Abstract
In children with desmoid-type fibromatosis (DTF) in whom disease progression occurs after an initial watch-and-wait strategy, prolonged low-dose chemotherapy using vinblastine and methotrexate (VBL-MTX) is currently the standard of care. These conventional drugs have been prospectively evaluated but their efficacy and safety profiles are limited, and alternative therapeutic options are therefore essential. Based on the results of clinical trials, the use of tyrosine kinase inhibitors (TKIs) in the treatment of DTF is currently considered only in adult patients. TKIs such as imatinib show superior therapeutic efficacy to VBL-MTX and tolerable short-term side effects for the treatment of adult DFT, supporting the concept of the use of TKIs for the treatment of paediatric DFT. Moreover, new-generation TKIs, such as pazopanib and sorafenib, have shown improved therapeutic efficacy compared to imatinib in adult non-comparative studies. A tolerable safety profile of TKI therapy in children with disease entities other than DTF, such as leukaemia, has been reported. However, the efficacy and, in particular, the long-term safety of TKIs, including childhood-specific aspects such as growth and fertility, for the treatment of children with DTF should be investigated prospectively, as DFT therapy requires long-term drug exposure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Schmidt, B. F., Koscielniak, E., Pilz, T. & Treuner, J. Radiation therapy in juvenile aggressive fibromatosis. Klin. Padiatr. 211, 296–299 (1999).
Reitamo, J. J., Scheinin, T. M. & Hayry, P. The desmoid syndrome. New aspects in the cause, pathogenesis and treatment of the desmoid tumor. Am. J. Surg. Feb. 151, 230–237 (1986).
Anthony, T., Rodriguez-Bigas, M. A., Weber, T. K. & Petrelli, N. J. Desmoid tumors. J. Am. Coll. Surg. 182, 369–377 (1996).
Orbach, D., Brennan, B., Bisogno, G., Van Noesel, M., Minard-Colin, V., Daragjati, J. et al. The EpSSG NRSTS 2005 treatment protocol for desmoid-type fibromatosis in children: an international prospective case series. Lancet Child Adolesc. Health 1, 284–292 (2017).
Fiore, M., Rimareix, F., Mariani, L., Domont, J., Collini, P., Le Pechoux, C. et al. Desmoid-type fibromatosis: a front-line conservative approach to select patients for surgical treatment. Ann. Surg. Oncol. 16, 2587–2593 (2009).
Fletcher, C. D. The evolving classification of soft tissue tumours—an update based on the new 2013 WHO classification. Histopathology. 64, 2–11 (2014).
Penel, N., Coindre, J. M., Bonvalot, S., Italiano, A., Neuville, A., Le Cesne, A. et al. Management of desmoid tumours: a nationwide survey of labelled reference centre networks in France. Eur. J. Cancer 58, 90–96 (2016).
Agresta, L., Kim, H., Turpin, B. K., Nagarajan, R., Plemmons, A., Szabo, S. et al. Pazopanib therapy for desmoid tumors in adolescent and young adult patients. Pediatr. Blood Cancer 65, e26968 (2018).
Trautmann, M., Rehkamper, J., Gevensleben, H., Becker, J., Wardelmann, E., Hartmann, W. et al. Novel pathogenic alterations in pediatric and adult desmoid-type fibromatosis—a systematic analysis of 204 cases. Sci. Rep. 25, 10:3368 (2020).
Meazza, C., Belfiore, A., Busico, A., Settanni, G., Paielli, N., Cesana, L. et al. AKT1 and BRAF mutations in pediatric aggressive fibromatosis. Cancer Med. 5, 1204–1213 (2016).
Meazza, C., Bisogno, G., Gronchi, A., Fiore, M., Cecchetto, G., Alaggio, R. et al. Aggressive fibromatosis in children and adolescents: the Italian experience. Cancer 116, 233–240 (2010).
Oudot, C., Orbach, D., Minard-Colin, V., Michon, J., Mary, P., Glorion, C. et al. Desmoid fibromatosis in pediatric patients: management based on a retrospective analysis of 59 patients and a review of the literature. Sarcoma 2012, 475202 (2012).
Woltsche, N., Gilg, M. M., Fraissler, L., Liegl-Atzwanger, B., Beham, A., Lackner, H. et al. Is wide resection obsolete for desmoid tumors in children and adolescents? Evaluation of histological margins, immunohistochemical markers, and review of literature. Pediatr. Hematol. Oncol. 32, 60–69 (2015).
Rutenberg, M. S., Indelicato, D. J., Knapik, J. A., Lagmay, J. P., Morris, C., Zlotecki, R. A. et al. External-beam radiotherapy for pediatric and young adult desmoid tumors. Pediatr. Blood Cancer 57, 435–442 (2011).
Buitendijk, S., van de Ven, C. P., Dumans, T. G., den Hollander, J. C., Nowak, P. J., Tissing, W. J. et al. Pediatric aggressive fibromatosis: a retrospective analysis of 13 patients and review of literature. Cancer 104, 1090–1099 (2005).
Kasper, B., Baumgarten, C., Garcia, J., Bonvalot, S., Haas, R., Haller, F. et al. An update on the management of sporadic desmoid-type fibromatosis: a European Consensus Initiative between Sarcoma PAtients EuroNet (SPAEN) and European Organization for Research and Treatment of Cancer (EORTC)/Soft Tissue and Bone Sarcoma Group (STBSG). Ann. Oncol. 28, 2399–2408 (2017).
Penel, N., Le Cesne, A., Bonvalot, S., Giraud, A., Bompas, E., Rios, M. et al. Surgical versus non-surgical approach in primary desmoid-type fibromatosis patients: a nationwide prospective cohort from the French Sarcoma Group. Eur. J. Cancer 83, 125–131 (2017).
Gounder, M. M., Mahoney, M. R., Van Tine, B. A., Ravi, V., Attia, S., Deshpande, H. A. et al. Sorafenib for advanced and refractory desmoid tumors. N. Engl. J. Med. 379, 2417–2428 (2018). 20.
Salas, S., Brulard, C., Terrier, P., Ranchere-Vince, D., Neuville, A., Guillou, L. et al. Gene expression profiling of desmoid tumors by cDNA microarrays and correlation with progression-free survival. Clin. Cancer Res. 21, 4194–4200 (2015).
Colombo, C., Miceli, R., Lazar, A. J., Perrone, F., Pollock, R. E., Le Cesne, A. et al. CTNNB1 45F mutation is a molecular prognosticator of increased postoperative primary desmoid tumor recurrence: an independent, multicenter validation study. Cancer 119, 3696–3702 (2013).
Meazza, C., Alaggio, R. & Ferrari, A. Aggressive fibromatosis in children: a changing approach. Minerva Pediatr. 63, 305–318 (2011).
Skapek, S. X., Ferguson, W. S., Granowetter, L., Devidas, M., Perez-Atayde, A. R., Dehner, L. P. et al. Vinblastine and methotrexate for desmoid fibromatosis in children: results of a Pediatric Oncology Group Phase II Trial. J. Clin. Oncol. 25, 501–506 (2007).
Azzarelli, A., Gronchi, A., Bertulli, R., Tesoro, J. D., Baratti, D., Pennacchioli, E. et al. Low-dose chemotherapy with methotrexate and vinblastine for patients with advanced aggressive fibromatosis. Cancer 92, 1259–1264 (2001).
Toulmonde, M., Pulido, M., Ray-Coquard, I., Andre, T., Isambert, N., Chevreau, C. et al. Pazopanib or methotrexate-vinblastine combination chemotherapy in adult patients with progressive desmoid tumours (DESMOPAZ): a non-comparative, randomised, open-label, multicentre, phase 2 study. Lancet Oncol. 20, 1263–1272 (2019).
Duhil de Benaze, G., Vigan, M., Corradini, N., Minard-Colin, V., Marie-Cardine, A., Verite, C. et al. Functional analysis of young patients with desmoid-type fibromatosis: initial surveillance does not jeopardize long term quality of life. Eur. J. Surg. Oncol. 46, 1294–1300 (2020).
Skapek, S. X., Ferguson, W. S., Granowetter, L., Devidas, M., Perez-Atayde, A. R., Dehner, L. P. et al. Vinblastine and methotrexate for desmoid fibromatosis in children: results of a Pediatric Oncology Group Phase II Trial. J. Clin. Oncol. 25, 501–506 (2007).
Group, D. T. W. The management of desmoid tumours: a joint global consensus-based guideline approach for adult and paediatric patients. Eur. J. Cancer 127, 96–107 (2020).
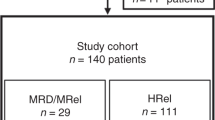
Sparber-Sauer, M., Seitz, G., von Kalle, T., Vokuhl, C., Leuschner, I., Scheer, M. et al. Systemic therapy of aggressive fibromatosis in children and adolescents: report of the Cooperative Weichteilsarkom Studiengruppe (CWS). Pediatr. Blood Cancer 65, e26943 (2018).
Skapek, S. X., Anderson, J. R., Hill, D. A., Henry, D., Spunt, S. L., Meyer, W. et al. Safety and efficacy of high-dose tamoxifen and sulindac for desmoid tumor in children: results of a Children’s Oncology Group (COG) phase II study. Pediatr. Blood Cancer 60, 1108–1112 (2013).
Ferrari, A., Orbach, D., Affinita, M. C., Chiaravalli, S., Corradini, N., Meazza, C. et al. Evidence of hydroxyurea activity in children with pretreated desmoid-type fibromatosis: a new option in the armamentarium of systemic therapies. Pediatr. Blood Cancer 66, e27472 (2019).
Constantinidou, A., Jones, R. L., Scurr, M., Al-Muderis, O. & Judson, I. Pegylated liposomal doxorubicin, an effective, well-tolerated treatment for refractory aggressive fibromatosis. Eur. J. Cancer 45, 2930–2934 (2009).
Crago, A. M., Chmielecki, J., Rosenberg, M., O’Connor, R., Byrne, C., Wilder, F. G. et al. Near universal detection of alterations in CTNNB1 and Wnt pathway regulators in desmoid-type fibromatosis by whole-exome sequencing and genomic analysis. Genes Chromosomes Cancer 54, 606–615 (2015).
Zambo, I. & Vesely, K. WHO classification of tumours of soft tissue and bone 2013: the main changes compared to the 3rd edition. Cesk Patol. 50, 64–70 (2014).
Coindre, J. M. New WHO classification of tumours of soft tissue and bone. Ann. Pathol. 32, S115–S116 (2012).
Li, C., Bapat, B. & Alman, B. A. Adenomatous polyposis coli gene mutation alters proliferation through its beta-catenin-regulatory function in aggressive fibromatosis (desmoid tumor). Am. J. Pathol. 153, 709–714 (1998).
Enzo, M. V., Rastrelli, M., Rossi, C. R., Hladnik, U. & Segat, D. The Wnt/beta-catenin pathway in human fibrotic-like diseases and its eligibility as a therapeutic target. Mol. Cell Ther. 3, 1 (2015).
Matono, H., Tamiya, S., Yokoyama, R., Saito, T., Iwamoto, Y., Tsuneyoshi, M. et al. Abnormalities of the Wnt/beta-catenin signalling pathway induce tumour progression in sporadic desmoid tumours: correlation between beta-catenin widespread nuclear expression and VEGF overexpression. Histopathology. 59, 368–375 (2011).
Chugh, R., Wathen, J. K., Patel, S. R., Maki, R. G., Meyers, P. A., Schuetze, S. M. et al. Efficacy of imatinib in aggressive fibromatosis: results of a phase II multicenter sarcoma alliance for research through Collaboration (SARC) trial. Clin. Cancer Res. 16, 4884–4891 (2010).
Heinrich, M. C., Joensuu, H., Demetri, G. D., Corless, C. L., Apperley, J., Fletcher, J. A. et al. Phase II, open-label study evaluating the activity of imatinib in treating life-threatening malignancies known to be associated with imatinib-sensitive tyrosine kinases. Clin. Cancer Res. 14, 2717–2725 (2008).
Heinrich, M. C., McArthur, G. A., Demetri, G. D., Joensuu, H., Bono, P., Herrmann, R. et al. Clinical and molecular studies of the effect of imatinib on advanced aggressive fibromatosis (desmoid tumor). J. Clin. Oncol. 24, 1195–1203 (2006).
Corless, C. L., Fletcher, J. A. & Heinrich, M. C. Biology of gastrointestinal stromal tumors. J. Clin. Oncol. 22, 3813–3825 (2004).
Maki, R. G., Awan, R. A., Dixon, R. H., Jhanwar, S. & Antonescu, C. R. Differential sensitivity to imatinib of 2 patients with metastatic sarcoma arising from dermatofibrosarcoma protuberans. Int. J. Cancer 100, 623–626 (2002).
Fields, R. C., Hameed, M., Qin, L. X., Moraco, N., Jia, X., Maki, R. G. et al. Dermatofibrosarcoma protuberans (DFSP): predictors of recurrence and the use of systemic therapy. Ann. Surg. Oncol. 18, 328–336 (2011).
Blay, J. Y., El Sayadi, H., Thiesse, P., Garret, J. & Ray-Coquard, I. Complete response to imatinib in relapsing pigmented villonodular synovitis/tenosynovial giant cell tumor (PVNS/TGCT). Ann. Oncol. 19, 821–822 (2008).
Penel, N., Le Cesne, A., Bui, B. N., Perol, D., Brain, E. G., Ray-Coquard, I. et al. Imatinib for progressive and recurrent aggressive fibromatosis (desmoid tumors): an FNCLCC/French Sarcoma Group phase II trial with a long-term follow-up. Ann. Oncol. 22, 452–457 (2011).
Kasper, B., Gruenwald, V., Reichardt, P., Bauer, S., Rauch, G., Limprecht, R. et al. Imatinib induces sustained progression arrest in RECIST progressive desmoid tumours: final results of a phase II study of the German Interdisciplinary Sarcoma Group (GISG). Eur. J. Cancer 76, 60–67 (2017).
Desmoid Tumor Working Group. The management of desmoid tumours: a joint global consensus-based guideline approach for adult and paediatric patients. Eur. J. Cancer 127, 96–107 (2020).
Kroschwald, L. M., Tauer, J. T., Kroschwald, S. I., Suttorp, M., Wiedenfeld, A., Beissert, S. et al. Imatinib mesylate and nilotinib decrease synthesis of bone matrix in vitro. Oncol. Lett. 18, 2102–2108 (2019).
Suttorp, M., Metzler, M., Millot, F., Shimada, H., Bansal, D., Gunes, A. M. et al. Generic formulations of imatinib for treatment of Philadelphia chromosome-positive leukemia in pediatric patients. Pediatr. Blood Cancer 65, e27431 (2018).
Suttorp, M., Schulze, P., Glauche, I., Gohring, G., von Neuhoff, N., Metzler, M. et al. Front-line imatinib treatment in children and adolescents with chronic myeloid leukemia: results from a phase III trial. Leukemia. 32, 1657–1669 (2018).
Suttorp, M., Bornhauser, M., Metzler, M., Millot, F. & Schleyer, E. Pharmacology and pharmacokinetics of imatinib in pediatric patients. Expert Rev. Clin. Pharmacol. 11, 219–231 (2018).
Proschmann, R., Baldow, C., Rothe, T., Suttorp, M., Thiede, C., Tauer, J. T. et al. Response dynamics of pediatric patients with chronic myeloid leukemia on imatinib therapy. Haematologica. 102, e39–e42 (2017).
Kroschwald, L., Suttorp, M., Tauer, J. T., Zimmermann, N., Gunther, C. & Bauer, A. Offtarget effect of imatinib and nilotinib on human vitamin D3 metabolism. Mol. Med. Rep. 17, 1382–1388 (2018).
Yin, X. F., Wang, J. H., Li, X., Yu, M. X., Ma, Z. X. & Jin, J. Incidence of second malignancies of chronic myeloid leukemia during treatment with tyrosine kinase inhibitors. Clin. Lymphoma Myeloma Leuk. 16, 577–581 (2016).
Choeyprasert, W., Yansomdet, T., Natesirinilkul, R., Wejaphikul, K. & Charoenkwan, P. Adverse effects of imatinib in children with chronic myelogenous leukemia. Pediatr. Int. 59, 286–292 (2017).
Samis, J., Lee, P., Zimmerman, D., Arceci, R. J., Suttorp, M. & Hijiya, N. Recognizing endocrinopathies associated with tyrosine kinase inhibitor therapy in children with chronic myelogenous leukemia. Pediatr. Blood Cancer 63, 1332–1338 (2016).
Tauer, J. T., Hofbauer, L. C., Jung, R., Gerdes, S., Glauche, I., Erben, R. G. et al. Impact of long-term exposure to the tyrosine kinase inhibitor imatinib on the skeleton of growing rats. PLoS ONE 10, e0131192 (2015).
Ulmer, A., Tabea Tauer, J., Glauche, I., Jung, R. & Suttorp, M. TK inhibitor treatment disrupts growth hormone axis: clinical observations in children with CML and experimental data from a juvenile animal model. Klin. Padiatr. 225, 120–126 (2013).
Jaeger, B. A., Tauer, J. T., Ulmer, A., Kuhlisch, E., Roth, H. J. & Suttorp, M. Changes in bone metabolic parameters in children with chronic myeloid leukemia on imatinib treatment. Med. Sci. Monit. 18, CR721–CR728 (2012).
Hosokawa, T., Hara, T., Arakawa, Y., Oguma, E. & Yamada, Y. Periosteal reaction possibly induced by pazopanib: a case report and literature review. J. Pediatr. Hematol. Oncol. 42, e822–e825 (2020).
Wang, E., DuBois, S. G., Wetmore, C. & Khosravan, R. Population pharmacokinetics-pharmacodynamics of sunitinib in pediatric patients with solid tumors. Cancer Chemother. Pharmacol. 86, 181–192 (2020).
Jo, J. C., Hong, Y. S., Kim, K. P., Lee, J. L., Lee, J., Park, Y. S. et al. A prospective multicenter phase II study of sunitinib in patients with advanced aggressive fibromatosis. Investig. New Drugs 32, 369–376 (2014).
Wang, E., DuBois, S. G., Wetmore, C. & Khosravan, R. Population pharmacokinetics-pharmacodynamics of sunitinib in pediatric patients with solid tumors. Cancer Chemother. Pharmacol. 86, 181–192 (2020).
van der Graaf, W. T., Blay, J. Y., Chawla, S. P., Kim, D. W., Bui-Nguyen, B., Casali, P. G. et al. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 379, 1879–1886 (2012).
Szucs, Z., Messiou, C., Wong, H. H., Hatcher, H., Miah, A., Zaidi, S. et al. Pazopanib, a promising option for the treatment of aggressive fibromatosis. Anticancer Drugs 28, 421–426 (2017).
Bulut, G., Ozluk, A., Erdogan, A. P., Uslu, R., Elmas, N. & Karaca, B. Pazopanib: a novel treatment option for aggressive fibromatosis. Clin. Sarcoma Res. 6, 22 (2016).
Martin-Liberal, J., Benson, C., McCarty, H., Thway, K., Messiou, C. & Judson, I. Pazopanib is an active treatment in desmoid tumour/aggressive fibromatosis. Clin. Sarcoma Res. 3, 13 (2013). 26.
Nishida, Y., Sakai, T., Koike, H. & Ito, K. Pazopanib for progressive desmoid tumours: children, persistant effects, and cost. Lancet Oncol. 20, e555 (2019).
Glade Bender, J. L., Lee, A., Reid, J. M., Baruchel, S., Roberts, T., Voss, S. D. et al. Phase I pharmacokinetic and pharmacodynamic study of pazopanib in children with soft tissue sarcoma and other refractory solid tumors: a children’s oncology group phase I consortium report. J. Clin. Oncol. 31, 3034–3043 (2013).
Weiss, A. R., Chen, Y. L., Scharschmidt, T. J., Chi, Y. Y., Tian, J., Black, J. O. et al. Pathological response in children and adults with large unresected intermediate-grade or high-grade soft tissue sarcoma receiving preoperative chemoradiotherapy with or without pazopanib (ARST1321): a multicentre, randomised, open-label, phase 2 trial. Lancet Oncol. 21, 1110–1122 (2020).
Gounder, M. M., Lefkowitz, R. A., Keohan, M. L., D’Adamo, D. R., Hameed, M., Antonescu, C. R. et al. Activity of sorafenib against desmoid tumor/deep fibromatosis. Clin. Cancer Res. 17, 4082–4090 (2011).
Walko, C. M., Aubert, R. E., La-Beck, N. M., Clore, G., Herrera, V., Kourlas, H. et al. Pharmacoepidemiology of clinically relevant hypothyroidism and hypertension from sunitinib and sorafenib. Oncologist 22, 208–212 (2017).
Widemann, B. C., Kim, A., Fox, E., Baruchel, S., Adamson, P. C., Ingle, A. M. et al. A phase I trial and pharmacokinetic study of sorafenib in children with refractory solid tumors or leukemias: a Children’s Oncology Group Phase I Consortium report. Clin. Cancer Res. 18, 6011–6022 (2012).
Kim, A., Widemann, B. C., Krailo, M., Jayaprakash, N., Fox, E., Weigel, B. et al. Phase 2 trial of sorafenib in children and young adults with refractory solid tumors: a report from the Children’s Oncology Group. Pediatr. Blood Cancer 62, 1562–1566 (2015).
Kim, A., Dombi, E., Tepas, K., Fox, E., Martin, S., Wolters, P. et al. Phase I trial and pharmacokinetic study of sorafenib in children with neurofibromatosis type I and plexiform neurofibromas. Pediatr. Blood Cancer 60, 396–401 (2013).
Navid, F., Baker, S. D., McCarville, M. B., Stewart, C. F., Billups, C. A., Wu, J. et al. Phase I and clinical pharmacology study of bevacizumab, sorafenib, and low-dose cyclophosphamide in children and young adults with refractory/recurrent solid tumors. Clin Cancer Res. 19, 236–246 (2013).
Karajannis, M. A., Legault, G., Fisher, M. J., Milla, S. S., Cohen, K. J., Wisoff, J. H. et al. Phase II study of sorafenib in children with recurrent or progressive low-grade astrocytomas. Neuro Oncol. 16, 1408–1416 (2014).
Inaba, H., Panetta, J. C., Pounds, S. B., Wang, L., Li, L., Navid, F. et al. Sorafenib population pharmacokinetics and skin toxicities in children and adolescents with refractory/relapsed leukemia or solid tumor malignancies. Clin. Cancer Res. 25, 7320–7330 (2019).
Skapek, S. X., Ferguson, W. S., Granowetter, L., Devidas, M., Perez-Atayde, A. R., Dehner, L. P. et al. Vinblastine and methotrexate for desmoid fibromatosis in children: results of a Pediatric Oncology Group Phase II Trial. J. Clin. Oncol. 25, 501–506 (2007).
Federico, S. M., Caldwell, K. J., McCarville, M. B., Daryani, V. M., Stewart, C. F., Mao, S. et al. Phase I expansion cohort to evaluate the combination of bevacizumab, sorafenib and low-dose cyclophosphamide in children and young adults with refractory or recurrent solid tumours. Eur. J. Cancer 132, 35–42 (2020).
Okada, K., Nakano, Y., Yamasaki, K., Nitani, C., Fujisaki, H. & Hara, J. Sorafenib treatment in children with relapsed and refractory neuroblastoma: an experience of four cases. Cancer Med. 5, 1947–1949 (2016).
Paul, A., Blouin, M. J., Minard-Colin, V., Galmiche, L., Coulomb, A., Corradini, N. et al. Desmoid-type fibromatosis of the head and neck in children: a changing situation. Int. J. Pediatr. Otorhinolaryngol. 123, 33–37 (2019).
Crombe, A., Kind, M., Ray-Coquard, I., Isambert, N., Chevreau, C., Andre, T. et al. Progressive desmoid tumor: radiomics compared with conventional response criteria for predicting progression during systemic therapy—a multicenter study by the French Sarcoma Group. Am. J. Roentgenol. 215, 1539–1548 (2020).
Sheth, P. J., Del Moral, S., Wilky, B. A., Trent, J. C., Cohen, J., Rosenberg, A. E. et al. Desmoid fibromatosis: MRI features of response to systemic therapy. Skeletal Radiol. 45, 1365–1373 (2016).
Macagno, N., Fina, F., Penel, N., Bouvier, C., Nanni, I., Duffaud, F. et al. Proof of concept: prognostic value of the plasmatic concentration of circulating cell free DNA in desmoid tumors using ddPCR. Oncotarget 9, 18296–18308 (2018).
Acknowledgements
Authors want to thank the ‘SOS Desmoid association' for the review of the manuscript.
Author information
Authors and Affiliations
Contributions
M.S.S., D.O. and A.F.: conceptualisation, formal analysis, methodology, writing and editing; F.N., S.H., S.S., N.C., M.C., A.W. and M.S.: formal analysis, methodology, writing and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publish
Not applicable.
Data availability
Not applicable.
Competing interests
The authors declare no conflict of interest in relation with this manuscript. M.S. is supported by the Robert Bosch Stiftung, Stuttgart, Germany.
Funding information
No specific funding.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sparber-Sauer, M., Orbach, D., Navid, F. et al. Rationale for the use of tyrosine kinase inhibitors in the treatment of paediatric desmoid-type fibromatosis. Br J Cancer 124, 1637–1646 (2021). https://doi.org/10.1038/s41416-021-01320-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01320-1
This article is cited by
-
The Role of Pharmacotherapeutic Agents in Children with Desmoid Tumors
Pediatric Drugs (2022)