Abstract
Aims This study aimed to use electronic referral management system (eRMS) oral surgery data across multiple sites in England to evaluate the service over a 34-month period in relation to: 1) pre- and post-pandemic referral rates in oral surgery; 2) examining the data for signs of inequality in obtaining a referral for oral surgery; and 3) considering the impact on service provision for oral surgery in England.
Methods Oral surgery referral data were available from an eRMS for areas of England covered by this service for the 34-month period of March 2019 to December 2021 (inclusive), which included 12 months of pre-pandemic data and the first 22 months of the pandemic. The data were from the following regions in England: Central Midlands; Cheshire and Merseyside; East Anglia and Essex; Greater Manchester; Lancashire; Thames Valley; and Yorkshire and the Humber.
Results The total number of referrals received was 1,766,895 during this 34-month period, with pre-pandemic referral levels averaging at 25,498 per month, with a reduction to 698 per month in April 2020. Referrals have risen to a peak of 217,646 for the month of November 2021. An average of 1.5% of referrals were rejected pre-pandemic, compared with 2.7% per month post-pandemic.
Discussion Pre-pandemic referral numbers were predictably stable within a narrow range which have then increased dramatically post-pandemic. The variations in oral surgery referral patterns place significant strain on oral surgery services across England. This not only has consequences on the patient experience, but also on workforce and workforce development, to ensure that there is not a long-term destabilising impact.
Conclusion Analysis of 1.75 million referrals to oral surgery services in England has highlighted the ongoing impact of the pandemic and the need to actively minimise adverse impacts on patients, NHS services and the workforce.
Key points
-
Between March 2019 and December 2021, over 1.75 million oral surgery referrals were received through an electronic referral management system to intermediate minor oral surgery and secondary care oral surgery providers.
-
The first lockdown during the COVID-19 pandemic demonstrated an immediate drop in referrals from an average of 25,498 per month before the pandemic, to 10,573 during the pandemic, and a peak of 217,646 in November 2021.
-
An increase in the number of oral surgery referrals demonstrates a need for workforce development in the speciality in both primary and secondary care.
Similar content being viewed by others
Introduction
The COVID-19 pandemic was declared by the World Health Organisation on 11 March 2020, after the first report of a case of pneumonia on 31 December 2019 in Wuhan, China. Following a rapid spread of the disease throughout the world, lockdown measures in England legally came into force on 26 March 2020. Fears that the SARS-CoV-2 virus could be spread in dental aerosol-generating procedures drove cessation of face-to-face routine and non-urgent dental care in England on 25 March 2020.1 Patient telephone triage was carried out with advice, analgesia and/or antibiotics (AAA) as first line treatment unless patients were acutely unwell, in which case they were referred to urgent dental care clinics (UDCs). Guidance was issued by the British Association of Oral Surgeons and the British Association of Oral and Maxillofacial Surgeons on the management of patients requiring oral surgery treatment.2 Oral surgery services in secondary care were suspended in many units, with staff deployed to support colleagues in medical specialties, particularly critical care;3 therefore, patients' access to oral surgery care was markedly and rapidly reduced. This was a similar situation with paediatric general anaesthetic operating lists for exodontia.4
A standard operating procedure was released by the Chief Dental Officer for England in preparation for dental practices returning to face-to-face care from early June 2020.1 Thereafter, the capacity of dental practices to deliver care has increased but without a return to pre-pandemic levels. Secondary care oral surgery service capacity has also increased over time, but ongoing operational pressures are having a detrimental impact on service provision. For patients who need oral surgery care, the pandemic disruption translates to a reduction in access to primary care and where needed to secondary care also. As secondary care services plan their recovery to make best use of the resources available to them, there is a need to understand the impact of pandemic disruption on oral surgery referrals to secondary care.
Aims
This study aimed to use the electronic referral management system (eRMS) oral surgery data across multiple sites in England to evaluate the service over a 34-month period in relation to:
-
Pre- and post-pandemic referral rates in oral surgery
-
Examining the data for signs of inequality in obtaining a referral for oral surgery
-
The impact on service provision for oral surgery in England.
Materials and method
Oral surgery referral data were available from an eRMS for areas of England covered by this service for the 34-month period of March 2019 to December 2021 (inclusive), which included 12 months of pre-pandemic data and the first 22 months of the pandemic. The data were from the following regions in England: Central Midlands; Cheshire and Merseyside; East Anglia and Essex; Greater Manchester; Lancashire; Thames Valley; and Yorkshire and the Humber.
Ethical approval was not required as this was a service evaluation, and no patient identifiable data were included within data export, complying with the Information Commissioner's Office guidelines on secondary use data. Data were exported from the eRMS into Microsoft Excel (Microsoft Corporation, 2018) and the accompanying index of multiple deprivation (IMD) decile for each referral was included at the time of data receipt.
Results
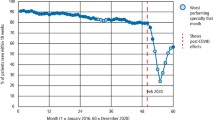
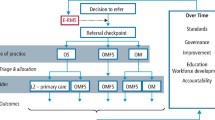
The total number of referrals received to both intermediate minor oral surgery and secondary care in the period March 2019 to December 2021 was 1,766,895, with large changes evident (Fig. 1 and Table 1). Pre-pandemic referrals averaged at 25,498 per month over a 11-month period (March 2019 to February 2020). Referrals reduced in March 2020 to 19,019, with a further reduction to 698 and 747 per month in April and May 2020, respectively. There was a slow but steady increase in referrals from June 2020 (4,692) to October 2020 (16,734), which coincided with dental practices in England resuming face-to-face care. While referral numbers in this period increased, they did not return to pre-pandemic levels. Referrals subsequently increased from 18,089 in February 2021 to 57,573 in March 2021 and continued to rise steeply to a peak in November 2021 of 217,646. Referrals averaged 84,953 per month in the period including August 2020 and December 2021.
Graphical representations of referral numbers through the eRMS per month from March 2019 to December 2021. The data demonstrates the total number of referrals, mean number of referrals pre pandemic (March 2019 to February 2020) and during the pandemic (July 2020 to December 2021), plus the number of referrers per month, with annotations to include key points in the pandemic timeline, such as national lockdowns and easing of restrictions during the study period
Not all referrals received are accepted at the point of clinical triage. The number of rejected referrals were recorded as a percentage compared to the number of referrals received (Fig. 2). Prior to the pandemic, an average of 1.5% of referrals were rejected each month; however, post pandemic, these increased to an average of 2.7% per month. There is a peak of rejected referrals in May 2020, which reached 98% but then dropped to 18% in June 2020.
Geographical representation of referrals. Map demonstrating the volume of referrals from practice postcodes in England. Blue represents low numbers, through the colour spectrum to red being high numbers of referrals. Map from OpenStreetMap. Data is available under the Open Database License (https://www.openstreetmap.org/copyright)
Since the easing of restrictions, there has a reduction in the number of referrers referring patients for oral surgery. Between March 2019 and December 2019, there were an average of 23,539 referrers per month, which has reduced to an average of 14,029 per month since June 2020.
To investigate the distribution and potential inequalities in oral surgery secondary care access via referrals during the first year of the pandemic, the IMD codes were plotted for referrals received over a 24-month period (March 2019 to February 2021, inclusive) (Fig. 2). IMD5 combines information from the seven key domains measured to give an overall relative measure of deprivation during the pandemic. The index ranks every small area in England from the lowest number to the highest. Health deprivation and disability accounts for 13.5% of the index. The lower the rank, the higher the deprivation. This demonstrates that pre-pandemic, the most deprived patients (IMD 3 or less) account for approximately 50% of all referrals. However, in April and May 2020, these increased to 60%, but soon returned within the evaluation period to pre-pandemic levels (Fig. 3).
Discussion
There has been widespread recognition that pandemic disruption to healthcare will be long-lasting and that services will need to plan their way through an extended recovery period that makes the most of the NHS resources available. This is the first report that captures and quantifies the impact of ongoing disruption to pre-pandemic referral patterns for oral surgery care across England through the analyses of 1.75 million referrals. As illustrated in Figure 2, there was broad geographical coverage across England within the dataset; London as the largest city is partially represented. Despite the sampling not being from across all of England, this large dataset was drawn from areas representing a full range of deprivation profiles, thus increasing confidence in the generalisability of the findings. The eRMS captures referrals to NHS services but not to private services.
During 2020, oral surgery (along with orthopaedics and trauma, and ear, nose and throat) was one of three specialties in England with the largest reduction in completed pathways compared to 2019.6 Reduced referral numbers and suspension of treatment pathways can be expected to be major factors on this adverse disruption to pre-pandemic services.
The literature suggests that patients were able to access emergency care, and explanations for the dramatic increase in referrals post pandemic could be due to general dental practitioners having limited clinical time to provide care and therefore are referring more, or patients' oral health has deteriorated during the pandemic due to no ongoing oral health care.
Since the restrictions were imposed on dental care in March 2020 due to the pandemic, there has been a reduction in access to routine dental care for all, which includes those patients seeking treatment for odontogenic infections. There was a delay in the publication of guidance for UDCs following the pandemic, with the key message of AAA. Despite this, however, perhaps due to the effectiveness of UDCs, there appears to have been a reduction7in those patients requiring admission and treatment in secondary care for acute admissions for dento-facial infections. There has been a reported decrease of patients attending oral and maxillofacial departments for dental-related issues with the advent of urgent care centres.8,9 Politi et al.7 reported that during 2020, no patients presented with a post-extraction infection and suggested that this was due to the number of extractions being carried out in UDCs as opposed to general dental practitioners doing so. There was, however, an increase in the percentage of those requiring admission who presented with infection during lockdown. With respect to the management of paediatric patients requiring exodontia under general anaesthesia, during the first two months of lockdown, 1,456 children had their appointments cancelled and although activity resumed later in the year,4 services are insufficient to manage the backlog and continued increase in numbers of children on the waiting list.
In this study, we have demonstrated large changes in referrals to oral surgery services, which at the end of the study period remain very different from pre-pandemic levels. This is within the context that the pandemic would not have an immediate impact on the pattern of clinical disease that would typically trigger an oral surgery referral, given that access to routine care was suspended and therefore patients would develop dental disease over time, which may then require oral surgery care. However, the longer the period of disruption to pre-pandemic patient pathways, there is an increased likelihood of delayed clinical presentations that place an increased burden on the delivery of care in primary care and by specialist services.
The data reveal three phases to a disrupted pattern of referrals following the onset of the pandemic: immediate drop (March to April 2020), gradual increase (May 2020 to January 2021) and accelerated increase (February to November 2021).
The immediate dramatic drop in referrals at the start of the first national lockdown reflects dental practices suddenly closing for face-to-face care and a switch to telephone consultations and advice without the benefits of clinical examination.3 Although face-to-face dental care didn't cease until 25 March 2020, there was a general awareness in dentistry and among the public of the potential issues relating to COVID-19, and this may account for the decline in referrals immediately before practice closures. Concerns in oral surgery that the early stages of the pandemic would see an increased need to manage patients with acute dental infections, including in-patients, did not materialise.7 The early introduction of the AAA approach, coupled with establishment of UDCs, are likely to have been key initiatives. For other patients, who represent the majority, the suspension of non-urgent oral surgery care would need to be delivered in the future consistent with a broad theme recognised across many areas of healthcare. Key initiatives in relation to this would include ongoing dental care and an emphasis on prevention.
The re-opening of general dental practices for face-to-face care was expected to generate a rise in referral activity and by the middle of 2020, referrals were gradually increasing, along with the capacity of oral surgery services to deliver routine care, even though both remained reduced compared to pre-pandemic levels. Mitigations to reduce the risk of transmission of COVID-19 associated with general dental and oral surgery practice were developing and represented a shift from the earliest stages of the pandemic, when oral and maxillofacial procedures were categorised as 'high-risk aerosol generating procedures'.10 Changing public attitudes to COVID-19 would also have been a factor in their willingness to seek general dental and specialist oral surgery care as the pandemic evolved.
The accelerated increase in referrals that started in early 2021 and was sustained throughout the year was dramatic, unexpected, and is likely to reflect a variety of factors. The period immediately before included the pre-Christmas 2020 national lockdown and the introduction of the national COVID-19 vaccination programme. Early in the accelerated phase, the vaccination roll-out progressed well, but there was a need for a third national lockdown. Through 2021, the vaccination programme brought a new confidence to many living in England, within an increased understanding of how to medically manage those who became unwell due to COVID-19. Patient throughput in dental practices increased, reflecting a switch from crisis measures to planned recovery.
Overall, the data demonstrate that the average referrals received per month pre-pandemic were 25,498, compared to an average of 84,953 in the period July 2020 to December 2021. This increase of 57% per month over a sustained period, with a peak 8.5-fold excess over pre-pandemic average numbers in November 2021, represents a huge and unprecedented challenge for services that are already stretched and continue to be disrupted by multiple factors. The pandemic period has been characterised by large-scale changes in referral numbers, with an average of 84,953, with referrals ranging from 10,573 in July 2020 to 217,646 in November 2021.
At the end of 2021 and the end of the study period, there is a noticeable downturn in referral numbers. It is unknown if this represents the peak of the accelerated referral phase. This coincided with identification of the rapidly transmissible COVID-19 Omicron variant11 and the implementation of restrictions, including working from home wherever possible, although face-to-face dental care continued. The seasonal holiday period and better understanding of the effectiveness and limitations of the national vaccination programme may also have been factors. Further, it is possible that issues of limited access to NHS dentistry may have resulted in some patients opting for private care to expedite the resolution of their dental problems.
To better understand the dramatic changes to referral numbers made over the study period, we investigated the numbers of referrers. On average, there were 5,871 individual healthcare professionals referring each month before the pandemic, and since the pandemic, this has reduced by 4%, to 5,399 per month. Accordingly, fewer referrers made more referrals. The reasons for this are likely to be multifactorial and may include a reduced capacity to deliver patient care within dental practices, including fewer patient treatments being delivered by each dentist and a reduction in the total number of general dental practitioners across the referral network. Other contributory factors may include delayed clinical presentations or co-morbid health issues, which mean that care needs are increasingly complex and prompt onwards referral. We have previously reported that, pre-pandemic, there was a wide variation in the number of referrals made per practitioner, with a small subset accounting for a high number of referrals.12This may also be a contributory factor but was not one investigated in this study.
The variations in oral surgery referral patterns place a huge strain on oral surgery services across England. We investigated if the increased referral numbers affected the rejection rate at clinical triage. Pre-pandemic, an average of 1.5% of referrals were rejected, but since August 2020, this has risen to 2.7%. While this has increased, it will have a minimal impact on the overall strain on oral surgery service delivery. The increased referral numbers coincide with the NHS in England setting ambitious targets to manage the backlog in routine care created by the pandemic.13
In addition to the disruption experienced by patients, there are also consequences for workforce development and how foundation, core and speciality trainees are supported to develop their skills appropriately in oral surgery.14 This data highlight the need for considered planning of workforce development to ensure that the disrupted referral patterns presented do not have a long-term destabilising impact.
The pandemic disruption had the potential to disproportionately disadvantage individuals in areas of highest deprivation. The IMD data presented confirm a disproportionate use of oral surgery services by those in lower deciles across the time periods studied. During the initial lockdown period, those with a lower IMD score (that is, more deprived) were not disproportionately disadvantaged in accessing oral surgery care, within the context of an overall reduction in numbers of referrals received. The Health Foundation6 reported that 45,187 oral surgery treatment pathways were completed in April 2019 compared to 12,989 in April 2020. They also reported that between 2019-2020, the number of completed treatment pathways fell by 9,162 per population in the most deprived areas of England, compared with a fall of 6,765 in the least deprived areas. It therefore suggests that pre-existing inequalities did have had an impact on patients' healthcare experience during the initial period of the pandemic.
Conclusion
In summary, analyses of 1.75 million referrals to oral surgery services in England have highlighted the ongoing impact of the pandemic and the need for active management to minimise the adverse impacts on patients, NHS services and the workforce. This study also demonstrates the need for the more effective use of healthcare data to inform future planning of healthcare services and in preparation for future pandemics or other disruptive events.
References
NHS England. Preparedness letter for primary dental care. 2020. Available at https://www.england.nhs.uk/coronavirus/documents/issue-7-preparedness-letter-for-primary-dental-care/ (accessed January 2023).
British Association of Maxillofacial Surgery. Guidance for the care of OMFS and Oral Surgery Patients where COVID is prevalent. 2020. Available at https://www.baoms.org.uk/_userfiles/pages/files/professionals/covid_19/baoms_omfs_general_covid19_guidance_from_baoms_final_updated.pdf (accessed January 2023).
Moore R, Keshani D, Coulthard P. UK oral surgeons' early response to the COVID-19 pandemic and impact on patient care. Oral Surg 2022; 15: 315-323.
Elsherif N, Lewney J, John J H. Impact of cancelled General Anaesthetic dental extraction appointments on children due to the COVID-19 pandemic. Community Dent Health 2021; 38: 209-214.
UK Government. The English Indices of Deprivation 2019 - FAQs. 2019. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/853811/IoD2019_FAQ_v4.pdf (accessed January 2023).
Gardener T, Fraser C. Longer waits, missing patients and catching up. The Health Foundation (London) 2021 April 13.
Politi I, McParland E, Smith R, Crummey S, Fan K. The impact of COVID-19 on cervicofacial infection of dental aetiology. Br J Oral Maxillofac Surg 2020; 58: 1029-1033.
Hammond D, Hughes F, Stirrup P, Barkworth N. Setting up and maximising the usage of an Urgent Dental Care Centre in Blackpool. Sharing our experiences. Br J Oral Maxillofac Surg 2020; 58: 834-837.
Long L, Corsar K. The COVID-19 effect: number of patients presenting to The Mid Yorkshire Hospitals OMFS team with dental infections before and during The COVID-19 outbreak. Br J Oral Maxillofac Surg 2020; 58: 713-714.
Howard B E. High-Risk Aerosol-Generating Procedures in COVID-19: Respiratory Protective Equipment Considerations. Otolaryngol Head Neck Surg 2020; 163: 98-103.
World Health Organisation. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. 2021. Available at https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed January 2023).
Moore R J, Pretty I, Douglas G, Mighell A J. An evaluation of referrer factors for 98,671 referrals made to the West Yorkshire oral surgery managed clinical network over a three-year period. Br Dent J 2022; DOI: 10.1038/s41415-022-4034-z.
NHS England. Delivery plan for tackling COVID-19 backlog of elective care. 2022. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2022/02/C1466-delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care.pdf (accessed January 2023).
Aulakh G, Wanis C, Wilson G, Moore R. The impact of COVID-19 on oral surgery training. Oral Surg 2021; 14: 313-320.
Author information
Authors and Affiliations
Contributions
Richard Moore is the main author, with equal contributions from Gail Douglas and Iain Pretty. Alan Mighell is the supervising and advisory author for the group.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval was not required as this was a service evaluation, and no patient identifiable data were included within data export, complying with the ICO guidelines on secondary use data.
Rights and permissions
About this article
Cite this article
Moore, R., Pretty, I., Douglas, G. et al. Review of 1.75 million referrals over 34 months identifies the disruptive impact of the SARS-CoV-2 pandemic on oral surgery care in England: a service evaluation. Br Dent J (2023). https://doi.org/10.1038/s41415-023-5526-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-5526-1