Abstract
Background
This study aimed to evaluate the prognostic value of pre-treatment NLR in patients with oropharyngeal cancer.
Methods
Patients who completed definitive radiotherapy (RT) for oropharyngeal cancer and had blood counts taken pre-RT from 2002 to 2013 were included. NLR was calculated as total neutrophil/lymphocytes. Survival rates were estimated using the Kaplan–Meier method. Univariable and multivariable analyses were conducted with linear and Cox regression methods. NLR was analysed posteriori and dichotomised on the discovered median.
Results
Eight hundred and forty-eight patients were analysed. The median pre-RT NLR was 3. Patients with NLR of <3 had improved overall survival (OS) than those with NLR ≥ 3 (5-year OS 85 vs 74%, p < 0.0001). OS differences remained significant when stratified according to HPV status (HPV-positive p = 0.011; HPV-negative p = 0.003). Freedom from any recurrence (FFR), locoregional control (LRC) and freedom of distant recurrence (FDR) were better in those with NLR < 3. The negative impact of elevated pre-RT NLR on OS (HR = 1.64, p = 0.001), FFR (HR = 1.6, p = 0.006) and LRC (HR = 1.8, p = 0.005) remained significant on multivariable analysis.
Conclusions
Pre-RT NLR is an independent prognostic factor in patients with oropharyngeal cancer regardless of HPV status. Patients with lower NLR had more favourable OS and disease control.
Similar content being viewed by others
Background
The incidence of oropharyngeal cancer is on the rise in the developed countries.1 As human papillomavirus (HPV) is an infectious agent, there is renewed interest to investigate the extent of host’s inflammatory reaction to the persistent HPV infection contributing to neoplastic transformation, cancer treatment response and patient’s prognosis. While inflammation can be protective against malignancy in the initial phase, activating the innate immune system and recruiting primitive immune cells such as neutrophils to the site is attributed to promote tumorigenesis and cancer progression.2 It is postulated that chronic inflammation promotes quick turnover of cells, thereby accumulating and propagating mutations contributing to malignant transformation. In addition, the inflammatory cascade leads to capillary leakiness potentially promoting tumour angiogenesis and metastatic potential.
Neutrophil-to-lymphocyte ratio (NLR) is a simple biomarker of systemic inflammation and has been demonstrated to be a prognostic marker in several solid cancers, including prostate,3 renal,4 gastric,5 brain6 and hypopharyngeal7 cancers. Here we evaluated the effect of pre-treatment NLR on outcomes in patients with oropharyngeal cancer in the contemporary era.
Methods
This retrospective study was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center. This study was performed in accordance with the Declaration of Helsinki. All patients, above the age of 18 years, who completed curative-intent radiotherapy for squamous cell carcinoma of the oropharynx and had blood counts taken within 2 weeks before radiotherapy from 2002 to 2013 were included in this study. All patients received curative-intent radiation dose. Patients with distant metastatic disease (M1) at diagnosis, had no blood counts taken within 2 weeks of commencing radiotherapy or had a haematologic disorder affecting lymphocyte and/or neutrophil counts were excluded. Patient, tumour and treatment characteristics, clinical outcomes and pre-radiotherapy total neutrophil and lymphocyte counts (TNC and TLC, respectively) were recorded. HPV status was collected, whenever available, and is deemed positive if either p16 immunohistochemistry or HPV in situ hybridisation was positive. The disease was staged according to the American Joint Committee on Cancer (AJCC) staging system (Seventh edition). NLR was calculated as TNC divided by TLC. NLR was analysed posteriori and dichotomised on the discovered median (rounded to nearest whole number).
Statistical analysis
Overall survival (OS) was calculated with the Kaplan–Meier method from the date of completion of radiotherapy to date of death. Freedom from locoregional failure was measured from the date of completion of radiotherapy to the date of first locoregional failure. Freedom from distant metastasis was calculated from the date of completion of radiotherapy to the date of first distant disease. Freedom from recurrence was calculated from the date of completion of radiotherapy to the date of any first recurrence. For all survival calculations, patients without events were censored at last follow-up time.
The impact of NLR on survival and disease control rates was estimated using the Kaplan–Meier method and compared with log-rank tests. Potential prognostic factors for OS and freedom from recurrence were evaluated with univariable and multivariable analyses and were conducted with linear and Cox proportional hazard regression models. Variables that achieved a p value of ≤0.1 in univariable analyses were included in the multivariable analysis. A two-tailed p value of <0.05 was deemed statistically significant. Statistical analyses were performed using JMP v14.0 (SAS Institute Inc.).
Results
Patient characteristics
From 2002 to 2013, 1124 patients with localised oropharyngeal cancer received definitive radiotherapy. Of these, 276 patients were excluded from this analysis: 273 patients did not have a blood count within 2 weeks of commencing radiotherapy, 2 had chronic lymphocytic leukaemia, and 1 had a spurious high neutrophil count. Therefore, a total of 848 patients were eligible for analysis. Table 1 summarises the patient, disease and treatment characteristics. The median age of the cohort was 57 years (range: 29–87 years). The majority (87%) were males and approximately half the cohort were never smokers or previous smokers with <10 pack year history. Base of tongue and tonsil were the predominant sites accounting for 98% of the cohort primary site. Six hundred and three (71%) patients had HPV/p16-positive squamous cell carcinoma. The median radiation dose fractionation delivered was 70 Gy in 33 fractions. Almost half the cohort received induction chemotherapy and 88% had concurrent chemotherapy.
Pre-treatment NLR and outcomes
The median pre-treatment NLR was 2.52 (range: 0.05–23.9). The median follow-up time was 59 months (range: 6–153 months). At last follow-up, 183 (22%) patients had died. Overall, 141 (17%) patients developed disease recurrence: 70 with distant disease (including 11 with local and/or regional disease, 37 with local disease, 29 with regional disease, and 5 with local and regional disease.
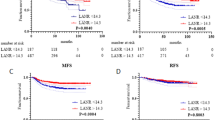
Patients with NLR < 3 had a 5-year OS of 85% compared to 74% (p < 0.0001) for those with NLR ≥ 3. Freedom from recurrence, locoregional failure and distant metastasis were better in those with NLR < 3 (5-year freedom from recurrence 86 vs 77%, p = 0.0009; 5-year freedom from locoregional failure 92 vs 85%, p = 0.003; 5-year freedom from distant metastasis 91 vs 86%, p = 0.038; Fig. 1). To verify that our results were not influenced by outliers, we re-analysed the data with just the patients whose NLR was in the 5–95% values (range: 0.95–7.97). This demonstrated that the improved outcomes in those with NLR < 3, as shown in the overall cohort analysis, remained significant.
Stratification by HPV status
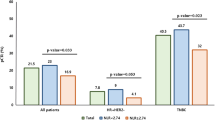
HPV status was available for 674 patients—603 HPV positive and 71 HPV negative. When stratified according to HPV status, those with NLR < 3 continued to have a significantly better OS than those with NLR ≥ 3 (HPV positive: 5-year OS 85 vs 78%, p = 0.011; HPV negative: 5-year OS 88 vs 61%, p = 0.003; Fig. 2). Similar effect is observed for freedom from recurrence (HPV positive: 5-year 86 vs 80%, p = 0.036; HPV negative: 5-year 84 vs 69%, p = 0.051). On logistic regression analysis, there was association between NLR and T stage (p = 0.0003) and N stage (p = 0.002) but no significant association with HPV status (p = 0.75) nor smoking status (p = 0.88). Figure 3 shows the impact of combined T stage and NLR on OS.
Univariable and multivariable analyses
Univariable analyses of variable of interest are shown in Table 2. On multivariable analyses, NLR remained as an independent prognostic factor for OS and freedom from recurrence with NLR ≥ 3 having a risk ratio of 1.64 (95% confidence interval (CI) 1.22–2.19, p = 0.001) and 1.62 (95% CI 1.15–2.26, p = 0.006), respectively. In addition to NLR, patient’s smoking status, age and T stage were also associated with OS outcome. Radiation dose (higher dose) and NLR < 3 were associated with improved freedom from recurrence.
To determine whether the effect of NLR is relatively linear as an overall continuous degree of inflammation, NLR was analysed as a continuous variable. On univariable analysis, lower NLR was associated with better freedom from recurrence (p = 0.003, HR = 1.04, 95% CI = 1.01–1.06) and locoregional failure (p = 0.007, HR = 1.05, 95% CI = 1.01–1.07). However, NLR as a continuous variable had no significant correlation with OS (p = 0.37) and freedom from distant metastasis (p = 0.92).
Discussion
Our study which consisted of a large cohort of patients with squamous cell carcinoma of the oropharynx demonstrated that the pre-radiotherapy NLR has significant impact on OS and disease control. Patients with NLR of <3 before radiotherapy had an improved 5-year survival of 85% compared to 74% in those with NLR of 3. The impact of NLR on clinical outcomes was independent of HPV status.
NLR is a simple inflammatory marker that has been proven to be a prognostic marker in multiple malignancies.3,4,5,6,8 A large meta-analysis reporting on a 100 studies with >40,000 patients demonstrated that patients with solid tumours and a higher NLR (>4) had worse OS and disease outcomes, regardless of cancer stage or subsites.8 In head and neck cancer, NLR has been extensively investigated as a prognostic marker although variable cut-off values and timepoints were used.7,9,10,11,12,13,14,15 The majority of studies have included a heterogeneous group of patients with tumours from differing head and neck subsites.7,11,13,14,15,16 More recently, in a smaller study than ours, So et al.12 reported on a cohort of 104 patients with HPV-associated oropharyngeal cancer and showed that patients with high NLR had worse 5-year disease-free survival. In patients with HPV-negative disease, Lin et al.17 reported that an elevated NLR at 3 months after completion of radiotherapy was associated with worse survival. Our study results are consistent with previous literature and provide a validation for the use of pre-treatment NLR as a prognostic marker in a contemporary cohort of patients with oropharyngeal cancer.
The relationship between inflammation and cancer has become an increasingly interesting but intricate area of research. Although inflammation has been identified as one of the hallmarks of cancer,18 the complex relationship between inflammation and the tumour microenvironment, promoting angiogenesis and malignant transformation and subsequently cancer progression, remain poorly understood. While HPV is now identified as a cause of oropharyngeal cancer, our study has shown that NLR remained as an effective prognostic biomarker regardless of viral status. One might assume that the persistent HPV infection releases pro-inflammatory cytokines resulting in chronic inflammation and subsequently carcinogenesis. However, it appears that the inflammatory tumour microenvironment may differ between HPV-positive and HPV-negative tumours, as patients with HPV-positive oropharyngeal cancer have improved outcomes compared to those with HPV-negative cancer. For example, it has been noted that patients with HPV-positive oropharyngeal cancer tend to have radiologically cystic or necrotic neck nodes19,20 compared to those with HPV-negative disease. Necrosis is proinflammatory and can recruit immune cells to the area with the intent of clearing the necrotic debris.18 Although the intent of inflammatory infiltrate is to remove debris and promote healing, interleukin-1α released by necrotic cells for cell proliferation can inadvertently expedite neoplastic transformation and progression.21
Our study comes with caveats of a single institution retrospective cohort study. Second, relative to those with HPV-positive disease, the number of patients with HPV-negative oropharyngeal cancer in this cohort is only 71 (8.4%), thereby limiting the statistical power and further analysis to determine the impact of NLR on disease-specific outcomes due to the small number of events. Third, although we reported the number of patients who received induction and concurrent chemotherapy, we did not detail the chemotherapeutic agents. The vast majority who received induction chemotherapy received taxane–platinum-based regimens, while our concurrent patients received single agent platin or cetuximab. Nevertheless, our results are consistent with the previous studies in head and neck and other cancers indicating that NLR, as a marker of systemic inflammation, is prognostic for clinical outcomes.
In this large cohort of patients with oropharyngeal cancer, we highlighted that pre-radiotherapy NLR is an independent prognostic factor in patients with oropharyngeal cancer regardless of HPV status. Patients with lower NLR had more favourable clinical outcomes in terms of survival and disease control. NLR could be explored prospectively as a potential cost-effective biomarker for further pre-treatment risk stratification of patients with oropharyngeal cancer for treatment de-escalation/escalation.
References
Chaturvedi, A. K., Anderson, W. F., Lortet-Tieulent, J., Curado, M. P., Ferlay, J., Franceschi, S. et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J. Clin. Oncol. 31, 4550–4559 (2013).
Coussens, L. M. & Werb, Z. Inflammation and cancer. Nature 420, 860–867 (2002).
Conteduca, V., Crabb, S. J., Jones, R. J., Caffo, O., Elliott, T., Scarpi, E. et al. Persistent neutrophil to lymphocyte ratio >3 during treatment with enzalutamide and clinical outcome in patients with castration-resistant prostate cancer. PLoS ONE 11, e0158952 (2016).
Kim, T. W., Lee, J. H., Shim, K. H., Choo, S. H., Choi, J. B., Ahn, H. S. et al. Prognostic significance of preoperative and follow-up neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with non-metastatic clear cell renal cell carcinoma. Investig. Clin. Urol. 60, 14–20 (2019).
Choi, J. H., Suh, Y. S., Choi, Y., Han, J., Kim, T. H., Park, S. H. et al. Comprehensive analysis of the neutrophil-to-lymphocyte ratio for preoperative prognostic prediction nomogram in gastric cancer. World J. Surg. 42, 2530–2541 (2018).
Mason, M., Maurice, C., McNamara, M. G., Tieu, M. T., Lwin, Z., Millar, B. A. et al. Neutrophil-lymphocyte ratio dynamics during concurrent chemo-radiotherapy for glioblastoma is an independent predictor for overall survival. J. Neurooncol. 132, 463–471 (2017).
Kuo, C., Hsueh, W. T., Wu, Y. H., Yang, M. W., Cheng, Y. J., Pao, T. H. et al. The role of pretreatment serum neutrophil-to-lymphocyte ratio in hypopharyngeal cancer treated with definitive chemoradiotherapy: a pilot study. Sci. Rep. 9, 1618 (2019).
Templeton, A. J., McNamara, M. G., Seruga, B., Vera-Badillo, F. E., Aneja, P., Ocana, A. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl Cancer Inst. 106, dju124 (2014).
Takenaka, Y., Oya, R., Kitamiura, T., Ashida, N., Shimizu, K., Takemura, K. et al. Prognostic role of neutrophil-to-lymphocyte ratio in head and neck cancer: a meta-analysis. Head Neck 40, 647–655 (2018).
Charles, K. A., Harris, B. D., Haddad, C. R., Clarke, S. J., Guminski, A., Stevens, M. et al. Systemic inflammation is an independent predictive marker of clinical outcomes in mucosal squamous cell carcinoma of the head and neck in oropharyngeal and non-oropharyngeal patients. BMC Cancer 16, 124 (2016).
Cho, Y. Kim, J. W., Yoon, H. I., Lee, C. G., Keum, K. C. & Lee, I. J. The prognostic significance of neutrophil-to-lymphocyte ratio in head and neck cancer patients treated with radiotherapy. J. Clin. Med. https://doi.org/10.3390/jcm7120512 (2018).
So, Y. K., Lee, G., Oh, D., Byeon, S., Park, W. & Chung, M. K. Prognostic role of neutrophil-to-lymphocyte ratio in patients with human papillomavirus-positive oropharyngeal cancer. Otolaryngol. Head Neck Surg. 159, 303–309 (2018).
Chandrasekara, S., Davis, S., Thomson, P. & Haydon, A. High neutrophil-to-lymphocyte ratio predicts poor prognosis in patients with squamous cell carcinoma of the head and neck treated with definitive chemoradiotherapy. Asia Pac. J. Clin. Oncol. 14, e442–e447 (2018).
Bojaxhiu, B., Templeton, A. J., Elicin, O., Shelan, M., Zaugg, K., Walser, M. et al. Relation of baseline neutrophil-to-lymphocyte ratio to survival and toxicity in head and neck cancer patients treated with (chemo-) radiation. Radiat. Oncol. 13, 216 (2018).
Kim, D. Y., Kim, I. S., Park, S. G., Kim, H., Choi, Y. J. & Seol, Y. M. Prognostic value of posttreatment neutrophil-lymphocyte ratio in head and neck squamous cell carcinoma treated by chemoradiotherapy. Auris Nasus Larynx 44, 199–204 (2017).
Cho, J. K., Kim, M. W., Choi, I. S., Moon, U. Y., Kim, M. J., Sohn, I. et al. Optimal cutoff of pretreatment neutrophil-to-lymphocyte ratio in head and neck cancer patients: a meta-analysis and validation study. BMC Cancer 18, 969 (2018).
Lin, A. J., Gang, M., Rao, Y. J., Campian, J., Daly, M., Gay, H. et al. Association of posttreatment lymphopenia and elevated neutrophil-to-lymphocyte ratio with poor clinical outcomes in patients with human papillomavirus-negative oropharyngeal cancers. JAMA Otolaryngol. Head Neck Surg. 145, 413–421 (2019).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Goldenberg, D., Begum, S., Westra, W. H., Khan, Z., Sciubba, J., Pai, S. I. et al. Cystic lymph node metastasis in patients with head and neck cancer: an HPV-associated phenomenon. Head Neck 30, 898–903 (2008).
Tang, C., Fuller, C. D., Garden, A. S., Awan, M. J., Colen, R. R., Morrison, W. H. et al. Characteristics and kinetics of cervical lymph node regression after radiation therapy for human papillomavirus-associated oropharyngeal carcinoma: quantitative image analysis of post-radiotherapy response. Oral. Oncol. 51, 195–201 (2015).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140, 883–899 (2010).
Author information
Authors and Affiliations
Contributions
S.P.N.: conceptualisation, data curation, formal analysis, investigation, methodology, project administration, visualisation, writing—original draft, and writing—review and editing. H.B.: data curation, investigation, visualisation, and writing—review and editing. A.J.: data curation and writing—review and editing. E.M.S., F.M.J., G.B.G., R.F., J.P., D.I.R., S.J.F. and C.D.F.: resources, methodology, and writing—review and editing. B.E.: methodology and writing—review and editing. A.S.G.: supervision, project administration, resources, writing—original draft, and writing—review and editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center. Informed consent was waived. This study was performed in accordance with the Declaration of Helsinki.
Consent to publish
Not applicable.
Data availability
Data will be available on request.
Competing interests
The authors declare no competing interests.
Funding information
S.P.N. is funded by the Australian Postgraduate Award, the Royal Australian and New Zealand College of Radiologists (RANZCR) Research Grant and the Radiological Society of North America (RSNA) Fellow Grant. C.D.F. was supported by Andrew Sabin Family Fellowship. C.D.F. received funding support from the National Institutes of Health (NIH)/National Institute for Dental and Craniofacial Research (NIDCR) (1R01DE025248-01/R56DE025248-01). C.D.F. was previously funded via the National Science Foundation (NSF), Division of Mathematical Sciences, Joint NIH/NSF Initiative on Quantitative Approaches to Biomedical Big Data (QuBBD) Grant (NSF DMS-1557679) and is currently supported by the NIH National Cancer Institute (NCI)/Big Data to Knowledge (BD2K) Program (1R01CA214825-01), the NIH/NCI Head and Neck Specialized Programs of Research Excellence (SPORE) Developmental Research Program Career Development Award (P50CA097007-10); the NCI Paul Calabresi Clinical Oncology Program Award (K12 CA088084-06); a General Electric Healthcare/MD Anderson Center for Advanced Biomedical Imaging In-Kind Award; an Elekta AB/MD Anderson Department of Radiation Oncology Seed Grant; the Center for Radiation Oncology Research (CROR) at MD Anderson Cancer Center Seed Grant and the MD Anderson Institutional Research Grant (IRG) Program. C.D.F. has received speaker travel funding from Elekta AB. This study was supported in part by the NIH/NCI Cancer Center Support (Core) Grant CA016672 to The University of Texas MD Anderson Cancer Center (P30 CA016672). F.M.J. has received research funding from PIQUR Therapeutics and Trovagene. E.M.S. has a research award from Roche Diagnostics supporting HPV testing of oral rinse and mucosal swab samples on the clinical trial for HPV-related cancers screening in men (HOUSTON study).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Note This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ng, S.P., Bahig, H., Jethanandani, A. et al. Prognostic significance of pre-treatment neutrophil-to-lymphocyte ratio (NLR) in patients with oropharyngeal cancer treated with radiotherapy. Br J Cancer 124, 628–633 (2021). https://doi.org/10.1038/s41416-020-01106-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-01106-x
This article is cited by
-
A predictive model for advanced oropharyngeal cancer patients treated with chemoradiation
BMC Cancer (2022)
-
Recent advances in the oncological management of head and neck cancer and implications for oral toxicity
British Dental Journal (2022)