were reclassified as new or continuous users 12 months after their second post-diagnosis script. Further analyses were conducted by lipid affinity (lipophilic vs. hydrophilic statins), stratified by histotype, and in the subset of concession card holders where we could use prescription of anti-diabetic medications to classify women as having mild (prescriptions for either metformin or a sulphonylurea), severe (any prescription for insulin) or moderate (all other diabetes medications) diabetes.
To test the robustness of our primary results, we conducted a series of sensitivity analyses. First, we reduced the lag period for post-diagnosis use from 12 to six and zero months. Second, we assessed post-diagnosis statin use during fixed exposure periods of 1 and 3 years after the initial cancer diagnosis and followed women from the end of the relevant exposure period. In the 1-year fixed post-diagnosis statin use analysis, we also examined both short-term (1–3 years) and long-term (>3 years) survival and ran models restricted to women treated with chemotherapy to assess the concurrent use of statins during chemotherapy treatment. Analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC).
Results
Table 1 shows the characteristics of the women by statin use in the first year after their diagnosis of ovarian cancer. As expected, statin users were older than non-users and so were slightly more likely to have serous cancers and have been treated with chemotherapy. They were also more likely to be in the lowest quintile of socioeconomic status and to use medications for diabetes. As use of statins has increased over time, users were diagnosed more recently. The groups did not differ markedly with respect to their country of birth or place of residence.
In total, 4652 women (54%) died during the follow-up period; 4263 deaths (92%) were from ovarian cancer, 121 (3%) from another form of cancer, 266 (6%) from other causes and two of unknown cause. As expected, ovarian cancer-specific mortality was lower among women with mucinous, endometrioid and clear cell cancers compared to those with serous cancers and carcinosarcomas (Supplementary Table 2). It was also lower among women who were not treated with chemotherapy (likely early stage disease), women born in Asia or of unknown country of birth, women with no or only mild diabetes and those diagnosed more recently. Non-cancer mortality was higher among those of lowest socioeconomic status and those with more severe diabetes.
Overall, 2119 women (25%) used statins in the year prior to their diagnosis, filling a median of 11 prescriptions each during the year (interquartile range 8–12). Pre-diagnosis statin use was not associated with overall survival (HR = 1.02, 95% CI 0.96–1.09) or with ovarian cancer-specific (1.04, 0.97–1.12) mortality and there was little difference between hydrophilic and lipophilic statins (Table 2). The results were essentially unchanged when we considered statin use in the two years prior to diagnosis, included histotype and/or treatment with chemotherapy in the models, or when we additionally adjusted for use of diabetes medications, as a marker of diabetes severity, among concession card holders (results not shown). When we stratified by histotype, statin use pre-diagnosis was associated with higher ovarian cancer-specific mortality among women with carcinosarcomas and mucinous cancers, but with lower mortality among those with endometrioid cancers (Table 2).
In total, 2564 women (30%) used statins at some point after their cancer diagnosis including 1835 who had also used statins before diagnosis (continuing users) and 729 new users; 2354 women met the definition of a user for time-varying analyses (>12 months follow-up after their second prescription). In our primary time-varying models, post-diagnosis statin users had 13% lower ovarian cancer-specific mortality overall (HR = 0.87, 95% CI 0.81–0.94), with a 19% reduction for those who had filled at least 12 prescriptions after their cancer diagnosis (0.81, 0.73–0.89) (Table 3). The reduction in ovarian cancer-specific mortality was seen for both types of statins but was largely restricted to women who only started using statins after their cancer diagnosis (HR = 0.68, 95% CI 0.57–0.81) with little apparent benefit seen for women who had also used statins prior to their diagnosis (0.94, 0.87–1.01). Women who stopped taking statins after their cancer diagnosis had the highest mortality (1.36, 1.20–1.54). Results from models with a 6-month lag were similar; however, the associations were slightly stronger when we reduced the lag to zero (Table 4; HR for any statin use and ovarian cancer-specific mortality = 0.83; 95% CI 0.77–0.89).
As for analyses of pre-diagnosis use, the inverse association with post-diagnosis statin use was strongest among women with endometrioid cancers (Table 3), where it was seen among both continuing (HR = 0.51, 95% CI 0.30–0.86) and new users (0.34, 0.12–0.94). A significant inverse association was also seen for serous cancers overall, but this was restricted to women who started using statins after their cancer diagnosis (HR = 0.63, 95% CI 0.52–0.77) and was not seen among continuing users (0.94, 0.86–1.03). Statin use was associated with slightly higher ovarian cancer-specific mortality among women with mucinous cancers.
We also conducted sensitivity analyses similar to Verdoodt et al. [11] looking at fixed exposure periods after diagnosis and short- and long-term follow-up (Table 4). Compared to the time-varying models, the overall association between use of statins in the first year after diagnosis and ovarian cancer-specific mortality was weaker (HR = 0.93, 95% CI 0.86–1.00) and it did not vary appreciably with the length of follow-up. When we stratified by chemotherapy treatment, there was no suggestion of a survival benefit for statin use among women treated with chemotherapy (HR = 0.97, 95% CI 0.90–1.05), although a benefit was seen among women not treated with chemotherapy (HR = 0.84, 95% CI 0.72–0.98). Any use of statins in the first three years after diagnosis was associated with significantly lower mortality (HR = 0.80, 95% CI 0.71–0.89).
Discussion
Our results suggest that mortality is ~13% lower among women with ovarian cancer who use statins after their diagnosis, with greater reductions for women with endometrioid cancers and those who use them for longer. However, the overall reduction in risk was only seen for women who initiated statin use after their cancer diagnosis and not for women who used them before diagnosis as well. The only exception to this pattern was among women with endometrioid cancers where we saw a survival benefit among both new and continuing users of statins. There was no suggestion that taking statins with chemotherapy was associated with improved survival, but the stronger association among women who were not treated with chemotherapy suggests any potential benefit of statins might be greater for women with earlier stage disease, although we were not able to assess this directly.
Overall, our results are broadly consistent with previous reports, although the inverse association we observed is more modest than that from a recent meta-analysis [7] (HR = 0.87 vs. 0.76 in the meta-analysis). Of note, both the size and pattern of our results are very consistent with those from a previous record-linkage study from Denmark [11] although that was limited by a smaller sample size and so their effect estimates were not statistically significant. Despite pre-clinical data suggesting that lipophilic statins might be expected to have a greater effect than hydrophilic statins, we saw no difference between the two and this is consistent with previous reports [14,15,16].
Like us, the Danish linkage study reported an inverse association among women with endometrioid cancers although in their analysis a similar association was seen for clear cell cancers [11]; in contrast, others have reported similar associations for all histotypes but sample sizes have been limited [16]. A beneficial effect for women with endometrioid cancers is not implausible. Observational studies have reported stronger associations between overweight and obesity (measured as body mass index) and risk of the endometrioid and mucinous histotypes [17, 18] and, in a Mendelian randomisation study using a genetic variant that inhibits HMGCoA reductase, the target of statins, the observed inverse association with ovarian cancer risk was strongest for the endometrioid histotype [19].
Unlike others [20,21,22], we saw no evidence of an overall survival benefit for women who used statins before their diagnosis of ovarian cancer, although we did see a benefit in terms of ovarian cancer-specific mortality among women with endometrioid cancers. Women who are prescribed a statin will have some indication for this, usually high cholesterol levels, and they may, therefore, differ from non-users in ways that would affect their cancer prognosis. In practice, it is likely that women with comorbidity would have worse survival than those without [23], so it is possible that confounding by indication has biased our effect estimates upwards, thereby masking a true inverse association with statins.
Our observation that the reduction in mortality associated with the use of statins after diagnosis is largely restricted to new users, is also consistent with the Danish study [11]. It is possible that cancers that have developed in the presence of a statin are then ‘resistant’ to statin use after diagnosis, thereby explaining the lack of benefit for continuing users; however, it is notable that we also saw significantly higher mortality among women who used statins before their cancer diagnosis but then stopped. This raises concerns about whether statins are influencing survival or whether a woman’s general health status is influencing her statin use; a form of reverse causation whereby a woman’s prognosis affects her statin use rather than the other way around such that women only initiate statin use after diagnosis if their cancer is under control, while the continuation of statins is a low priority for those struggling with their cancer.
Strengths of our analysis include the large sample size (this is the biggest sample to date), the use of time-varying models to prevent immortal-time bias and the high levels of adherence in our population. The main limitation is the limited amount of information available regarding potential confounders including stage and grade of disease, and the absence of information about cancer recurrence. In particular, we were unable to separate high- and low-grade serous cancers so, as the vast majority of serous cancers are high-grade, our results will pertain primarily to this group. In a previous study, we reported that women who used statins were slightly more likely to have high-grade serous cancers, to be overweight or obese and to have other comorbidities [22]. These factors would all tend to increase mortality among statin users, suggesting they cannot explain the inverse associations we have seen. However, statin users were also more likely to use other medications including metformin and aspirin [22] which might also reduce mortality. Another limitation of any observational study is that women who do not have elevated high cholesterol levels rarely use statins so it is not possible to draw any conclusions about the potential effects of statin use in this group.
Conclusion
Our results confirm previous observations that women with ovarian cancer who take statins after their diagnosis may have better survival than women who do not use statins. However, it is impossible to rule out all potential sources of bias in observational studies. Particularly important in a population like this, where a high proportion of women are likely to be experiencing side-effects of both treatment and the disease, is the possibility of reverse causation. There are also no data about the potential effects of statins among women who do not have high cholesterol levels. On this basis, we believe it is too early to recommend that all women with ovarian cancer take statins to improve their survival and that definitive evidence about the potential benefits of statins for women with ovarian cancer will require a randomised trial.
Data availability
The datasets used for the current study are not publicly available due to privacy issues. Strict access restrictions apply to linked data such that they can only be accessed by approved study investigators.
References
Wang CY, Liu PY, Liao JK. Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol Med. 2008;14:37–44.
Thurnher M, Gruenbacher G, Nussbaumer O. Regulation of mevalonate metabolism in cancer and immune cells. Biochim Biophys Acta. 2013;1831:1009–15.
Wong WW, Dimitroulakos J, Minden MD, Penn LZ. HMG-CoA reductase inhibitors and the malignant cell: the statin family of drugs as triggers of tumor-specific apoptosis. Leukemia. 2002;16:508–19.
Kato S, Smalley S, Sadarangani A, Chen-Lin K, Oliva B, Branes J, et al. Lipophilic but not hydrophilic statins selectively induce cell death in gynaecological cancers expressing high levels of HMGCoA reductase. J Cell Mol Med. 2010;14:1180–93.
Gazzerro P, Proto MC, Gangemi G, Malfitano AM, Ciaglia E, Pisanti S, et al. Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharm Rev. 2012;64:102–46.
Mei Z, Liang M, Li L, Zhang Y, Wang Q, Yang W. Effects of statins on cancer mortality and progression: a systematic review and meta-analysis of 95 cohorts including 1,111,407 individuals. Int J Cancer. 2017;140:1068–81.
Majidi A, Na R, Dixon-Suen S, Jordan SJ, Webb PM. Common medications and survival in women with ovarian cancer: a systematic review and meta-analysis. Gynecol Oncol. 2020;157:678–85.
Li AJ, Elmore RG, Chen IY, Karlan BY. Serum low-density lipoprotein levels correlate with survival in advanced stage epithelial ovarian cancers. Gynecol Oncol. 2010;116:78–81.
Wentzensen N, Poole EM, Trabert B, White E, Arslan AA, Patel AV, et al. Ovarian cancer risk factors by histologic subtype: an analysis from the Ovarian Cancer Cohort Consortium. J Clin Oncol. 2016;34:2888–98.
Anuradha S, Webb PM, Blomfield P, Brand AH, Friedlander M, Leung Y, et al. Survival of Australian women with invasive epithelial ovarian cancer: a population-based study. Med J Aust. 2014;201:283–8.
Verdoodt F, Kjaer HM, Kjaer SK, Pottegard A, Friis S, Dehlendorff C. Statin use and mortality among ovarian cancer patients: a population-based cohort study. Int J Cancer. 2017;141:279–86.
Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia. Canberra: Australian Bureau of Statistics. Contract No.: Cat no. 5.001 (2013).
Australian Government Department of Health. Accessibility Remoteness Index of Australia (ARIA) Remoteness Area (RA). Canberra (2011).
Couttenier A, Lacroix O, Vaes E, Cardwell CR, De Schutter H, Robert A. Statin use is associated with improved survival in ovarian cancer: a retrospective population-based study. PLoS ONE. 2017;12:e0189233.
Harding BN, Delaney JA, Urban RR, Weiss NS. Use of statin medications following diagnosis in relation to survival among women with ovarian cancer. Cancer Epidemiol Biomark. Prev. 2019;28:1127–33.
Vogel TJ, Goodman MT, Li AJ, Jeon CY. Statin treatment is associated with survival in a nationally representative population of elderly women with epithelial ovarian cancer. Gynecol Oncol. 2017;146:340–5.
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 2012;9:e1001200.
Olsen CM, Nagle C, Whiteman DC, Ness R, Pearce CL, Pike MC, et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr Relat Cancer. 2013;20:251–62.
Yarmolinsky J, Bull C, Vincent E, Robinson J, Walther A, Davey Smith G, et al. Association between genetically proxied inhibition of HMG-CoA reductase and epithelial ovarian cancer. J Am Med Assoc. 2020;323:646–55.
Wang A, Aragaki AK, Tang JY, Kurian AW, Manson JE, Chlebowski RT, et al. Statin use and all-cancer survival: prospective results from the Women’s Health Initiative. Br. J. Cancer. 2016;115:129–35.
Urpilainen E, Marttila M, Hautakoski A, Arffman M, Sund R, Ilanne-Parikka P, et al. Prognosis of ovarian cancer in women with type 2 diabetes using metformin and other forms of antidiabetic medication or statins: a retrospective cohort study. BMC Cancer. 2018;18:767.
Majidi, A, Na, R, Jordan, SJ, De Fazio, A, Webb, PM, OPAL Study Group. Statin use and survival following a diagnosis of ovarian cancer: a prospective observational study. Int J Cancer. 2020. https://doi.org/10.1002/ijc.33333.
Tetsche MS, Dethlefsen C, Pedersen L, Sorensen HT, Norgaard M. The impact of comorbidity and stage on ovarian cancer mortality: a nationwide Danish cohort study. BMC Cancer. 2008;8:31.
Acknowledgements
We acknowledge the Australian Capital Territory Cancer Registry; New South Wales Central Cancer Registry and Ministry of Health; Chief Health Officer of the Northern Territory; Queensland Department of Health; South Australia Health, Government of South Australia; Director of Public Health Tasmania; Victorian Cancer Registry; Western Australia Cancer Registry and Commonwealth Department of Health for allowing access to their data. We also thank the Data Linkage Group at the Australian Institute of Health and Welfare (AIHW) for their help with facilitating and performing the data linkage. This project was approved by all relevant human research ethics committees (QIMR Berghofer Medical Research Institute HREC; AIHW HREC; ACT Health HREC, 3 August 2015; NSW Population and Health Services Research Ethics Committee; SA Health Human Research Ethics Committee; Human Research Ethics Committee (Tasmania) Network; Cancer Council Victoria Human Research Ethics Committee).
Funding
This work was supported by the National Health and Medical Research Council (NHMRC) of Australia (GNT1073898). P.M.W. was supported by a fellowship from the NHMRC (GNT1173346).
Author information
Authors and Affiliations
Contributions
Jia-Li Feng: Data analysis, interpretation of results, editing and review of the final manuscript; Suzanne Dixon-Suen: Project design, interpretation of results, editing and review of the final manuscript; Susan Jordan: Project design, interpretation of results, editing and review of the final manuscript; Penelope Webb: Funding acquisition, project design, supervision, interpretation of results, drafting and revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Research Ethics Committees at QIMR Berghofer Medical Research Institute (P2061), the Australian Institute of Health and Welfare (EO2014-3-116) and all relevant data custodians. The study was performed in accordance with the Declaration of Helsinki and the authors did not have any access to identifying information for individuals. Individual consent was not obtained.
Consent to publish
Not applicable.
Competing interests
P.M.W. has received grant funding from Astra Zeneca for an unrelated ovarian cancer study. The remaining authors have declared no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Feng, JL., Dixon-Suen, S.C., Jordan, S.J. et al. Statin use and survival among women with ovarian cancer: an Australian national data-linkage study. Br J Cancer 125, 766–771 (2021). https://doi.org/10.1038/s41416-021-01460-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01460-4
This article is cited by
-
Pre-operative levels of angiopoietin protein-like 3 (ANGPTL3) in women diagnosed with high-grade serous carcinoma of the ovary
Lipids in Health and Disease (2024)